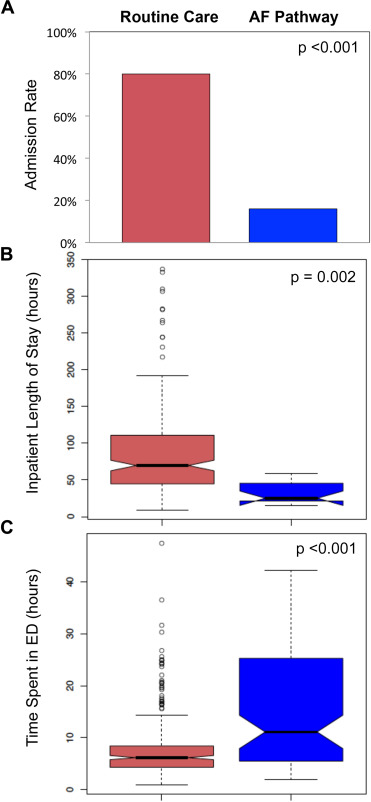
Management of atrial fibrillation (AF) in the emergency department (ED) is variable because of the absence of universally adopted treatment guidelines. To address potentially preventable hospital admissions and prolonged length of stay, an AF treatment pathway was co-developed by physicians from the cardiac electrophysiology service and the department of emergency medicine at our institution. The impact of this AF pathway on patient outcomes was evaluated with a prospective, observational study conducted in a single tertiary care center from July 1, 2013, to June 30, 2014. The primary study outcome was the rate of hospital admission. The secondary outcomes were duration of ED visit and inpatient length of stay. The 94 patients treated according to the AF pathway during the study period were less likely to be admitted than the 265 patients who received routine care (16% vs 80%, p <0.001). For admitted patients, the mean length of stay was shorter for patients treated according to the AF pathway (32 vs 85 hours, p = 0.002). The time spent in the ED was longer for patients in the AF pathway (16 vs 85 hours, p <0.001). Utilization of a multidisciplinary pathway for management of AF in the ED led to a significant reduction in the rate of hospital admission. Patients who were admitted after receiving care according to the AF pathway had a shorter length of stay. In conclusion, utilization of a multidisciplinary AF pathway resulted in a 5-fold reduction in admission rate and >2-fold reduction length of stay for admitted patients.
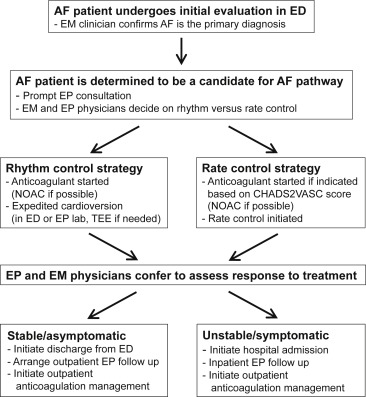
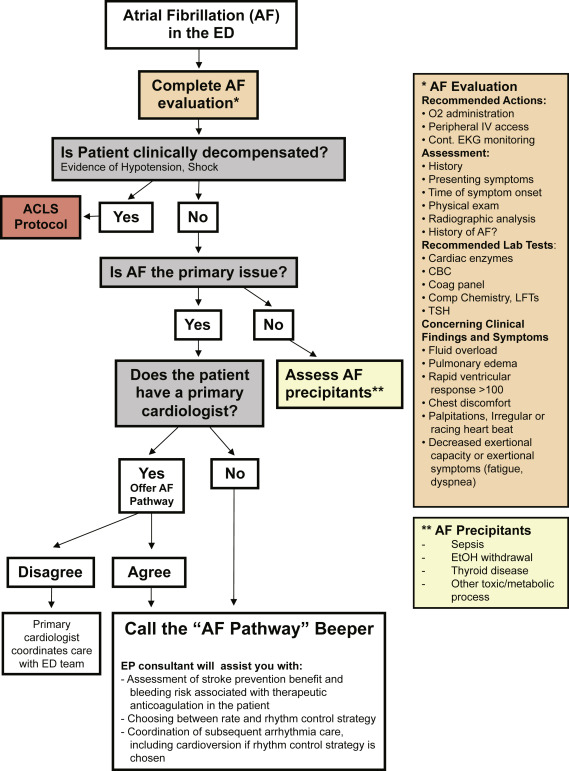
Hospitalization is the primary cost driver for atrial fibrillation (AF) management. Hospital admissions due to AF have increased several fold in recent years and currently exceed 460,000 per year in the United States. A study of the US National Hospital Ambulatory Medical Care Survey from 1993 to 2004 revealed that 64% of the emergency department (ED) visits for AF resulted in hospital admission. During this period, the proportion of ED visits for AF that led to admission remained stable, resulting in an increase in the absolute number of admissions. Many AF-related hospitalizations can be avoided. There is a growing body of evidence that a revised paradigm for management of AF in the ED, including cardioversion followed by a brief observation period and discharge, is a safe and feasible alternative to inpatient management for appropriately selected patients. Implementation of this strategy could lead to decreased hospital admission rates and reduced utilization of health care resources ; however, studies describing this approach are comparatively small, and the guidelines that address the management of AF specifically in the ED setting are not as well validated as other aspects of AF management. Consequently, there is considerable variability among specialists with regard to management of AF in the ED. To improve the consistency with which available AF treatment guidelines are applied in the ED at our institution, we created an AF treatment pathway that is based on structured collaboration between emergency medicine (EM) and cardiac electrophysiology (EP) clinicians ( Figures 1 and 2 ). The purpose of this study was to test the hypothesis that a multidisciplinary AF treatment pathway could reduce hospital admission rates and length of inpatient stay.
Methods
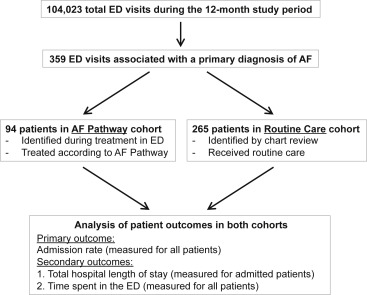
The multidisciplinary AF treatment pathway, summarized in Figure 1 , was approved by participating EM and EP physicians and the authors’ institutional review board before the start of the study. The impact of this AF treatment pathway on patient outcomes was evaluated with a prospective, observational study that was performed during a 1-year period (July 1, 2013, to June 30, 2014) in the ED of a single tertiary care center. Selection of study cohorts is summarized in Figure 3 . Patients included in the AF pathway cohort included adult patients who presented to the ED with AF as the primary diagnosis and received treatment according to the AF pathway. Patients in the routine care cohort included adult patients who presented to the ED with a primary diagnosis of AF who were not treated according to the AF pathway and instead received routine care. The decision to treat patients according to the AF pathway versus routine care was at the discretion of the ED physicians. Some ED physicians did not use the AF pathway. Patients in the routine care cohort were identified by chart review using the Partners Research Patient Data Repository. Patients in the routine care group were defined as being patients for whom AF was listed as the primary diagnosis ( International Classification of Diseases, Ninth Revision , code) in the ED attending physician note, physician inpatient admission note, or physician discharge summary. All patient data were captured from the patients’ electronic medical records using a standard electronic report form. The primary study end point was hospital admission. Rate of hospital admission was measured and compared for both the AF pathway and routine care cohorts. The secondary end points were ED length of stay and total length of stay for admitted patients (defined as the length of the ED stay plus the inpatient stay). Baseline characteristics of patients in both cohorts are presented using descriptive statistics with mean and SD for continuous variables and counts or percentages for categorical variables. Baseline characteristics of the patient groups were compared using a 2-tailed Student t test for continuous variables and the Pearson chi-square test for categorical variables.
The relations between AF pathway utilization and hospital admission rate were examined using multivariate logistic regression. We fit models adjusted for (1) demographic factors (age, gender); (2) demographic factors plus co-morbid conditions (e.g., hypertension, heart failure, and valvular heart disease); and (3) demographic factors, co-morbid conditions, plus acute cardiac biomarker elevation (N-terminal pro B-type natriuretic peptide [NT-proBNP], troponin T) measured at the time of ED presentation. In models that included biomarkers, the values were log-transformed before inclusion. Models adjusted for NT-proBNP and troponin T were considered exploratory as these biomarkers were not measured in all subjects. In secondary analyses, we examined the relations between AF pathway utilization and total length of stay using multiple linear regression. Duration of ED visit was calculated for all patients irrespective of admission status. We fit models adjusted for the same covariates as outlined previously for analyses of hospital admission.
To minimize potential confounding, we also assessed the relations between AF pathway utilization and outcomes in propensity-matched analyses. Specifically, propensity scores were computed for each subject by regressing patient group assignment (AF pathway or routine care) on age, gender, and co-morbid conditions as outlined previously using multivariate logistic regression. Each patient in the AF pathway cohort was matched to the closest control patient in the routine care cohort using a nearest neighbor matching technique.
A second study author who was blinded to the study results collected data from a random sample of patients for verification of internal validity. Two separate interrater reliability (IRR) analyses were performed. First, Cohen κ coefficient was calculated to assess IRR for determination of whether patients presenting to the ED during the specified study period had AF as their primary diagnosis. Second, Pearson correlation coefficient was used to calculate IRR for duration of ED stay (performed for patients in both study cohorts). For all statistical analyses performed, a 2-sided p value <0.05 was considered significant. Analyses were performed by using R version 3.1.1. Propensity score matching was performed using the MatchIt package.
Results
The baseline characteristics of the study groups were as follows. During the 12-month study period, 359 patients presented to the ED at our institution with a primary diagnosis of AF. Of these patients, 94 were treated according to the AF pathway and were therefore included in the AF pathway cohort ( Figure 3 ). Chart review was performed to identify the 265 patients in the routine care cohort, who qualified for treatment according to the AF pathway but received routine care instead. Baseline characteristics of the 2 study cohorts are listed in Tables 1 and 2 . Comparison of the 2 cohorts revealed significant differences in age and gender. No significant differences in the incidence of the included comorbidities were observed.
| Characteristics | AF Pathway (N = 94) | Prematch | Postmatch | ||
|---|---|---|---|---|---|
| Routine Care (N = 265) | P value | Routine Care (N = 94) | P value | ||
| Age, mean (SD) | 59.9 (13.3) | 69.9 (13.6) | <0.001 | 60.6 (13) | 0.708 |
| Male | 68% | 56% | 0.038 | 70% | 0.875 |
| Female | 32% | 44% | 0.038 | 30% | 0.875 |
| Hypertension | 55% | 66% | 0.064 | 53% | 0.884 |
| Congestive heart failure | 13% | 18% | 0.260 | 15% | 0.833 |
| Valve disease | 7% | 10% | 0.490 | 9% | 1 |
| Cerebrovascular disease | 3% | 9% | 0.077 | 1% | 0.621 |
| Peripheral arterial disease | 4% | 6% | 0.520 | 2% | 0.682 |
| Coronary artery disease | 13% | 20% | 0.140 | 11% | 0.821 |
| Prior myocardial infarction | 2% | 4% | 0.370 | 1% | 1 |
| Diabetes mellitus | 12% | 13% | 0.858 | 11% | 1 |
| Hyperlipidemia | 29% | 38% | 0.120 | 25% | 0.621 |
| Lung disease | 10% | 10% | 0.950 | 9% | 1 |
| Chronic kidney disease | 4% | 6% | 0.448 | 4% | 1 |
| CHA 2 DS 2 VASc score, mean (SD) | 1.6 (0.8) | 2.9 (1.7) | <0.001 | 1.8 (1.5) | 0.314 |
| HAS-BLED score, mean (SD) | 0.8 (0.8) | 1.2 (0.8) | <0.001 | 0.8 (0.8) | 0.853 |
| No prior history of AF | 59% | 48% | 0.077 | 50% | 0.242 |
| Prior AF, paroxysmal | 35% | 40% | 0.439 | 37% | 0.761 |
| Prior AF, persistent | 6% | 12% | 0.123 | 12% | 0.204 |
| Presenting symptoms ∗ | AF Pathway (N = 94) | Prematch | Postmatch | ||
|---|---|---|---|---|---|
| Routine Care (N = 265) | P value | Routine Care (N = 94) | P value | ||
| Palpitations | 77% | 36% | <0.001 | 46% | <0.001 |
| Dyspnea/Fatigue | 42% | 24% | 0.402 | 34% | 0.292 |
| Chest discomfort | 20% | 17% | 0.479 | 24% | 0.385 |
| Lightheadedness | 33% | 17% | <0.001 | 18% | 0.019 |
| Asymptomatic | 5% | 10% | 0.183 | 10% | 0.266 |
∗ Some patients reported more than one symptom at initial presentation.
Utilization of the AF pathway reduced the rate of hospital admission. During the study period, the admission rate for patients who received routine care was 80%, compared with 16% for patients treated according to the AF pathway ( Figure 4 ). Multivariate logistic regression was performed to further examine relations between AF pathway utilization and hospital admissions. Use of the AF pathway was associated with a significant reduction in hospital admission, compared with routine care, despite adjustment for demographic and clinical covariates ( Table 3 ). Although patients with a primary clinical diagnosis of decompensated heart failure or acute coronary syndrome were excluded from this study, in exploratory analyses performed in the subset of subjects with measured NT-proBNP and troponin levels in the ED, use of the AF pathway remained significantly associated with reduced hospital admission ( Table 3 ).
| Risk of hospital admission | |||
|---|---|---|---|
| Model | No. AF pathway / No. routine care | AF pathway OR (95% CI) | P value |
| Overall sample | |||
| Age, gender | 94 / 265 | 0.05 (0.02-0.10) | <0.001 |
| Multivariable ∗ | 94 / 265 | 0.05 (0.02-0.09) | <0.001 |
| Multivariable ∗ + NT-proBNP + Troponin T † | 36 / 163 | 0.03 (0.01-0.09) | <0.001 |
| Propensity matched subset | |||
| Univariable ‡ | 94 / 94 | 0.05 (0.02-0.10) | <0.001 |
| Multivariable ‡ , § | 94 / 94 | 0.04 (0.02-0.09) | <0.001 |
| Multivariable ¶ , § + NT-proBNP + Troponin T † | 36 / 36 | 0.04 (0.01-0.18) | <0.001 |
| Length of hospitalization (ED stay + inpatient stay) in patients admitted from the ED | |||
|---|---|---|---|
| Model | No. | AF pathway β (standard error), hours | P value |
| Age, gender | 226 | -43.5 (16.7) | 0.01 |
| Multivariable ∗ | 226 | -36.4 (16.9) | 0.03 |
| Multivariable ∗ + NT-proBNP + Troponin T † | 155 | -25.0 (23.4) | 0.33 |
| Length of ED stay | |||
|---|---|---|---|
| Model | No. | AF pathway β (standard error), hours | P value |
| Age, gender | 359 | 7.8 (1.0) | <0.001 |
| Multivariable ∗ | 359 | 7.8 (1.0) | <0.001 |
| Multivariable ∗ + NT-proBNP + Troponin T † | 177 | 6.6 (1.4) | <0.001 |
∗ Age + gender + hypertension + congestive heart failure + valve disease + cerebrovascular disease + peripheral arterial disease + coronary artery disease + prior myocardial infarction + diabetes mellitus + hyperlipidemia + lung disease + chronic kidney disease.
† BNP and troponin are natural log transformed; troponin values of <0.01 assumed to be 0.001 for modeling purposes.
‡ Matching based on age + gender + hypertension + congestive heart failure + valve disease + cerebrovascular disease + peripheral arterial disease + coronary artery disease + prior myocardial infarction + diabetes mellitus + hyperlipidemia + lung disease + chronic kidney disease.
§ Multivariable model includes age + gender + hypertension + congestive heart failure + valve disease + cerebrovascular disease + peripheral arterial disease + coronary artery disease + prior myocardial infarction + diabetes mellitus + hyperlipidemia + lung disease + chronic kidney disease.
¶ Matching based on age + gender + hypertension + congestive heart failure + valve disease + cerebrovascular disease + peripheral arterial disease + coronary artery disease + prior myocardial infarction + diabetes mellitus + hyperlipidemia + lung disease + chronic kidney disease + ln(NT-proBNP) + ln(Troponin T).
To minimize potential for residual confounding in this observational study, we also examined associations in a subset of subjects defined by propensity score matching for AF pathway utilization. A nearest-neighbor matching approach was used to maximize the number of subjects exposed to the AF pathway included in the analysis. This approach yielded a subset of the routine care cohort for which there were no significant differences in age, gender, and co-morbid conditions compared with the AF pathway cohort ( Tables 1 and 2 ). After multivariate regression in the propensity-matched cohort, utilization of the AF pathway remained associated with reduced admission rate ( Table 3 ). In sensitivity analyses in which patients were grouped into tertiles of propensity to be treated according to the AF pathway, the magnitude of effect associated with the AF pathway remained similar to that in the overall sample (odds ratio range 0.01 to 0.06, p <0.001 for each analysis). In the subset of subjects with measured NT-proBNP and troponin levels, no substantive difference was observed in the magnitude of effect associated with AF pathway utilization after adjustment for these biomarkers in exploratory analyses ( Table 3 ). Patients who were admitted after receiving treatment according to the AF pathway in the ED were found to have shorter hospital stays (mean 32 hours) than patients admitted after receiving routine care in the ED (mean 85 hours, p = 0.002; Figure 4 ). In multivariate-adjusted models, the AF pathway was associated with significantly reduced admission length of stay. After adjustment for age, gender, and medical co-morbidities, the AF pathway was associated with a reduction in length of stay of 36 hours ( Table 3 ). In the subset of subjects in which biomarkers were measured, no significant difference was observed after adjustment for these factors.
Utilization of the AF pathway was associated with prolongation of the ED stay. Duration of the ED stay was calculated for all patients in both cohorts, including patients who were admitted to inpatient units after ED treatment and patients who were discharged directly from the ED. Patients treated according to the AF pathway remained in the ED longer (mean 16 hours) than patients who received routine care (mean 8 hours; Figure 4 ). Multivariate-adjusted models that correct for age, gender, and medical co-morbidities demonstrated that patients in the AF pathway spent 8 hours longer in the ED than routine care patients ( Table 3 ). A significant prolongation of the ED stay (7 hours) was also observed in the subset of patients in the AF pathway in whom biomarkers were measured.
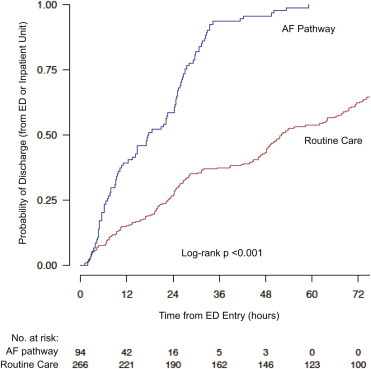
AF pathway utilization increased the overall probability of discharge. Time from initial ED presentation to hospital discharge was calculated for all patients in both study cohorts, irrespective of admission status. A Kaplan–Meier estimate of discharge probability revealed that utilization of the AF pathway increased the overall probability of hospital discharge ( Figure 5 ).