In 2007, the Texas legislature appropriated money for a pilot study to evaluate cardiovascular screening of student athletes to identify those who might be at risk of sudden death using a questionnaire, physical examination, electrocardiography, and limited echocardiography. We sought to determine (1) the feasibility of a state-wide cardiovascular screening program, (2) the ability to reliably identify at-risk subjects, and (3) problems in implementing screening state wide. The data were analyzed using established pediatric electrocardiographic and echocardiographic criteria. Positive results were confirmed by a blinded reviewer. In 31 venues (2,506 students), the electrocardiographic findings met the criteria for cardiovascular disease in 57 (2.3%), with 33 changes suggestive of hypertrophic cardiomyopathy, 14 with long QT syndrome, 7 with Wolff–Parkinson–White syndrome, and 3 with potential ischemic findings related to a coronary anomaly. Of the 2,051 echocardiograms, 11 had findings concerning for disease (9 with hypertrophic cardiomyopathy and 1 with dilated cardiomyopathy). In patients with electrocardiographic findings consistent with hypertrophic cardiomyopathy, the limited echocardiograms were normal in 24 of 33. Of the 33 who remained at risk of sudden death on the electrocardiogram or echocardiogram, 25 (65.8%) pursued the recommended evaluation, which confirmed long QT syndrome in 4, Wolff–Parkinson–White syndrome in 7, and dilated cardiomyopathy in 1. The interobserver agreement was 100% for electrocardiography and 79% for echocardiography. The questionnaire identified 895 (35% of the total) potentially at-risk students, with disease confirmed in 11 (1.23%). In conclusion, in this large state-funded project, electrocardiographic and echocardiographic screening identified 11 of 2,506 patients potentially at risk of cardiovascular disease. The questionnaire was of limited value and had a large number of false-positive results. Interobserver variation was significant for echocardiography and might create problems with limited echocardiographic screening. Finally, many subjects with abnormal screening results declined a follow-up evaluation.
Considerable national interest is being focused on developing more effective preparticipation screening programs to identify those student athletes who might be at risk of sudden death (SD). The challenge in developing such a screening process is that one must take into account the extraordinary number of young athletes and the infrequency of SD. The purpose of the present study was to analyze the results of statewide screening of young athletes for undiagnosed causes of SD. The factors analyzed included technical and operational limitations in both the performance and the coordination of such a program, appropriate identification of screen-positive subjects, and the ability to perform all aspects of the screening in a timely and cost-effective manner.
Methods
In 2007, the Texas State legislature approved Senate Bill 7, relating to the placement of automated external defibrillators in schools statewide. Section 38.109 of this bill allocated 1 million dollars for the Texas Education Agency to “establish a pilot program under which students are administered cardiovascular screening, including an electrocardiogram and an echocardiogram.” To implement this screening program, a collaborative group of investigators was formed with regional centers in Dallas, Austin, and Houston. The University of Texas Southwestern Medical School and Baylor College of Medicine institutional review boards approved the study. Student athletes from grades 6 to 12 were enrolled from 34 schools in the Dallas area, 27 schools in the Austin area, and 10 schools in the Houston area. The inclusion criteria required all students to (1) participate in either school and/or recreational sport teams, (2) complete the screening questionnaire (in accordance with the 12 currently recommended American College of Cardiology/American Heart Association screening guidelines), and (3) provide informed consent and student assent. Those with pre-existing cardiovascular conditions were excluded from the present study.
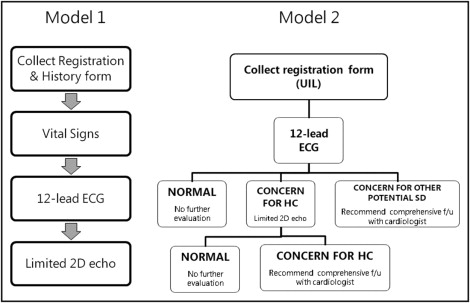
Students underwent screening according to 1 of 2 models, depending on their location. In both models, students underwent 12-lead electrocardiography ( Figure 1 ). In model 1, all students underwent limited 2-dimensional echocardiography, and then the electrocardiograms (ECGs) and echocardiograms were reviewed off-site. In model 2, the 12-lead ECG was interpreted by an on-site pediatric electrophysiologist. If concern was present for cardiomyopathy, the student underwent a limited echocardiographic study. A screen-positive ECG or echocardiogram specifically referred to the identification of the potential risk of having disease abnormalities that could result in a future life-threatening event, thereby prompting a referral to a pediatric cardiologist for additional evaluation.
Previously established screening electrocardiographic criteria ( Table 1 ) were used to identify those at risk of SD. In this athletic population, an electrocardiographic diagnosis of left ventricular hypertrophy was made using recent modifications described by Corrado et al, including increased QRS voltage in the precordial leads associated with additional nonvoltage criteria such as left atrial enlargement, left axis deviation, ST-segment and T-wave abnormalities, and pathologic Q waves. The ECGs were visually assessed for the presence of Wolff–Parkinson–White (WPW) pattern. All borderline QT values were measured manually in lead II or V 5 , and the corrected QT interval was calculated using Bazett’s formula. Athletes with corrected QT values of ≥450 ms were referred for a comprehensive assessment. All ECGs were interpreted by board-certified pediatric cardiologists with a specialty in electrophysiology. If an ECG was screen positive (i.e., hypertrophic cardiomyopathy [HC], long QT [LQT] syndrome, WPW), the students were advised not to participate in competitive athletics and to be examined by a pediatric cardiologist. Incidental findings on the ECG were recorded but not considered screen positive. These findings included PACs/ PVCs and incomplete right bundle branch block.
| Rate <40 or >125 beats/min | Ventricular premature complexes ≥3 per 6-second tracing |
| QRS axis >120° (right-axis deviation) | Ventricular couplets/triplets |
| QRS axis ≤30° (left-axis deviation) | Any supraventricular tachycardia |
| Right atrial enlargement, left atrial enlargement | ST-T wave abnormality in ≥2 leads ⁎ |
| QRS >120 ms (right bundle branch block, left bundle branch block, or interventricular conduction delay) | Abnormal Q wave (>0.04 s or >3 mm deep in ≥2 leads) |
| First-degree atrioventricular block >200 ms | Corrected QT interval >450 ms |
| Second- or third-degree atrioventricular block | QS pattern in ≥2 precordial leads |
| “Brugada pattern” in lead V 1 | Modified left ventricular hypertrophy criteria † |
| Wolff–Parkinson–White syndrome | Poor R wave progression |
⁎ ST-T wave abnormality included primarily inverted T waves but also >2-mm ST-segment depression; isolated T-wave inversion in lead aVR or lead V 1 was not considered abnormal.
† Modified left ventricular hypertrophy criteria included increased precordial voltage (>3 mV) plus increased limb lead voltage as determined by the standards of Davignon or increased precordial lead voltage (>3 mV) accompanied by ST-T–wave abnormalities, prominent Q waves, extreme left-axis deviation (≥30°), or findings of left atrial enlargement.
The limited screening echocardiogram was a focused 2-dimensional study to assess for the presence of HC using standard criteria recommendations from the American Society of Echocardiography ( Table 2 ). Apical and parasternal views were obtained, and the left ventricular (LV) end-diastolic, LV end-systolic, interventricular septal dimension in diastole, LV posterior wall end-diastolic dimension, LV ejection fraction, and LV shortening fraction were measured. Where appropriate, the measurements were adjusted according to the body surface area. Students whose results were screen positive were not given sports clearance and were referred for directed, standard care by a pediatric cardiologist. Students with an incidental, nonlife-threatening abnormality appreciated on the echocardiographic screen, including atrial septal defect, bicuspid aortic valve, and mitral valve prolapse, were not excluded from participation but were directed to follow-up with a pediatric cardiologist.
| Variable | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|
| Reference Range | Mildly Abnormal | Moderately Abnormal | Severely Abnormal | Reference Range | Mildly Abnormal | Moderately Abnormal | Severely Abnormal | |
| Left ventricular mass (g) | 67–162 | 163–186 | 187–210 | ≥211 | 88–224 | 225–258 | 259–292 | ≥293 |
| Left ventricular mass/body surface area (g/m 2 ) | 43–95 | 96–108 | 109–121 | ≥122 | 49–115 | 116–131 | 132–148 | ≥149 |
| Ventricular septal thickness (cm) | 0.6–0.9 | 1.0–1.2 | 1.3–1.5 | ≥1.6 | 0.6–1.0 | 1.1–1.3 | 1.4–1.6 | ≥1.6 |
| Left ventricular posterior wall thickness (cm) | 0.6–0.9 | 1.0–1.2 | 1.3–1.5 | ≥1.6 | 0.6–1.0 | 1.1–1.3 | 1.4–1.6 | ≥1.6 |
In model 1, all results were communicated, at a later date, verbally and by a letter to the parents. In model 2, the students received a report at the screening venue. Abnormal screen results were also communicated at a later date, both verbally and in writing, to the parents.
Three facilities in Dallas, Austin, and Houston performed the initial electrocardiographic and echocardiographic interpretation. Each facility had board-certified pediatric cardiologists with expertise in electrophysiology conduct the electrocardiographic analysis. Pediatric cardiologists with expertise in echocardiography and an Intersocietal Commission for the Accreditation of Echocardiographic Laboratories designation were responsible for the echocardiographic interpretation. To control for interobserver variability, all positive results were sent to 1 of the other 2 facilities for blinded validation. Also, 10% of all normal results were sent to a second facility for blinded validation. In cases in which disease was suspected by the primary facility but considered normal by the review facility, the records were sent in a blinded fashion to an independent institution for interpretation of the results.
This was a prospective, nonrandomized, observational study. The demographic data are presented as mean ± SD. With respect to the cost analysis, the expenses reported are related to the screening process only.
Results
A total of 28 events were present for model 1, averaging 72.2 students/event. On average, the ECGs were interpreted 82.5 days after the screening venue, the echocardiograms were read 28.6 days after the venue, and the study results were mailed to the participants 89.5 days after the venue. In model 2, 3 events occurred, averaging 161.3 students/venue. In this latter model, the screening results were provided immediately to the participant.
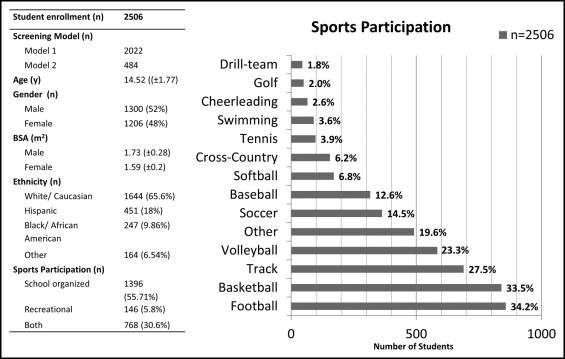
A total of 2,506 students were enrolled, with 2,022 screened according to model 1 and 484 according to model 2 ( Figure 2 ). The average age was 14.5 ± 1.77 years, 1,300 subjects were boys (52%), and the mean body surface area was 1.73 m 2 . Most students were white (65.6%), followed by Hispanics and blacks.
A total of 550 subjects (21.9%) reported ≥1 cardiovascular symptom with exercise, with 178 (32.4%) of 550 reporting >1 symptom. Most (78%) reported no concerning cardiovascular family history. Approximately 14% reported a family history of either an “abnormal heart rhythm” or an “enlarged/thickened heart.” Of note, 33 students specifically mentioned a potentially hereditable familial condition: HC in 15, Marfan syndrome in 9, LQT syndrome in 3, ventricular fibrillation in 3, and SD in 4.
Of the 2,506 ECGs performed, 57 (2.3%) were screen positive: 33 showed LV hypertrophy, 14 a prolonged QT interval, 7 WPW pattern, and 3 abnormal Q waves and repolarization abnormalities, concerning for potential CA abnormalities ( Figure 3 ). There was 100% agreement for electrocardiographic interpretation among the screening and reviewing electrophysiologists regarding the identification of a screen-positive ECG using the predetermined, written electrocardiographic criteria. Of those students with concern for HC from the screening ECG, 24 of 33 had normal screening echocardiograms. Of those remaining, 9 continued to have concern after the screening echocardiogram and were referred for additional follow-up. However, only 3 pursed the recommendation and were ultimately found to have a no definitive evidence of HC. Of those with a prolonged QT interval, 13 of 14 pursued additional follow-up and 4 were subsequently diagnosed by cardiologists not involved with the present study with LQT syndrome and a β-blocker medication was initiated. No genetic testing has been performed to confirm the diagnosis. Of the 7 subjects with WPW, 4 pursued follow-up and eventually underwent an ablation procedure, and 2 were lost to follow-up. The remaining patient with WPW was subsequently diagnosed with dilated cardiomyopathy as well and is currently in the care of a pediatric cardiologist. Finally, of the 3 students with electrocardiographic findings suspicious for having a CA abnormality, only 1 chose to pursue follow-up and was found to have normal coronary artery anatomy. Thus, from the ECG screen alone, 11 of 57 subjects (0.4% of the total population screened) were ultimately diagnosed with concern for disease after a comprehensive evaluation by a pediatric cardiologist.

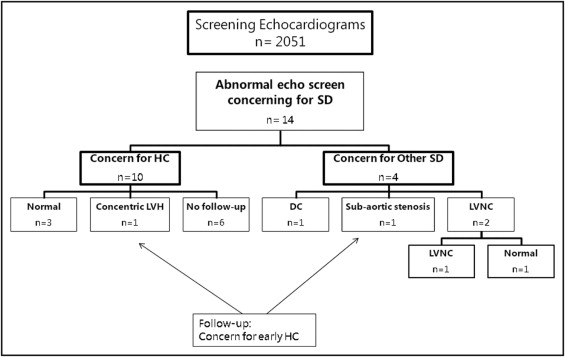
A total of 2,051 screening echocardiograms were performed ( Figure 4 ), of which 14 (0.7% of the population screened) were initially considered screen positive. Of these, 10 had concern for HC, 2 for LV noncompaction (LVNC), 1 for dilated cardiomyopathy, and 1 for subaortic stenosis. Of these, 8 subjects (57%) pursued follow-up and the following pathologic entity was diagnosed: dilated cardiomyopathy in 1, LVNC in 1, and early HC in 2, both of whom are being followed up conservatively and have been restricted from athletics by the primary cardiologist. On blinded review for validation purposes, neither the 1 case of LVNC nor the 2 cases of early HC met the criteria for disease diagnosis by either the review facility or the outside independent institution and, therefore, were not considered true screen-positive studies.