The advancing field of percutaneous endovascular therapy has led to a significant increase in options available for the treatment of patients with symptomatic peripheral vascular disease. Previous reticence in applying these techniques to the infrapo-pliteal arterial bed is slowly giving way, as technological improvements and operator experience have led to predictable and consistently high rates of technical success with low risk of complications.
INDICATIONS FOR INTERVENTION
Critical limb ischemia (CLI), manifest as ischemic rest pain or tissue loss, is the most common clinical indication for infrapopliteal intervention, and presents a significant risk for amputation in that individual (1). In the elderly, who are most at risk, the probability of loss of independence and reduced quality of life from an amputation is significant (2). Currently it appears that whatever treatment successfully prevents major amputation will be cost-effective, with benefit to the individual as well as society (3). In most instances of CLI, the risk-benefit ratio is different from that seen with the claudicant; because of the risk of limb threat in patients with CLI, there is a significantly lower threshold in performing endovascular and surgical procedures of greater complexity (and greater risk). There is also a greater acceptance in performing procedures of more limited durability, since in most circumstances, restenosis following complete wound healing is often clinically silent. The latter observation is based on the fact that the tissue in patients with nonhealing ulcers, or gangrene, requires high levels of oxygen and nutrition for tissue repair. This level of oxygenation is usually only adequately supplied by uninterrupted, straight-line arterial flow by at least one of the tibial vessels (i.e., with an intact pedal arch). However, once wound healing has occurred, the oxygen requirements to maintain tissue integrity are significantly decreased. Thus, if vascular occlusion or rest-enosis occurs after wound healing, most patients will maintain integrity of the tissue and function satisfactorily. Long-term healing will be particularly successful if patients are instructed in proper foot care, and in the avoidance of foot trauma and infection.
The therapeutic decision process for the treatment of infrapopliteal disease is complex, whether the treatment is medical, surgical, or endovascular. Considerations include such limb variables as the level and degree of tissue destruction, the presence of associated soft tissue or bony infection, and the need for debridement or skin grafting. General patient variables that play a significant role in the decision process include the presence of comorbidities such as cardiopulmonary disease, diabetes and renal insufficiency, the functional and ambulatory status of the patient, and the availability of appropriate vein conduit for surgical revascularization. Anatomic variables such as the distribution, burden, and nature of athereosclerosis in the lower extremities are important in assessing the likely technical success of revascularization. It should be recognized that the primary goal of treatment of significant distal limb ischemia is not necessarily hemodynamic but is that of safe avoidance of amputation and salvage of a functioning limb.
Historically, reconstructive femoral-to-tibial bypass surgery using venous conduit has been successful in preserving limb viability. However, in the absence of adequate venous conduit, results were universally dismal. Recent availability of heparin-bonded bypass conduit appears to be offering some improved results (4). Further larger studies will be required to confirm these initial data. In the interim, there is a general reluctance to use prosthetic grafts to bypass the tibial vessels (5,6). Even when appropriate vein conduit is available, there remain significant issues with distal bypass surgery. Although individual centers may give excellent results, similar results may not be possible in many centers, when audited (7). The problem of postoperative wound infection, necessitating weeks of intensive care, occurs commonly (i.e., 10% to 30%) but is rarely mentioned (8). Interestingly, as seen in distal angioplasty, the patency rates of surgical-bypass grafts may lag behind the limb salvage rates. Similar to restenosis following percutaneous procedures, graft closure after wound healing may not always lead to significant ischemia (9).
The published experience for endovascular intervention of the infrapopliteal arteries began with the advent of balloon angioplasty, but even today, it is still limited. In contrast to early data, current reports have documented endovascular revascularization to be highly efficacious with very low risk (10,11). Widespread application is still debated, primarily on the basis of poor long-term, hemodynamic outcome and lack of comparative trials (12,13). However, the use of endovascular techniques continues to grow rapidly because these procedures are repeatable, may be accomplished quickly, and are safely completed in patients with multiple comorbidities. Whereas restenosis is a major consideration for endovascular procedures performed above the knee (i.e., performed usually for claudication), it should not be a major limiting factor in below-the-knee intervention (i.e., performed usually for limb salvage).
Most of the literature evaluating infrapopliteal endovascular techniques has been reported from studies with populations with limb-threatening ischemia. It should be noted that except in diabetics, limb threat is usually produced by multilevel vascular obstruction. Even though this may be treated traditionally by surgical revascularization, it has been the authors’ experience that multilevel, endovascular intervention may treat these patients successfully (14). There are also those who advocate that distal intervention should be used to extend the durability of femoral-popliteal angioplasty (15).
ANATOMY
The popliteal artery typically divides below the level of the knee joint into the anterior tibial artery and tibioperoneal trunk. This “bifurcation” is often erroneously referred to as the “tibial trifurcation.” The anterior tibial artery courses laterally and anteriorly to penetrate the interosseous membrane, giving off branches to the surrounding muscles, and also small branches that penetrate the membrane to help supply the deep muscles of the posterior side of the leg (Fig. 17.1). It descends in the anterior compartment of the leg, and as it crosses the ankle joint, it becomes the dorsalis pedis artery. In about 3.5% of limbs, the anterior tibial artery either fails to reach the foot or is reduced to a very slender vessel.
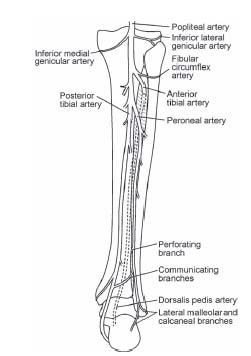
Figure 17.1 • Diagram of the arteries of the leg. Posterior view.
The tibioperoneal trunk, a segment of vessel of variable length, gives rise to the peroneal and posterior tibial arteries, which are both located in the posterior compartment of the leg. The posterior tibial artery continues downward on the tibialis posterior muscle along the medial aspect of the leg. When it reaches the plantar surface of the foot, it terminates, as the medial and lateral plantar branches. Typically, the lateral plantar branch is larger than the medial plantar branch, is located inferior to the medial plantar branch, and provides the major contribution to the metatarsal arch. The peroneal artery passes laterally, across the surface of the tibialis posterior muscle, to lie between the interosseous membrane and the fibula. The peroneal artery gives off branches that pass through the interosseous membrane to help supply the anterior calf muscles. Variation in the anatomy of the tibial vessels is seen in ~ 10% of individuals (Fig. 17.2) (16). The most common variants include hypoplastic or aplastic posterior tibial, hypoplastic or aplastic anterior tibial artery, true trifurcation of the popliteal artery, and high origin of the anterior tibial artery. An awareness of these variants is important in the interpretation of angiographic findings.
ACCESS
Access from the contralateral common femoral artery is used to approach most infrapopliteal stenotic disease. A 5- to 6-Fr. crossover sheath may be placed into the ipsilateral, distal external iliac artery from the contralateral common femoral artery (Fig. 17.3A). Infrapopliteal intervention may be performed with these short, crossover sheaths as guides, but this may make intervention somewhat cumbersome, owing to the distance of the crossover sheath tip to the infrapopliteal location. In addition, more contrast will be needed to opacify the distal circulation adequately. To maximize control, a 6-Fr. multipurpose, coronary guide catheter may be advanced through the crossover sheath to the ipsilateral, distal, superficial femoral artery, or midpopliteal artery (Fig. 17.3B). This 6-Fr. coronary guide catheter will then allow for most intervention modalities to be used. Alternatively, long, flexible, hydrophilic 5- to 6-Fr. guide sheaths have recently been introduced, which may be advanced from the contralateral, common femoral artery to the distal ipsilateral superficial femoral artery (SFA) or midpopliteal artery, to allow for similar control.
Antegrade access from the ipsilateral, common femoral artery is preferred to treat complex infrapopliteal occlusions or severe diffuse disease (Fig. 17.3C). The advantage of an ipsilateral antegrade femoral approach is that it decreases the overall distance guidewires have to be manipulated during attempts to cross complex stenotic disease or total occlusions. This approach also allows the treatment of distal tibial disease that can be problematic using the contralateral approach due to limitations in the length of delivery systems for a variety of interventional tools. Similarly, the antegrade approach allows the operator to deal with distal embolization to the plantar and dorsalis pedis vessels, which is often not possible from the contralateral approach. The 5- to 6-Fr. flexible sheaths of variable lengths (typically 11 to 30 cm) may be placed into the superficial femoral or proximal popliteal artery, using fluoroscopic guidance. Unfortunately, patients with a large abdominal girth may often not be approached in an antegrade fashion. Alternatively in patients with acceptable superficial femoral arteries, an antegrade sheath may be placed with ultrasound guidance into the proximal SFA. Theoretically, this may decrease the risk of access complications such as retroperitoneal bleeding.
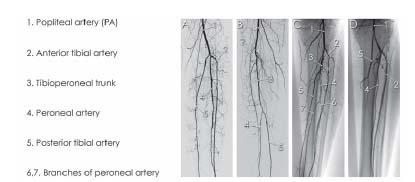
Figure 17.2 • Examples of variant angiographic anatomy of the tibial vessels. A: True trifurcation of the popliteal artery. B: Long tibioperoneal trunk. C: Bifurcation of the peroneal artery. D: Absent tibioperoneal trunk, with origin of the posterior tibial artery as the first branch of the popliteal artery, followed by the peroneal artery and anterior tibial artery. (1) Popliteal artery. (2) Anterior tibial artery. (3) Tibioperoneal trunk. (4) Peroneal artery. (5) Posterior tibial artery. (6,7) Bifurcation branches of peroneal artery—one of these branches supplied the medial plantar branch to the foot.
DIAGNOSTIC ANGIOGRAPHY
Digital subtraction angiography (DSA) is the gold standard for assessing vessel anatomy in patients with peripheral vascular disease (17,18). Studies have shown that unless the technique of DSA is done correctly, significant diagnostic errors can occur when imaging infrapopliteal vessels (17,18). Optimized DSA has an overall sensitivity and specificity of 96% and 92%, respectively, when utilized to image infrapopliteal vessels (19).
The infrapopliteal circulation is best viewed using injection of contrast from a selective catheter in the ipsilateral distal SFA or midpopliteal artery (3 to 4 cc/sec for a total of 9 to 12 cc). Injections of contrast agent from a catheter located in the ipsilateral distal external iliac artery or common femoral artery may not be sufficient to allow adequate definition of the infrapopliteal anatomy. The most common catheters used include 4- or 5-Fr. straight or angled angiographic catheter (e.g., glide catheter, Bernstein, straight flush, multipurpose). Vasodilators (e.g., nitroglycerin, verapamil, nitroprusside) that induce reactive hyperemia may be utilized to improve vessel opacification.
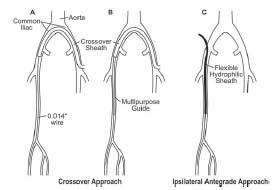
Figure 17.3 • A—C: Illustration of the access strategy techniques used for infrapopliteal endovascular procedures. See text for details.
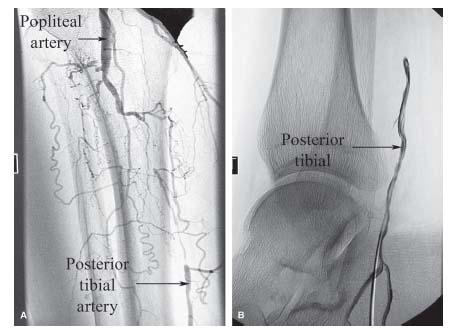
A straight anteroposterior (AP) view will demonstrate the infrapopliteal vasculature in the majority of patients. If the origin of the anterior tibial artery is not well seen, or the cortex of the fibula or tibia is obstructing visualization, then a 30°, ipsilateral oblique image will usually display the infrapopliteal bifurcation. Occasionally, a contralateral oblique view will be required to examine segments of the tibial vessels in the midleg, where there is often overlap particularly between the peroneal and anterior tibial arteries. A true lateral view will also help visualize the very distal aspect of the popliteal artery, and is often necessary in patients with a knee prosthesis. One of the important elements of tibial angiography, particularly in patients with CLI, is a careful angiographic examination of the arterial anatomy of the foot to help determine the most appropriate tibial target for revascularization. A steep contralateral oblique view is routinely performed in most laboratories. However, an AP cranial view is also very useful in delineating the lateral and medical plantar branches that are typically overlapped in the oblique contralateral view, and in differentiating the dorsalis pedis branch from collateral branches on the dorsum of the foot (Fig. 17.4).
Ideally, a low-osmolar, nonionic contrast solution is used to maximize patient comfort during peripheral angiography. Alternatively, gadolinium is a contrast agent commonly used during magnetic resonance imaging (MRI) that also may be used for infrapopliteal angiography. When selectively injected from the midpopliteal artery, gadolinium provides an adequate image of the infrapopliteal circulation.
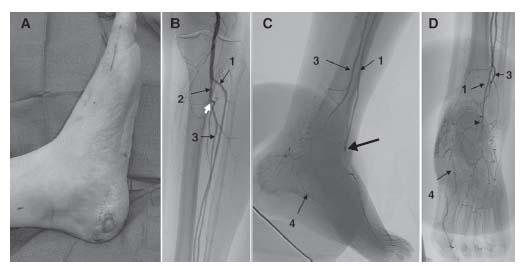
Figure 17.4 • Angiography of the tibial and pedal vessels in a patient with wound on medial aspect of left heel. A: Appearance of wound on left heel. B: Tibial angiography demonstrating occlusion of the posterior tibial artery (white arrow). C: Lateral angiogram of the foot demonstrating occlusion of the dorsalis pedis branch (arrow) and collateral filling of a plantar branch. D: Antero-posterior cranial view of the foot confirming that the plantar branch that fills via collaterals is the medial plantar branch and that the dorsalis pedis branch is occluded (arrowhead).
INTERVENTION
General Strategy
Infrapopliteal intervention is usually reserved for the patient with ischemic rest pain or tissue loss. There are rare patients who have true, lifestyle-limiting, intermittent claudication from isolated infrapopliteal disease. Obtaining a careful history is essential to determine the duration of symptoms, as thrombolytic therapy may be the initial intervention in the patient with an acute change in clinical status. A meticulous physical examination of the area of tissue loss is necessary to elicit any signs of infection or underlying osteomyelitis, either of which may adversely affect the success of any interventional therapy. Nuclear scanning or MRI may be important additional diagnostic modalities to characterize the presence of osteomyelitis.
The initial diagnostic angiogram will typically be obtained from the contralateral, common femoral artery, or bra-chial artery access, unless the patient has had prior CT or MR angiography. It is important to emphasize that routine invasive angiography remains critical to the accurate assessment of the infrapopliteal anatomy in patients with CLI due to the limitations of currently available noninvasive angiographic techniques. After demonstrating the infrapopliteal anatomy, the decision regarding approach and interventional modality may be made. For proximal, focal, stenotic disease, a contralateral common femoral artery access will usually suffice. For long occlusions and severely calcified or distal disease (i.e., below mid-calf), an antegrade approach is preferable.
In general, to resolve ischemic rest pain or heal an ischemic ulcer, it is necessary to achieve patency to one infrapopliteal vessel to the foot. Since rest pain typically involves the forefoot, the tibial target in this instance should ideally provide the main contribution to the metatarsal arch. In patients with tissue loss, the tibial target should provide flow to the affected area. For wounds that affect the digits (the most common scenario), the tibial target should again supply flow to the metatarsal arch. Less common wound locations such as the heel and malleoli require a careful examination of the arterial anatomy to determine the most appropriate tibial target. These considerations emphasize the need to identify the most appropriate tibial target for revascularization primarily based on the clinical indication, and not on the anticipated complexity of the procedure to open a given tibial vessels. Where two tibial vessels contribute equally to a given area of ischemia, the tibial vessel with the least complex disease can be approached. At times, two vessels may be recanalized without significant additional time, difficulty, or risk to the patient.
Anticoagulation/Antithrombotics
The pattern of infrapopliteal disease (i.e., focal stenotic or diffuse) will dictate the intensity of anticoagulation and antiplatelet therapy. In addition, the clinical presentation (i.e., acute or chronic presentation) will play a role in what pharmacologic adjuncts will be used.
In regard to antiplatelet therapy, the patient should be taking the combination of aspirin and an ADP-receptor inhibitor (e.g., ticlopidine or clopidogrel) prior to coming to the angiographic suite. For patients with diffuse infrapopliteal disease that may be scheduled to undergo rotational atherectomy or excimer laser therapy, intravenous glycoprotein (GP) IIb/IIIa inhibitor use may, theoretically, be useful in preventing platelet aggregation and development of the no-reflow phenomenon. In addition, in the limb salvage situation where there is tissue loss, those patients undergoing stand-alone angioplasty for long-segment disease may also be considered candidates for use of a GP IIb/IIIa inhibitor. However, further study and data are required before routine use can be recommended. As the patient with infrapopliteal disease likely has multivascular bed atherosclerosis, a consideration for chronic combination therapy with aspirin and ADP-receptor inhibitor administration, following infrapopliteal intervention, should be made.
Unfractionated heparin has been used most often as an anticoagulant agent during infrapopliteal intervention. Patients receive 50 to 70 U/kg, intravenously, as a bolus at the start of the procedure, with a goal activated clotting time (ACT) of 250 to 300 seconds. There is limited experience using low-molecular-weight heparin during infrapopliteal intervention, although a comfort level is certainly being established for its application during coronary intervention. The use of low-molecular-weight heparin during peripheral intervention is currently the subject of ongoing clinical trials. In regard to direct thrombin inhibitors for infrapopliteal intervention, the use of bivalirudin was studied as part of the Angiomax Peripheral Procedure Registry of Vascular Events (APPROVE) study (20). The APPROVE study group determined that bivalirudin provided consistent anticoagulation and similar outcomes in all vessel types treated, with low ischemic and bleeding events both in hospital and at 30 days (20).
Guide/Sheath
If intervention is being performed from the contralateral common femoral artery (i.e., crossing over the aortic bifurcation), the crossover sheath, itself, may be used as a guide, especially if treating proximal focal stenotic disease. Flexible 4- to 6-Fr. crossover sheaths (i.e., nonkinking) are now available from a number of vendors. The distal portion of the sheath should be advanced to the distal ipsilateral external iliac artery or mid-common femoral artery. For more complex disease being approached from the contralateral common femoral artery, a long, 4- to 6-Fr. sheath, or a 6-Fr. multipurpose coronary guide catheter telescoped through a standard crossover sheath, may be advanced to the level of the distal SFA or midpopliteal artery. If there is significant SFA disease precluding safe passage of the 6-Fr. multipurpose coronary guide, the SFA disease should be treated first.
If the infrapopliteal intervention is being performed from an antegrade approach, a flexible, hydrophilic, 4- to 6-Fr., 30- to 55-cm sheath, placed to the level of the distal SFA or midpopliteal artery will be sufficient. The antegrade approach is preferred when treating more complex disease such as total occlusions or long, segmental, diffuse disease.
Wires
The interventional treatment of infrapopliteal disease most commonly uses coronary modalities (e.g., balloons, rotational atherectomy, stents, laser) on a 0.014″ guidewire platform. The selection of which 0.014″ guidewire to use will be driven by the type of disease being treated (i.e., stenotic, occlusive, focal, diffuse). For focal stenotic disease, any commonly used, floppy, 0.014″ coronary guidewire may be used (e.g., Asahi Soft″Abbott Vascular, Santa Clara, CA). The guidewire is most easily manipulated if it is supported by an over-the-wire 0.014″ coronary balloon catheter (e.g., Maverick—Boston Scientific, Boston, MA), or a 0.014″/0.018″ low-profile catheter (e.g., Quickcross catheter—Spectranetics). For total occlusions, the group of 0.014″ coronary wires with stiffer tips specifically designed for crossing occlusions may be used (e.g., Miraclebro, Confi-anza—Abbott Vascular). Alternatively, a hydrophilic-coated, 0.018″ or 0.035″ guidewire may be used. The authors have had success using a 0.018″ angled hydrophilic wire that has a gold distal marker (manufactured by Terumo) inside of a 0.018″ Quickcross support catheter for crossing total occlusions. After successful crossing, the 0.018″ angled hydrophilic wire is then exchanged for a supportive, 0.014″ coronary-type guidewire (e.g., GrandSlam wire—Abbot Vascular) as a platform to perform the intervention.
When dealing with total occlusions that may not be crossed from the antegrade approach, Dorros and coworkers (21) have described their use of a surgical cut-down procedure on the tibial vessel, to achieve retrograde access in two cases. In similar cases, the authors have successfully entered the distal tibial vessel, using a micropuncture technique for advancement of a 0.018″, hydrophilic wire through the occlusion, in a retrograde fashion (22). The wire is then snared at the popliteal artery and externalized through an antegrade femoral sheath. Following removal of the tibial sheath, the endovascular procedure was then completed from the ante-grade access (Figs. 17.5 and 17.6).
Angioplasty
Standard 0.014″ low-profile balloon catheters, ranging from 1.5 to 4 mm in diameter, may be used in the majority of interventions for focal stenoses, when attempting stand-alone angioplasty for infrapopliteal disease. At experienced centers, the acute technical success of angioplasty in primarily focal in-frapopliteal stenoses is excellent, at approximately 98%. The success in treating total occlusions appears to be somewhat less. Clinical results are favorable. When defined by a pain-free extremity and limb salvage, success is reported in up to 84% at 2 to 5 years, in patients treated with angioplasty (23,24).
Traditionally, more diffuse, long-segment, diseased tibial vessels appear to have a lower clinical success rate when treated with stand-alone balloon angioplasty (i.e., 57% at 3 years) (25). Fortunately, there has been a major development and improvement in both angioplasty balloon catheters that are now manufactured for dedicated tibial artery use. The new relevant design characteristics include extremely low-profile tapered 0.014″ balloon catheter types, and longer balloon lengths including 120, 150, and 220 mm. While a monorail platform is most efficient, the best pushability and tracking characteristics have been obtained utilizing over-the-wire platforms. Other important technical characteristics applied to these new balloons include low compliance and the ability to sustain medium-high pressure inflations, improving the remodeling of the treated vessel, especially when employing prolonged inflation times.
Utilizing this new generation of long balloons, Graziani et al. (26) have published very impressive clinical outcomes in dialyzed patients with long-segment tibial disease with CLI. Immediate technical success was achieved in 97% of cases, with cumulative limb salvage rates (median follow-up, 22 months) at 12, 24, 36, and 48 months of 96%, 84%, 84%, and 62%, respectively. Limb salvage without any new intervention on the same leg was achieved in 70% of patients, and repeat interventions were performed on 23 (17%) legs.
The authors have experience using coronary cutting balloons for complex, infrapopliteal stenoses, such as lesions at vessel bifurcations, and heavily calcified lesions (Fig. 17.7). The cutting balloon (Boston Scientific, Boston, MA) utilizes atherotomes attached in a longitudinal fashion on the balloon, to score the stenotic lesion during inflation. This is thought to provide effective dilation and intimal disruption requiring less relative wall tension (27).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree