Left Mainstem Intervention
Michael Lee MD
Gopi Manthripragada MD
GUIDELINES
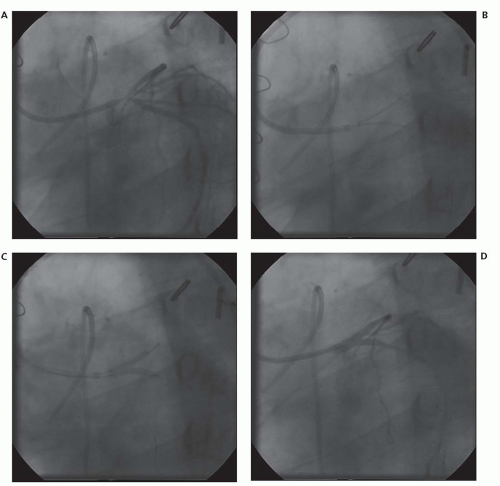
The left main artery is the most critical segment of the coronary vascular bed because it perfuses approximately 60% to 70% of the myocardium. Since the advent of percutaneous coronary intervention (PCI) as a revascularization technique for obstructive coronary disease, the procedure of choice for unprotected left main coronary artery (ULMCA) disease has been coronary artery bypass grafting (CABG) (1). The American College of Cardiology/American Heart Association/Society of Cardiovascular Angiography and Intervention (ACC/AHA/SCAI) 2005 Guideline Update states that PCI for ULMCA was a Class III indication, Level of Evidence C (based on expert opinion) (2). This paradigm has changed over the years, with the recognition that the primary disadvantage of PCI in most studies was a higher rate of repeat revascularization compared with CABG but no difference in mortality between the two techniques up to 3 years (3, 4). Advances in procedural technique, stent design, and patient selection have made PCI a reasonable alternative in select groups of ULMCA disease patients (5). The 2011 ACCF/AHA/SCAI Guidelines for PCI and CABG support PCI in patients with favorable anatomic conditions (isolated ostial and shaft disease, and the absence of multivessel disease), low risk of PCI-related complications and/or clinical conditions that would portend a high surgical risk (Class IIA, Level of Evidence B) (Fig. 25-1) (6).
PREPROCEDURAL CONSIDERATIONS
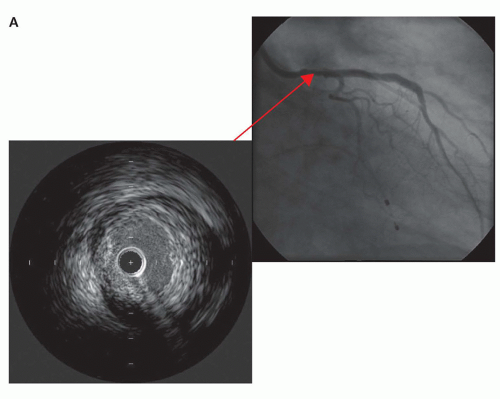
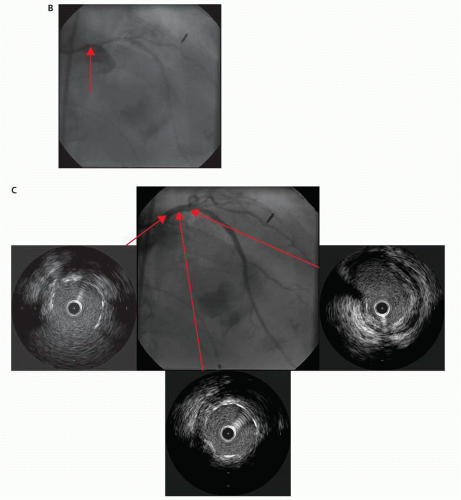
The proper selection of patients is critical to procedural success, particularly with ULMCA PCI. Owing to the large area of myocardium at risk, both clinical and anatomical considerations need to be taken into account when deciding the optimal revascularization strategy for a given patient (7). Low-risk clinical predictors include younger age, preserved left ventricular and renal function, and an elective, as opposed to an urgent or emergent, procedure. Low-risk anatomical predictors include isolated ostial or shaft disease and the absence of multivessel disease (8). Distal bifurcation lesions are almost always associated with disease within the left anterior descending, circumflex, or both on pathologic and intravascular ultrasound (IVUS) studies, with the carina usually being disease free (9). Because of the involvement of the bifurcation, and sometimes trifurcation, at the distal left main, PCI is associated with significantly higher rates of repeat revascularization and overall major adverse cardiac events (MACE) compared with ostial or shaft lesions (Fig. 25-2) (10, 11).
The Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX) Trial was a large, multicenter trial with 1,800 patients, with either three-vessel or ULMCA disease randomized to PCI with the first-generation paclitaxel-eluting stents or CABG. For all these patients, a Heart Team, comprising a cardiac surgeon and an interventional cardiologist, concluded that equivalent anatomic revascularization could be attained with either approach.
Preprocedure characteristics were similar (12). At 1 year, the rate of revascularization was significantly higher in the PCI group (13.5% vs. 5.9%), while the stroke rate was higher in the surgical group (2.2% vs. 0.6%).
Preprocedure characteristics were similar (12). At 1 year, the rate of revascularization was significantly higher in the PCI group (13.5% vs. 5.9%), while the stroke rate was higher in the surgical group (2.2% vs. 0.6%).
Owing to the variation in risk based on clinical and anatomic factors, predictive models have been developed to help determine the optimal mode of revascularization for the individual patient. They include clinical, angiographic, or procedural variables with some including a combination of all three. The SYNTAX score divides patients into tertiles of low, medium, and high risk based on an angiographic score (13). Outcomes between CABG and PCI in ULMCA disease for low- (SYNTAX score 0-22) and medium-(23, 24, 25, 26, 27, 28, 29, 30, 31 and 32) risk patients show clinical equipoise, with outcomes in high-risk (>32) patients favoring CABG (13, 14). MACE rates increase with the number of vessels intervened upon during PCI, with the most recent guidelines giving ULMCA PCI in intermediate risk score patients a IIA indication (6). The New Risk Stratification (NERS) model was created to improve upon the angiographic features used in the SYNTAX score by including clinical and procedural variables as well. The sensitivity and specificity of a NERS
score ≥25 were 92.0% and 74.1% for MACE compared with 70.5% and 35.2% for high-risk SYNTAX patients in a consecutive left main registry (15).
score ≥25 were 92.0% and 74.1% for MACE compared with 70.5% and 35.2% for high-risk SYNTAX patients in a consecutive left main registry (15).
The Revascularization for ULMCA Stenosis: Comparison of Percutaneous Coronary Angioplasty versus Surgical Revascularization (MAIN-COMPARE) study was a prospective, nonrandomized observational study of 2,240 patients with ULMCA disease, with 51% undergoing CABG and 49% undergoing PCI. 71% of those undergoing PCI received drug-eluting stents (DES). At a median follow-up of 5.2 years, no difference in death or myocardial infarction was noted between the two groups. The hazard ratio for target vessel revascularization compared with CABG was 6.69 for DES compared with 7.97 for bare metal stents (BMS). Further, half the patients in the PCI arm of the study had PCI of the distal ULMCA, which is associated with higher MACE rates than PCI of the mid-body or ostial left main. Proper patient selection can thus lower target lesion revascularization rates further with the use of DES.
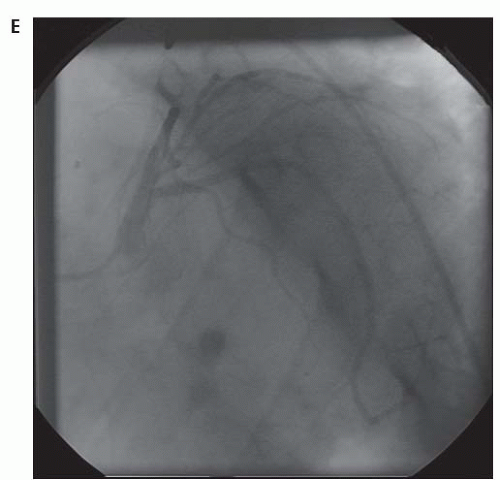
PROCEDURAL STRATEGIES AND TECHNIQUE
Discussion with patients regarding the optimal approach for ULMCA revascularization must include a thorough assessment of their candidacy for dual antiplatelet therapy (DAPT). Furthermore, since ULMCA restenosis would jeopardize a vast myocardial territory, and target lesion revascularization is the Achilles heel of ULMCA PCI when compared with CABG, DES should be the default stent choice (16, 17




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree