Percutaneous coronary intervention (PCI) of unprotected left main disease (ULM) with drug-eluting stents (DES) is hampered by lack of information on long-term (≥10 years) safety data. All patients treated with PCI on ULM in 9 international centers with at least 10 years follow-up were enrolled. Baseline and procedural features were recorded. Repeat PCI (re-PCI) on ULM at 10 years was the primary end point. Secondary end points included major adverse cardiac events and its components (cardiac and noncardiac death, myocardial infarction, re-PCI not on ULM, and stent thrombosis). Sensitivity analysis was performed according to the presence of isolated ULM disease: 284 patients were enrolled. A total of 70 patients (21%) performed a re-PCI on ULM, 39 in the first year, and 31 between 1 and 10 years (only 5 overall performed for acute coronary syndrome). Patients with re-PCI on ULM did not show differences in baseline and procedural features, or experience higher rates of cardiovascular death (12% vs 11%, p 0.65), myocardial infarction (11% vs 6%, p 0.56), or of re-PCI on non-ULM disease (31% vs 27%, p 0.76) compared with those without re-PCI on ULM. At Kaplan–Meier analysis, patients with PCI in other coronary vessels were at higher risk of major adverse cardiac events, driven by target vessel revascularization (20.4% vs 32.9%, p 0.009), as confirmed at multivariate analysis (stenosis other than LM; hazard ratio 2, 1.4 to 2.7, all CI 95%). In conclusion, despite of using first-generation stents, PCI on ULM is safe, with low rates of recurrent events due to index revascularization. Progression of atherosclerotic lesions on other coronary vessels represents the only independent predictive factor for prognosis.
With the advent of drug-eluting stents (DES), percutaneous coronary intervention (PCI) has become widely used in the setting of unprotected left main disease (ULM) disease, offering a feasible alternative to coronary artery bypass grafting (CABG). The 5-year follow-up data from the Synergy Between PCI with Taxus and Cardiac Surgery score (SYNTAX) trial showed similar rates of major adverse cardiac events (MACE) in patients treated with PCI versus CABG for ULM, mainly due to the higher risk of stroke with surgical revascularization which offered lower rates of subsequent PCI. This led to a similar level of recommendation in European Society of Cardiology (ESC) guidelines for patients with ULM disease and low SYNTAX Score. A key recommendation of the ESC guidelines is the careful appraisal of overall risk-benefit ratio in choosing the most appropriate procedure for the individual patient, with multidisciplinary discussion between cardiac surgeons and interventional cardiologists. The consequences of long-term stent failure in the LM can be catastrophic, given the large amount of subtended myocardium at risk in case of stent restenosis or thrombosis. An assessment of the long-term outcomes after PCI versus CABG is therefore mandatory; however, there have been no published reports using data obtained from observational registries on the 10-year outcome of PCI on ULM disease. In this multicenter study, we evaluated the long-term outcomes of patients treated with PCI for ULM disease.
Methods
This study is a multicenter, nonrandomized, single-cohort retrospective study including all patients with ULM treated with DES in the 9 participating centers (Division of Cardiology, Department of Science, Città della Salute e della Scienza, Turin, Italy; Division of Cardiology, Brighton; Scientific Institute S. Raffaele, Milan, Italy; Department of Cardiology, Institut Cardiovasculaire Paris Stud, Hôpital Privé Jacques Cartier, Générale de Santé, Massy, France; Cardiovascular Institute, Hospital Clínico San Carlos, 28,040 Madrid, Spain; Servicio de Cardiología, Hospital Marqués de Valdecilla, Santander, Cantabria, Spain (J.D.L.T.); Divisione di Cardiologia, Ospedale Mauriziano, Turin, Italy; Ospedale Di Rivoli, Italy). Consecutive patients with ULM treated from 2002 onward (year in which DES became commercially available in the participating centers) to 2004 were enrolled.
Clinical data were abstracted from clinical records (electronic), whereas follow-up was performed with clinical examinations or phone calls or formal query to primary care physicians.
Angiographic data were collected after examination of coronary angiographies by at least 2 dedicated physicians: site of lesions, classifications, and elaboration of SYNTAX Score were performed according to SYNTAX criteria.
Age, gender, cardiovascular risk factors, serum creatinine, indication for PCI, and ejection fraction at discharge from hospital after ULM PCI were recorded for each patient.
For the diagnostic and interventional features of ULM disease, information on site of lesion (ostial, mid, or distal), type of technique for bifurcation disease (provisional vs 2-stent strategies), stent type, and stent diameter were recorded.
For the angiographic features on non-ULM stenosis, site of vessel and lesion were appraised. For a subgroup of patients (n = 137), SYNTAX Score was evaluated by 2 different operators at each center.
Coronary angioplasty and stent implantation during index PCI were performed according to established practice and guidelines at the time of each procedure. The choice of devices, techniques (including the approach to bifurcation stenting, kissing balloon, and postdilatation), and drug therapy (including glycoprotein IIb/IIIa inhibitors) for the index procedure was at the operating cardiologist’s discretion. After procedure, all patients were prescribed lifelong aspirin 75 mg once daily for life and clopidogrel 75 mg for 6 to 12 months or longer. The choice between angiographic and clinical follow-up was at the operator’s and referring physician’s discretion, taking into account patient preference and co-morbidities. In most cases, angiographic follow-up was recommended 6 to 12 months after the index PCI irrespective of symptoms or signs of ischemia. Treatment of restenosis was also at the operating cardiologist’s discretion but in most cases was collectively discussed, and the final management decision was based on the patient’s symptoms and/or signs of ischemia, coronary anatomy, surgical risk, feasibility of PCI, and overall life expectancy. In cases of repeat PCI, the choice of technique and device was also at the interventionist’s discretion.
Repeat PCI (re-PCI) target lesion revascularization on ULM at 10 years was the primary end point, defined as repeat revascularization for instent restenosis on ULM. MACE and its single components (cardiovascular death, myocardial infarction, and re-PCI) were secondary end points, along with re-PCI on non-ULM disease and stent thrombosis which was diagnosed and classified according to Academic Research Consortium classification. Sensitivity analyses were performed according to the presence of isolated ULM disease versus coronary stenosis in other vessels, to timing of re-PCI on ULM (<12 months vs 13 to 120 months) and according to tertiles of SYNTAX Score.
Follow-up was performed with in-hospital clinical examination, formal inquiry to primary care physicians, and patient phone interview by clinical or interventional cardiologists.
Continuous variables are expressed as mean ± SD and were compared by analysis of variance or Gossett test. Categorical variables are presented as counts and percentages and were compared by the chi-square test. The p values unadjusted for multiplicity are reported throughout, with statistical significance set at the 2-tailed 0.05 level. Kaplan–Meier analysis for MACE, myocardial infarction, and target vessel revascularization were performed, with the log-rank test. Cox multivariate analysis was performed for re-PCI on ULM with features with significant difference at univariate analysis (p <0.05) with already established clinical relevance. Statistical analyses were performed with SPSS version 21.0 (SPSS, Inc., Chicago, Illinois).
Results
A total of 284 patients were enrolled. Median follow-up was 10.2 years (range 8.2 ± 10.8). Table 1 lists relevant demographic and clinical data of the study population.
| Variable | Overall population N=284 | Patients with rePCI on LM at 10 years | P | |
|---|---|---|---|---|
| Yes N=70 | No N=214 | |||
| Age (years) | 65±9 | 66±10 | 65±9 | 0.45 |
| Women | 37 (28%) | 18 (25%) | 19 (51%) | 0.67 |
| Hypertension | 231 (75%) | 53 (77%) | 178 (71%) | 0.69 |
| Hyperlipidemia | 231 (72%) | 49 (71%) | 182 (73%) | 0.83 |
| Diabetes mellitus | 0.44 | |||
| Non insulin dependent | 96 (32%) | 24 (35%) | 72 (28%) | |
| Insulin dependent | 29 (12%) | 8 (13%) | 21 (11%) | |
| Smoker | 128 (39%) | 26 (37%) | 102 (43%) | 0.88 |
| Previous Percutaneous Coronary Intervention | 103 (31%) | 22 (32%) | 81 (33%) | 0.53 |
| Previous surgical revascularization | 102 (38%) | 28 (41%) | 74 (29%) | 0.05 |
| Creatinine on admission (md/dl) | 1.11±0.54 | 1.21±0.82 | 0.91±0.45 | 0.07 |
At 10-year follow-up, 70 patients (21%) had undergone re-PCI target lesion revascularization for ULM disease. The remaining 216 (89%) did not undergo re-PCI for ULM (see Table 1 ).
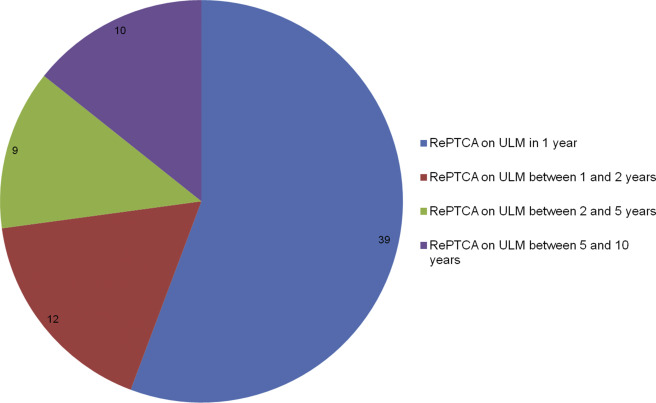
Of those patients who underwent re-PCI on ULM, the majority were performed within the first year (39 [55%]). Four (5%) of these were performed for acute coronary syndrome and the remainder performed for angiographic control which was associated with repeated PCI. Twenty-one (45%) were performed between 2 and 10 years for clinical reasons (see Figures 1 and 2 ).
Patients who underwent re-PCI on ULM did not show any differences in baseline features, apart for a trend, although not significant, for higher rates of previous surgical revascularization (41% vs 29%, p 0.05) and for higher levels of creatinine at admission (1.21 ± 0.82 vs 0.91 ± 0.45, p 0.07; see Table 1 ).
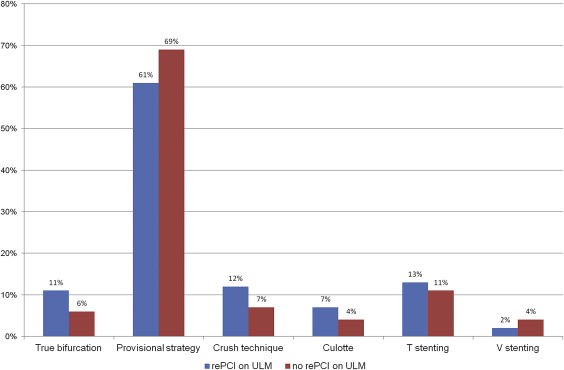
Regarding procedural features (see Table 2 ), ULM lesions were predominantly ostial (67% vs 62% p 0.54) and provisional stenting was the most frequently used strategy (61% vs 69%, p 0.48). For patients undergoing a 2-stent strategy, T-stenting and crush were the most commonly used. Sirolimus-eluting stents were used more frequently in patients undergoing re-PCI on ULM (64% vs 48%, p 0.05) without reaching statistical significance. Patients with re-PCI on ULM presented with higher rates of bifurcation disease involving both proximal left anterior descending and circumflex arteries (11% vs 6%, p 0.87). Among these, only 5 patients (20%) were treated with the provisional stenting approach.
| Variable | Overall population N=284 | Patients with rePCI on LM at 10 years | P | |
|---|---|---|---|---|
| Yes N=70 | No N=214 | |||
| Admission diagnosis | 0.84 | |||
| NSTEMI | 27 (8 %) | 4 (6%) | 23 (9%) | |
| Unstable angina | 119 (37%) | 27 (38%) | 92 (36%) | |
| Stable angina | 136 (41%) | 29 (41%) | 107 (42%) | |
| Silent ischemia | 44 (12%) | 10 (12%) | 34 (13%) | |
| Site of LM disease | 0.54 | |||
| Ostial | 205 (64%) | 46 (67%) | 159 (62%) | |
| Mid | 44 (12%) | 7 (10%) | 37 (14%) | |
| Distal | 79 (23%) | 16 (23%) | 63 (24%) | |
| IVUS | 40 (14%) | 9 (13%) | 31 (14%) | 0.46 |
| PCI: | 0.83 | |||
| LM/LAD | 195(67%) | 56 (39%) | 139 (54%) | |
| LM/CX | 99(35%) | 28 (40%) | 71 (27%) | |
| LM/ramus | 13(5%) | 3 (4%) | 10 (4%) | |
| Bifurcation: | 0.48 | |||
| Provisional | 178(63%) | 35 (61%) | 143 (69%) | |
| Crush | 27(10%) | 8 (12%) | 19 (7%) | |
| Culotte | 12(4%) | 4 (6%) | 8 (3%) | |
| T stenting | 36(13%) | 9 (13%) | 27 (11%) | |
| V stenting | 12(4%) | 1 (2%) | 11 (4%) | |
| Maximum diameter stent on LM (mm) | 3.4±0.5 | 3.6±0.5 | 3.5±0.2 | 0.78 |
| Kind of stent on LM | 0.06 | |||
| Paclitaxel Eluting Stent | 169 (49%) | 35 (26%) | 134(51%) | |
| Sirolimus Eluting Stent | 170 (51%) | 45 (64%) | 125 (48%) | |
IVUS = intravascular ultrasound.
For patients presenting with lesions on vessels other than left main stem (see Table 3 ), most presented with multivessel disease (35% vs 22%, p 0.04), with similar values of SYNTAX Score (25 ± 5 vs 23 ± 9, p 0.38) and were treated with a median of 1.2 ± 0.7 versus 1.5 ± 0.6 stents (p 0.67).
| Variable | Overall population N=284 | Patients with rePTCA on LM at 10 years | P | |
|---|---|---|---|---|
| Yes N=70 | No N=214 | |||
| Syntax score | 0.38 | |||
| Median values | 24±7 | 25±5 | 23±9 | |
| First tertile | 25 (23%) | 7 (28%) | 18 (16%) | |
| Second tertile | 43 (31%) | 7 (28%) | 36 (32%) | |
| Third tertile | 69 (43%) | 11 (44%) | 58 (43%) | |
| Number of narrowed coronary arteries other than LM | 0.04 | |||
| 1 | 104 (34%) | 27 (38%) | 77 (28%) | |
| 2 | 62 (22%) | 15 (21%) | 47 (17%) | |
| 3 | 21 (9%) | 7 (14%) | 14 (5%) | |
| Ejection fraction at discharge (%) | 53±8 | 53±9 | 52±7 | 0.69 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


