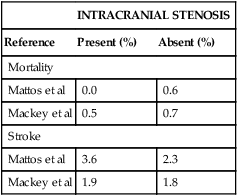
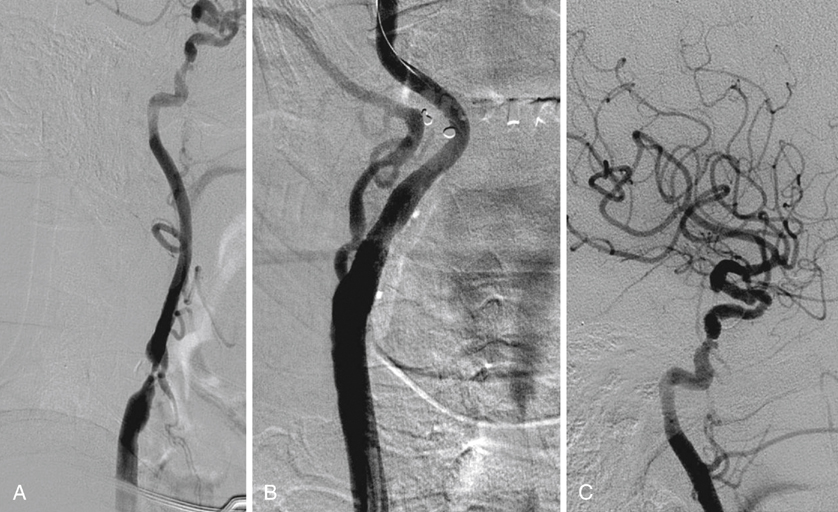
Perioperative (30 day) stroke and death rates are not statistically significantly increased in CEA patients with intracranial occlusive lesions (Table 1). In a subgroup of patients with more than 50% siphon stenosis, Mattos and coworkers found a perioperative stroke rate of 1 in 19 (5.3%), which was not statistically significantly different from the stroke rate noted in patients without siphon disease or with mild (20%–49%) siphon lesions. This is similar to the findings of Schuler and associates, who noted perioperative stroke rate of 7.1% in patients with more than 50% ipsilateral siphon stenosis. In addition, they found a stroke rate of 2 in 18 (11.1%) in patients undergoing endarterectomy in whom the siphon stenosis exceeded the bifurcation stenosis. Although this was greater than the perioperative stroke risk (4.1%) noted in patients with normal or less severely diseased siphons, the difference was not statistically significant. TABLE 1 Perioperative Mortality and Stroke Risk Data from Mackey WC, O’Donnell TF Jr, Callow AD: Carotid endarterectomy in patients with intracranial vascular disease: short-term risk and long-term outcome, J Vasc Surg 10:432–438, 1989; Mattos MA, van Bemmelen PS, Hodgson KJ: The influence of carotid siphon stenosis on short- and long-term outcome after carotid endarterectomy, J Vasc Surg 17:902-910; discussion 910–911, 1993. Because intracranial occlusive lesions have only minor effects on perioperative mortality or stroke risk or on long-term stroke-free rates, most patients with appropriate carotid bifurcation pathology and intracranial occlusive lesions are acceptable candidates for CEA or CAS. Thus a symptomatic patient with a compelling bifurcation lesion and a smooth intracranial stenosis (Figure 1A) may subsequently undergo CAS or CEA (Figure 1B and C). The presence of mild to moderate intracranial occlusive disease in this setting should not influence a decision to intervene.
Intracranial Occlusive Disease and Aneurysms
Influence on Carotid Revascularization Outcomes
Intracranial Occlusive Disease
INTRACRANIAL STENOSIS
Reference
Present (%)
Absent (%)
Mortality
Mattos et al
0.0
0.6
Mackey et al
0.5
0.7
Stroke
Mattos et al
3.6
2.3
Mackey et al
1.9
1.8
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine
