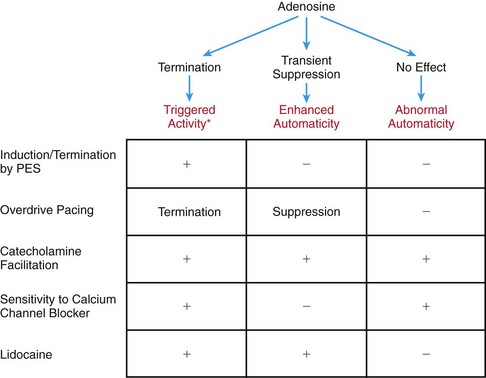
79 As indicated earlier, the most challenging differential diagnosis is between JET and AVNRT, as the two arrhythmias present with similar HV intervals recorded during tachycardia and sinus rhythm. Each arrhythmia may also be associated with VA block.1 Several maneuvers can help to differentiate JT from AV node reentry but require the presence of VA conduction. Atrial overdrive pacing yields an A-H-H-A response in JET because of the focal nature of this tachycardia; the maneuver yields an A-H-A response in AVNRT because entrainment proceeds via the same anterograde limb as the reentry circuit (Figure 79-1).2 Another useful maneuver involves the introduction of premature atrial complexes (PACs) during tachycardia. A late-coupled PAC delivered during His-refractoriness does not affect JET but can preexcite or delay the subsequent ventricular beat in AVNRT by engaging the anterograde slow AV nodal pathway (Figure 79-2, A, B). An early-coupled PAC that captures the His and ventricle usually allows JET to continue but should terminate AVNRT because it conducts anterogradely down the fast pathway (Figure 79-2, C, D).3 Figure 79-1 Atrial Overdrive Pacing to Differentiate Junctional Tachycardia (JT) from Atrioventricular Nodal Reentrant Tachycardia (AVNRT) Figure 79-2 Premature Atrial Complex (PAC) Response to Differentiate Junctional Tachycardia (JT) from Atrioventricular Nodal Reentrant Tachycardia (AVNRT) There is a dearth of data regarding the electrophysiological mechanism of junctional ectopic tachycardia. Given the lack of dependence on a critical coupling interval for tachycardia initiation, the often irregular tachycardia rate, and inability to entrain the arrhythmia, the electrophysiological behavior of JET is consistent with a focal non-reentrant arrhythmia. With regard to cellular mechanisms, most published case series of JET have postulated that enhanced automaticity is responsible for the arrhythmia.4–6 However, recent evidence suggests that at least two other mechanisms may be responsible for cases of JET: abnormal automaticity and triggered activity.7 In contrast with enhanced automaticity, tissue with abnormal automaticity generally does not demonstrate overdrive suppression because of its reduced resting membrane potential (typically ≤−60 mV) and the inactivated state of the sodium current and the electrogenic sodium pump. Abnormal automaticity is then dependent on the slow inward calcium current and is therefore sensitive to inhibition of this current by calcium channel blockers.8 Adenosine has no effect on abnormal automaticity, whereas it transiently suppresses enhanced normal automaticity (Figure 79-3).9 Therefore, sensitivity of an automatic tachycardia to calcium channel blockade as well as insensitivity to adenosine is consistent with abnormal automaticity rather than enhanced “normal” automaticity (Figure 79-4).
Junctional Tachycardia
Differentiation During Electrophysiological Study
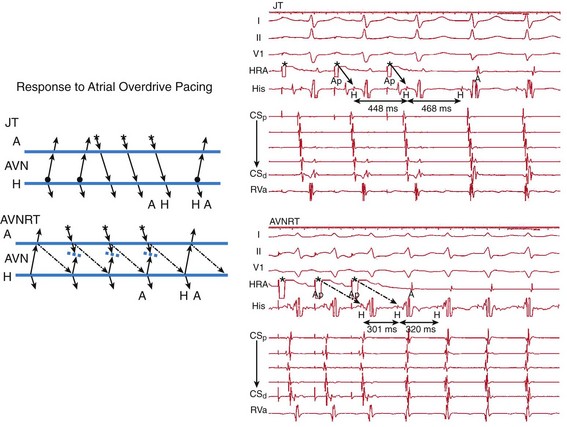
Left side, Ladder diagrams illustrating response to atrial overdrive pacing. Top, During JT, the earliest return signal is an H followed by an A, resulting in an AHHA response. Bottom, During AVNRT, the earliest return signal is an A, resulting in an AHA response. Star represents atrial pace. Solid arrows represent conduction through the atrium, fast AV nodal pathway, and His. Interrupted arrows represent conduction through the slow AV nodal pathway. A, Atrium; AVN, atrioventricular node; H, His. Right side, Intracardiac electrograms. Top, During JT, tachycardia cycle length is 468 ms. Atrial overdrive pacing is performed at 448 ms. After cessation of pacing, an AHHA response is observed. Solid arrows represent conduction down the fast AV nodal pathway. Bottom, During AVNRT, tachycardia cycle length is 320 ms. Atrial overdrive pacing is performed at 300 ms. After cessation of pacing, an AHA response is observed. Interrupted arrows represent slow pathway conduction. Ap, Atrial pace; CS, coronary sinus; HRA, high right atrium; RVa, right ventricular apex. (From Fan R, Tardos JG, Almasry I, et al: Novel use of atrial overdrive pacing to rapidly differentiate junctional tachycardia from atrioventricular nodal reentrant tachycardia. Heart Rhythm 8:840-844, 2011.)
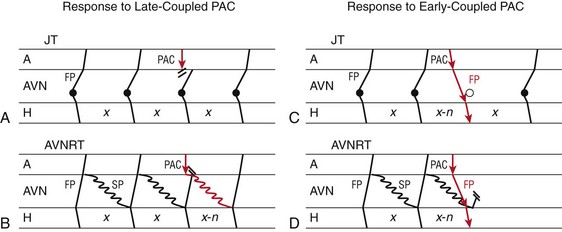
Left, Response to PAC delivered when junction is refractory (local atrial activation from PAC occurs at or after His activation). A, During JT, a PAC delivered at a time the junction focus has already depolarized blocks at the AV node (AVN) and is unable to influence the immediate or the next junction beat. Solid circles represent junction focus. Black lines show conduction through AVN, His (H), and atrium (A). B, During AVNRT, a similarly timed PAC can influence the next beat of AVNRT by early engagement of the slow pathway. Black lines show conduction through AVN, His (H), and atrium (A), and red lines show PAC and its response. Although this figure shows advancement of the next beat (x-n), delay of the next beat or termination of tachycardia is also specific to AVNRT. Red arrow indicates PAC and its response. FP, Fast AV nodal pathway; SP, slow AV nodal pathway; x and x-n, H-H intervals. Right, Response to earlier-coupled PACs. C, During JT, an early PAC advances the immediate JT beat, and His timing by AV nodal fast pathway activation and JT continues. Open circle represents the anticipated JT beat timing if no PAC is delivered. D, During AVNRT, an early PAC may advance the immediate His by activation of the AV nodal fast pathway. However, this makes the fast pathway refractory and unavailable for retrograde conduction, thus terminating the AVNRT circuit. (From Padanilam BJ, Manfredi JA, Steinberg LA, et al: Differentiating junctional tachycardia and atrioventricular node re-entry tachycardia based on response to atrial extrastimulus pacing. J Am Coll Cardiol 52:1711-1717, 2008.)
Mechanisms
Junctional Tachycardia