Contrast-induced acute kidney injury (CI-AKI) after coronary angiography or interventions is relatively frequent and portends adverse outcomes. The lack of a “universally accepted” definition, however, limits the integration and comparison of available data. We aimed to detect the CI-AKI definition that best correlates with the occurrence of clinical events at long-term in a 3-year follow-up study of patients at intermediate-to-high risk for CI-AKI. Furthermore, we sought to describe the incidence and long-term evolution of persistent renal damage (PRD) after CI-AKI and clarify the role of early (<12 hours) increments of serum creatinine (SCr) in CI-AKI prediction. Among a total of 216 patients enrolled at our center and followed for a median of 37 months, CI-AKI was diagnosed in 18.1% of cases (SCr increment ≥25% of baseline), 7.4% (SCr increment ≥0.5 mg/dl), and in 17.1% (SCr increment ≥0.3 mg/dl), according to 3 different definitions. The third definition was the only one significantly associated with the occurrence of events at 3 years (Cox regression, p = 0.04). PRD at 30 days, as detected by the same cutoff, significantly and independently identified patients at risk of worst outcomes at 3 years (p = 0.04 at multivariate Cox regression). Furthermore, a slight 5% to 10% increment of SCr compared with baseline, occurring as early as 12 hours postprocedure, was confirmed as a strong predictor of inhospital CI-AKI occurrence. In conclusion, an absolute increase in SCr ≥0.3 mg/dl seems to be most clinically informative cutoff for CI-AKI and PRD detection.
Contrast-induced acute kidney injury (CI-AKI) after coronary angiography and interventions is relatively frequent and related to adverse outcomes. At least 3 different criteria are currently used for CI-AKI diagnosis: a relative increase in serum creatinine (SCr) ≥25% from baseline values (definition 1), an absolute increase in SCr concentration ≥0.5 mg/dl (definition 2), and an absolute increase in SCr ≥0.3 mg/dl (definition 3), all presenting within 48–72 hours from contrast administration. The present study has 2 main aims: (1) to prospectively describe the clinical outcomes at a mean follow-up of 3 years in a population at intermediate-to-high risk of CI-AKI who underwent percutaneous coronary procedures and (2) to clarify which definition of CK-AKI correlates best with long-term events. Secondary aims are the description of the incidence and evolution of persistent renal damage (PRD) and its relations with long-term outcomes and to verify whether slight increments of SCr as early as 12 hours after contrast administration predict CI-AKI occurrence, as defined by the best method found.
Methods
Men and women >18 years admitted to the division of cardiology of the University of Verona for urgent or elective coronary angiography or interventional procedures, presenting risk characteristics to develop contrast-induced nephropathy, were consecutively enrolled in this prospective, observational study, in a 2-year frame.
Study protocol and inclusion and exclusion criteria have been previously reported in a short-term follow-up study, in which the predictive value of slight (5% to 10%) and early (<12 hours) increments of SCr on CI-AKI development was demonstrated. Briefly, inclusion criteria were at least one of the following: age ≥75 years, diabetes, known mild or moderate chronic kidney disease (stages 2 or 3, according to the classification of the National Kidney Foundation ), and ST-segment elevation myocardial infarction (STEMI) admitted for primary angioplasty during office hours. Patients with kidney disease in stages 4 or 5 were excluded from the study.
Renal function together with routine biochemical determinations were assessed at baseline before angiography under preventive hydration and 12, 24, 48, and 72 hours thereafter. Blood examinations were repeated also at 1 month and subsequently every 6 months up to 3 years after discharge. Kinetic Jaffè method (Dimension; Dade Behring, Deerfield, Illinois) was used for determination of SCr: the results were recalibrated to standardized creatinine measurements obtained at the Cleveland Clinic Research Laboratory. Glomerular filtration rate was estimated by the Modification of Diet in Renal Disease Study equation.
Coronary angiography was performed by either standard femoral or radial approach. In all cases either iso-osmolar (iodixanol) or low-osmolar, (iohexol) contrast media were used because of their lower nephrotoxicity. Except for the emergencies, diabetic patients discontinued metformin at least 24 hours before the procedure. Hydration was started at least 12 hours before the procedure, as in most previous clinical trials, and the infusion rate was standardized at 1 ml/kg/hour of 0.9% saline, except in cases of severe left ventricular dysfunction (ejection fraction <35%), when the infusion rate was reduced to 0.5 ml/kg/hour. Intravenous hydration was given for a minimum of 24 hours after angiography, and it was further continued if an increment of SCr compared with baseline was detected.
Each patient was visited in the outpatient clinic at 30 days after discharge and subsequently at 12-month intervals up to 3 years. The investigators also checked the blood determinations every 6 months and contacted the patients if required. The primary end point was a composite of any death, MI, or need for chronic dialytic therapy at 3-year follow-up. The study was approved by the Ethical Committee of the Azienda Ospedaliera-Universtaria di Verona, and all participating patients provided written informed consent.
Categorical data are reported as count and percentage, whereas continuous variables are presented as mean and SD if normally distributed. Chi-square statistics were used for evaluation of hierarchical events at 3 years in patients with versus without CI-AKI. Survival analyses were performed by means of Kaplan-Meier method and univariate and multivariate Cox proportional regressions. Logistic regression was used to assess the association between early SCr increments and CI-AKI onset, whereas receiver-operating characteristic curves were constructed to define sensitivity and specificity of the selected test (5% to 10% SCr variation). A multivariate Cox regression model, including demographic data and all the variables associated with a p <0.1 at univariate, was constructed to define independent predictors of 3-year events. A significance level of <5% was adopted for 2-sided statistics. All calculations were performed using Excel v.2007 (Microsoft, Redmond, California) and SPSS v.15 (IBM, New York, New York).
Results
A total of 216 patients, 71.7% men, mean age of 70 years, were prospectively evaluated in this observational study. Table 1 summarizes the main clinical and procedural features of the population. Of note, 20% of patients had baseline mild-to-moderate renal dysfunction, and 46.7% were diabetics. The main indication for coronary angiography was acute coronary syndrome (60%), namely non-STEMI (n = 47; 22%), STEMI (n = 46; 21%), and unstable angina (n = 37; 17%).
| Variable | Overall population (n=216) |
|---|---|
| Age (years), mean±SD | 71.8±10.2 |
| Men | 155 (71.7%) |
| Diabetes mellitus | 101 (46.8%) |
| Acute coronary syndrome | 161 (60%) |
| Unstable angina pectoris | 37 (17.1%) |
| Non ST-elevation Myocardial Infarction | 47 (21.8%) |
| ST-elevation Myocardial Infarction | 46 (21.3%) |
| Body Mass Index (Kg/m 2 ), mean±SD | 27.1±4.4 |
| Peripheral vascular disease | 53 (24.5%) |
| Chronic Kidney Disease mild to moderate (Glomerular Filtration Rate>30 ml/min/1,73 2 ) | 43 (19.9%) |
| Hypertension ∗ | 188 (87.7%) |
| Active Smoke | 96 (44.4%) |
| Dyslipidemia ∗ | 144 (66.7%) |
| Metabolic syndrome | 105 (48.6%) |
| Familiarity for Coronary Artery Disease | 72 (33.3%) |
| Contrast medium (ml), mean±SD | 162 ± 101 ml |
| CI-AKI def 1 (CI-AKI+/CI-AKI-/p value) | 190±147 ml/ 164±84 ml / p=0.08 |
| CI-AKI def 2 (CI-AKI+/CI-AKI-/p value) | 168±99 ml/ 162±102 / p=0.8 |
| CI-AKI def 3 (CI-AKI+/CI-AKI-/p value) | 179±132 ml/ 167±94 / p=0.1 |
| Vascular access (radial) | 83 (38.4%) |
| Procedure (interventional) | 102 (47.2%) |
∗ Hypertension is defined as a resting systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg. Dyslipidemia is defined as total cholesterol ≥200 mg/dl or triglycerides ≥150 mg/dl.
Only 18 patients received iso-osmolar contrast, with no impact on CI-AKI occurrence; patients with CI-AKI tended to receive more contrast agent than non–CI-AKI subjects, but the difference never reached significance.
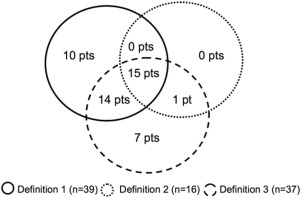
Patients were classified as developing or not CI-AKI on the basis of the already mentioned definitions: 39 patients (18.1%) developed CI-AKI based on definition 1, 16 patients (7.4%) based on definition 2, and 37 patients (17.1%) were diagnosed CI-AKI with definition 3. Figure 1 shows the details of CI-AKI diagnosis and clarifies the overlap of patients between the 3 definitions. Although basal glomerular filtration rate was 65.9 ± 26.7 ml/min in the whole population, patients with CI-AKI diagnosed with definitions 2 and 3 tended to have lower values (54 ± 21 and 58 ± 24 ml/min, respectively) than those diagnosed with definition 1 (67 ± 28 ml/min). Medical therapy at baseline and follow-up was similar for patients with and without CI-AKI, except for a trend of non–CI-AKI subjects (any definition) to receive more diuretics at baseline (53% vs 33% p = 0.07). Details for all the 3 groups of patients with CI-AKI are reported in Table 2 .
| Drug | CI-AKI DEFINITION 1 | CI-AKI DEFINITION 2 | CI-AKI DEFINITION 3 | |||
|---|---|---|---|---|---|---|
| Basal (n=39) | F/U (n=36) | Basal (n=16) | F/U (n=14) | Basal (n=37) | F/U (n=32) | |
| Beta-Blockers | 25(64%) | 21(58%) | 9(56%) | 7(50%) | 24(65%) | 18(56%) |
| ACE inhibitors/Sartans | 30(77%) | 22(61%) | 12(75%) | 9(64%) | 27(73%) | 21(63%) |
| Aspirin | 34(87%) | 23(64%) | 14(87%) | 8(57%) | 32(87%) | 20(63%) |
| Thienopiridyne | 30(77%) | 7(19%) | 12(75%) | 4(28%) | 29(78%) | 5(16%) |
| Diuretics | 18(46%) | 13(36%) | 10(62%) | 6(43%) | 17(46%) | 10(31%) |
| Statins | 24(61%) | 25(69%) | 12(75%) | 11(78%) | 25(68%) | 22(69%) |
Follow-up length had a median of 1,121 days with an interquartile range of 860 to 1,382 days. At 3-year follow-up, we observed 15 deaths (6.9%): of those, 10 (4.6%) were because of cardiovascular causes and 5 (2.3%) of other causes. Nine patients (4.2%) had myocardial infarction, whereas 7 (3.2%) experienced a major stoke. Finally, 6 subjects (2.8%) needed chronic dialytic therapy. Table 3 reports the details of the follow-up events for each of the 3 considered CI-AKI definitions. Only patients diagnosed CI-AKI by definition 3 presented a significantly higher incidence of the primary end point (any death, any MI, and need for dialysis) in respect to those who did not develop this condition (24.3% vs 11.7%; p = 0.04).
| Events | DEFINITION 1 | DEFINITION 2 | DEFINITION 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| CI/AKI- | CI/AKI+ | p | CI/AKI- | CI/AKI+ | p | CI/AKI- | CI/AKI+ | p | |
| Cadiovascular Death | 9(5.1%) | 1(2.6%) | 0.50 | 9(4.5%) | 1(6.3%) | 0.74 | 7(3.9%) | 3(8.1%) | 0.27 |
| Non Cardiovascular Death | 3(1.7%) | 2(5.1%) | 0.19 | 4(2.0%) | 1(6.3%) | 0.28 | 3(1.7%) | 2(5.4%) | 0.17 |
| Any death | 12(6.8%) | 3(7.7%) | 0.84 | 13(6.5%) | 2(12.5%) | 0.36 | 10(5.6%) | 5(13.5%) | 0.07 |
| Myocardial Infarction | 8(4.5%) | 1(2.6%) | 0.58 | 8(4.0%) | 1(6.3%) | 0.66 | 7(3.9%) | 2(5.4%) | 0.67 |
| Major Stroke | 5(2.8%) | 2(5.1%) | 0.46 | 6(3.0%) | 1(6.3%) | 0.48 | 5(2.8%) | 2(5.4%) | 0.41 |
| Dialisys | 4(2.3%) | 2(5.1%) | 0.32 | 6(3.0%) | 0(0.0%) | 0.48 | 4(2.2%) | 2(5.4%) | 0.28 |
| Recurrent Angina | 15(8.5%) | 3(7.7%) | 0.87 | 18(9.0%) | 0(0.0%) | 0.21 | 16(8.9%) | 2(5.4%) | 0.48 |
| Heart Failure | 7(4.0%) | 0(0.0%) | 0.20 | 7(3.5%) | 0(0.0%) | 0.45 | 7(3.9%) | 0(0.0%) | 0.22 |
| Composite End Point | 24(13.6%) | 6(15.4%) | 0.76 | 27(13.5%) | 3(18.8%) | 0.56 | 21(11.7%) | 9(24.3%) | 0.04 |
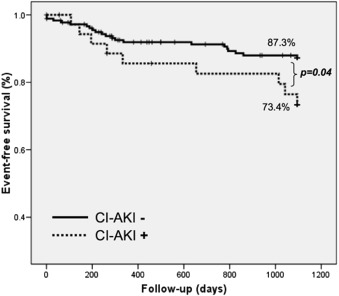
CI-AKI definitions 1 to 3 were evaluated with Cox regression models to define which one performs better for the prediction of 3-year follow-up events. Increments of at least 25% of SCr from baseline within 48 to 72 hours (definition 1) did not associate significantly with the considered events at long term (p = 0.81; hazard ratio [HR] 1.110; 95% confidence interval [CI] 0.454 to 2.717). Similarly, absolute increments of SCr of at least 0.5 mg/dl from baseline values (definition 2) did not predict 3-year outcome (p = 0.74; HR 1.224; 95% CI 0.371 to 4.037). Interestingly, there was a significant association between long-term events and CI-AKI as diagnosed by definition 3 (absolute increments from baseline SCr of at least 0.3 mg/dl within 48 to 72 h; HR 2.168; 95% CI 1.193 to 4.734, p = 0.04). At Kaplan-Meier analysis (shown in Figure 2 ), patients diagnosed with CI-AKI by definition 3 had 73.4 ± 7.6% survival free from any death, MI, or dialysis at 3 years compared with 87.3 ± 2.6% in CI-AKI–negative patients (p = 0.04 at log-rank test). These findings are summarized in Supplemental Table 1 .