Patients with non–ST elevation myocardial infarction who are managed noninvasively at presentation or are catheterized but without revascularization represent a heterogeneous and understudied population. We evaluated the clinical characteristics, management strategies, and outcomes of patients with non–ST elevation myocardial infarction (NSTEMI) who were enrolled in the prospective biannual Acute Coronary Syndrome Israeli Surveys from 2004 to 2013. Patients were divided into 3 groups: no catheterization (no angio), catheterization with revascularization (angio-revascularized), and catheterization without revascularization (angio-nonrevascularized) groups. The study included 3,198 patients with NSTEMI. Coronary angiography was performed in 2,525 (79%) during the index hospitalization, of whom 1899 (59%) underwent revascularization. Evidence-based therapies were administered during the index hospitalization at a significantly higher rate to those in the angio-revascularized group compared with the other 2 groups. Multivariate analysis showed that compared with those in the angio-revascularized and angio-nonrevascularized groups, patients in the no angio group experienced a significantly higher risk for 1-year mortality (hazard ratio 2.04 [p ≤0.0001] and 1.21 [p = 0.01], respectively). The risk associated with no revascularized was consistent in each risk subset analyzed, including an older age, and increased creatinine levels. In conclusion, our data, from a large real-world contemporary experience, suggest that patients with NSTEMI who do not undergo coronary revascularization during the index hospitalization represent a greater risk and undertreated group with increased risk for long-term mortality.
In patients with non–ST elevation myocardial infarction (NSTEMI) with moderate to high risk characteristics, current guidelines recommend an invasive strategy with angiography followed by percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) if appropriate. In clinical practice, 27% to 48% and 45% to 69% of this patient population do not undergo catheterization and revascularization procedures respectively. Several studies have highlighted the higher morbidity and mortality rates for such patients. These findings suggest that this is a high-risk population, yet these patients are undertreated with evidence-based therapies. Patients with NSTEMI who are managed without revascularization represent a heterogeneous and understudied population. Furthermore, currently, there are limited data regarding the clinical characteristics and outcomes of patients with NSTEMI who do not undergo coronary revascularization during the index event in a contemporary real-world setting. In this study, we evaluated the clinical characteristics, medical management, and outcomes of patients with NSTEMI who were enrolled in the prospective Israeli Acute Coronary Syndrome Israeli surveys (ACSIS). Patients were categorized as those who were managed medically without intervention, compared with those who were managed with an invasive strategy, with or without revascularization.
Methods
The ACSIS is a national survey conducted in Israel since 1992. Details of these nationwide registries have been previously reported. Briefly, ACSIS is conducted during a period of 2 months, once in 2 years. Data are prospectively collected from all patients discharged with any diagnosis corresponding to the acute coronary syndrome (ACS) spectrum in each of the 25 coronary care units and cardiology wards operating in Israel. Demographic and clinical data are recorded on prespecified forms for all these patients. The discharge diagnoses are recorded as determined by the attending physicians based on clinical, electrocardiographic, and biochemical criteria. In-hospital and 30-day outcome data are ascertained by hospital chart review, telephone contact, and clinical follow-up data. Patient management is at the discretion of the attending physicians. Mortality data during hospitalization and at 30 days and 1 year after hospitalization are determined for all patients from hospital charts and by matching identification numbers of patients with the Israeli National Population Register. All parameters captured by the registry are defined by protocol.
The population of the present study comprises patients included in ACSIS surveys from the years 2004 to 2013, who were admitted with NSTEMI, that is, clinical picture of ACS without STEMI and increase of cardiac biomarkers, principally troponin. Patients with STEMI and patients with an increase in cardiac biomarkers whose predominant clinical picture was not of an ACS (i.e., heart failure, sepsis, pulmonary embolism, arrhythmias) were not included. For this analysis, patients were categorized as who were treated conservatively only without coronary angiography (“no angio group”). The angio group was further classified by patients who underwent revascularization, percutaneously or bypass graft operation (“angio-revascularized group”), and those who did not undergo intervention (“angio-nonrevascularized group”). Patients admitted with STEMI or discharged as unstable angina were not included in the current analysis. Major adverse cardiac events (MACE) at 30 days were defined by the composite outcome of death, unstable angina, and reinfarction.
Characteristics of study participants were compared using the chi-square test for categorical variables and the Student t test or Wilcoxon rank tests, as appropriate for continuous variables. The Kruskal–Wallis test was used for comparison of nonnormally distributed continuous variables. The probability of all-cause mortality during 30-day and 1-year interval was graphically displayed using the Kaplan–Meier method. Cox proportional hazards multivariate-adjusted survival models were used to evaluate the independent effects of treatment groups on 7 days, 30-day and 1-year all-cause mortality results presented as hazard ratio (HR) and CI 95%. Logistic regression was used to evaluate the association between treatment group and MACE. All multivariate models were further adjusted for the additional prespecified covariates: gender, age, hypertension, diabetes mellitus, dyslipidemia, chronic kidney disease, current smoking, a family history of coronary artery disease (CAD), electrocardiogram at arrival, coronary artery disease, previous MI, a history of heart failure, past PCI, past CABG, stroke, and peripheral vascular disease.
Results
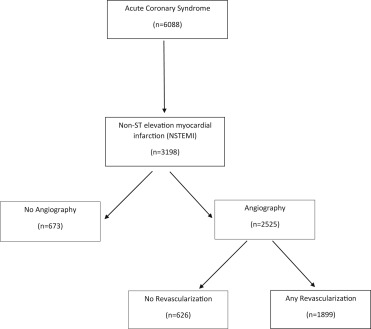
A total of 6,088 patients were included in the last 5 ACSIS. A total of 3,198 patients (54%) were admitted with a diagnosis of NSTEMI ( Figure 1 ). Among the 3,198 study patients with an admission diagnosis of NSTEMI, coronary angiography was performed in 2,525 patients (79%) during the index hospitalization, of whom, 1,899 (59%) underwent a revascularization intervention. The baseline clinical characteristics of study patients are presented in Table 1 . Compared with the angio groups, patients in the no angio group was significantly older and with higher rates of baseline clinical risk factors, known coronary artery disease, chronic heart failure, symptomatic noncardiac atherosclerosis, and lower mean hemoglobin level. Accordingly were prescribed higher rates of cardiovascular medications before admission.
| Variable | No-Angio (n=673) | Angio-No -Revasc (n= 626) | Angio-Revasc (n=1899) | p |
|---|---|---|---|---|
| Age (years) (mean ±SD) | 71. 98 ± 12.9 | 64.02± 12.4 | 63.69 ± 12.2 | < 0.001 |
| Women | 30.9 | 26.6 | 20.3 | < 0.001 |
| Body Mass Index (kg/m 2 ) (mean +SD) | 28.72 ± 8.0 | 29.18± 17.8 | 28.69 ± 13.61 | 0.01 |
| Weight (kg) (mean ±SD) | 77.1 ± 15.7 | 79.9 ± 16.9 | 80.9 ± 15.6 | <0.001 |
| Diabetes Mellitus | 50.9 % | 42.1 % | 36.5 % | <0.001 |
| Hypertension | 78.5 % | 68.4 % | 64.3 % | <0.001 |
| Dyslipidemia | 68.0 % | 72.5 % | 74.1 % | 0.08 |
| Family history of Coronary Artery Disease | 15.8 % | 24.5 % | 28.2 % | <0.001 |
| Current Smoker | 21.0 % | 33.5 % | 36.6 % | <0.001 |
| Prior Myocardical Infarction | 48.8 % | 37.7 % | 30.0 % | <0.001 |
| Prior Percutaneous Coronary Intervention | 38.3 % | 34.3 % | 32.8% | 0.033 |
| Prior Coronary Arterial By-Pass Grafts | 22.8 % | 13.2 % | 11.2 % | <0.001 |
| Chronic heart failure | 25.3 % | 8.3 % | 7.7 % | <0.001 |
| Chronic Kidney Disease | 34.8 % | 15.3 % | 10.2 % | <0.001 |
| Past Cerebro-Vascular Accident | 15.5 % | 9.8 % | 7.5 % | <0.001 |
| Peripheral Vascular Disease | 18.6 % | 10.4 % | 7.9 % | <0.001 |
| Aspirin | 61.9 % | 55.6 % | 52.0 % | <0.001 |
| Oral anticoagulants | 10.5 % | 4.6 % | 3.7 % | <0.001 |
| Beta blockers | 55.9 % | 41.3 % | 40.3 % | <0.001 |
| Nitrates | 24.6 % | 11.6 % | 10.0 % | <0.001 |
| Diuretics | 38.1 % | 23.6 % | 18.3 % | <0.001 |
| Angiotensin-Converting-Enzyme Inhibitor / Angiotensin Receptor Blocker | 54.3 % | 46.8 % | 40.2 % | <0.001 |
| Statins | 55.9 % | 53.0 % | 50.7 % | 0.05 |
| Insulin | 14.8 % | 10.4 % | 7.4 % | <0.001 |
| Anti-hyperglycemic drugs | 29.9 % | 28.2 % | 24.2 % | <0.01 |
| Creatinine (mg%) (mean ±SD) | 2.03 ± 7.47 | 1.2± 0.88 | 1.39 ± 4.7 | <0.001 |
| Glomerular Filtration Rate (ml/min) (mean ±SD) | 57.2 ± 66 | 78.1±76 | 87.0 ± 309.3 | <0.001 |
| Hemoglobin (g/dL ) (mean ±SD) | 12.2 ± 2.2 | 13.4± 1.8 | 13.8 ± 3.6 | <0.001 |
| Creatine Phosphokinase (IU) (mean ±SD) | 500.9 ± 1161 | 373.7± 481 | 432.7 ± 623 | <0.001 |
| Glucose (mg%) (mean ±SD) | 174 ± 90 | 153 ± 81 | 146 ± 74 | 0.001 |
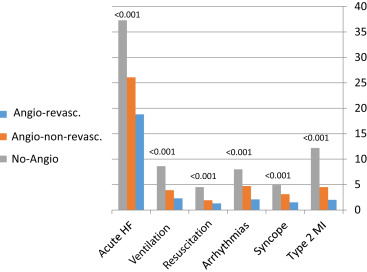
Patients who underwent coronary angiography (with or without intervention) were more likely to present with typical angina (70%) as compared with those in the no angio group (51%; p <0.001) but had significant lower frequency of high-risk admission clinical features ( Figure 2 ). Hospital management of the study patients by the revascularization strategy is summarized in Table 2 . The overall revascularization rate was 60%. Among patients who underwent coronary revascularization, 92% were treated with PCI and 8% underwent CABG. During hospital stay, the medical management of ACS was more closely followed per guidelines in the angio groups, as reflected in the higher rate of dual antiplatelet treatment, Angiotensin converting enzyme inhibitors/Angiotensin receptor blockers, and statins administration than for the no angio group. Drugs to relieve heart failure or angina symptoms, such as nitrates, furosemide, and digoxin, were given significantly more frequently in the no angio group. Consistent with those findings, rates of all cardiovascular and other in-hospital complications were statistically higher in the no angio group, as illustrated in Figure 3 .
| Variable | No-Angio (n=673) | Angio-No-Revasc (n= 626) | Angio-Revasc (n=1899) | p |
|---|---|---|---|---|
| Coronary arterial by-pass grafts | 0 | 0 | 8.8 % | <0.001 |
| Percutaneous coronary intervention | 0 | 0 | 92.2 % | <0.001 |
| Aspirin | 90 % | 96.2 % | 98.4 % | <0.001 |
| Clopidogrel | 61.8 % | 73.6 % | 88.1 % | <0.001 |
| Beta blockers | 81.7 % | 84.3 % | 84.0 % | 0.335 |
| Angiotensin-converting-enzyme inhibitor / Angiotensin receptor blocker | 70.4 % | 74.5 % | 79.3 % | <0.001 |
| Statins | 79.1 % | 91.7 % | 93.3 % | <0.001 |
| Digoxin | 5.5 % | 1.4 % | 1.1 % | <0.001 |
| Diuretic | 53.4 % | 31.2 % | 24.5 % | <0.001 |
| Nitrates | 34.4 % | 28.2 % | 23.9 % | <0.001 |
| Oral Anticoagulants | 7.4 % | 4.4 % | 3.3 % | <0.001 |
| Hospital duration (days) | 7.1 ± 6.3 | 6.8 ± 6.2 | 5.8 ± 5.1 | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


