Interrupted and Hypoplastic Aortic Arch
Interrupted Aortic Arch
Interruption of the aortic arch is a rare condition that requires a patent ductus arteriosus for survival. A ventricular septal defect is often present and may be associated with left ventricular outflow obstruction due to malalignment of the conal septum. Other associated anomalies include a bicuspid aortic valve, truncus arteriosus, and aortopulmonary window. The aortic arch may be interrupted at one of three sites. The interruption may be just distal to the left subclavian artery (type A), between the left carotid and left subclavian arteries (type B), or between the innominate and left carotid artery (type C) (Fig. 29-1). Type B is the most common form of interrupted aortic arch, and type C is very rare.
Hypoplastic Aortic Arch
Hypoplasia of the aortic arch may occur with or without a discrete coarctation. Hypoplasia of the proximal arch between the innominate and left carotid arteries is defined as a diameter less than 60% of that of the ascending aorta. The distal arch between the left carotid and left subclavian arteries is considered hypoplastic if the diameter is less than 50% that of the ascending aorta. A hypoplastic aortic arch may be associated with a ventricular septal defect and other congenital heart lesions.
Patients with an interrupted or hypoplastic aortic arch usually present as neonates when the ductus arteriosus closes and flow to the descending aorta ceases or is severely restricted. Low cardiac output with metabolic acidosis is soon evident. Infusion of prostaglandin E1 is immediately started to reopen the ductus arteriosus to perfuse the distal aorta. When the patient’s general condition has improved and the low output state has been corrected, semiurgent surgical intervention is contemplated. One-stage complete repair of the aortic arch and associated cardiac defects is the preferred technique.
Incision
A median sternotomy is performed. Most of the thymus gland is removed to allow adequate mobilization of the branches of the aortic arch.
Cannulation
Traditionally, deep hypothermic arrest has been used for surgery involving the aortic arch. More recently, low-flow cerebral perfusion has been advocated during reconstruction of the arch to avoid or minimize circulatory arrest and cerebral ischemia.
A purse-string suture is placed on the right side of the distal ascending aorta near the origin of the innominate artery. In patients with an interrupted aortic arch, a second purse-string suture is placed on the proximal main pulmonary artery. The right and left pulmonary arteries are dissected and encircled with Silastic tourniquets. Dual arterial cannulation with flexible 8 to 10-F aortic cannulas is achieved using a Y-connector on the arterial line for interrupted aortic arch. Single aortic cannulation is used with a hypoplastic aortic arch. The right atrial cannula is then placed through a purse-string suture on the right atrial appendage. If intracardiac defects need to be addressed, bicaval cannulation is performed. A vent is placed through the right superior pulmonary vein (see Chapter 4). As cardiopulmonary bypass is initiated, the snares on the right and left pulmonary arteries are tightened to prevent flooding of the pulmonary bed.
Technique: General
While cooling is being carried out, the innominate artery, left common carotid artery, and left subclavian artery are mobilized, and snares are placed around them. The ductus arteriosus is also dissected, and the descending aorta is mobilized distally beyond the level of the left bronchus. Also during this period, the intracardiac lesions can be repaired after cross-clamping the aorta and administering cardiopegia into the aortic root. Following the intracardiac procedure, the aortic cannula is advanced into the innominate artery, and the snare around the innominate artery is tightened. The pump flow is reduced to 10 to 20 mL per kilogram per minute, and adjusted to maintain a right radial pressure of 30 to 40 mm Hg. The left carotid and left subclavian tourniquets are snugged down, and a curved vascular clamp is applied to the distal descending aorta.
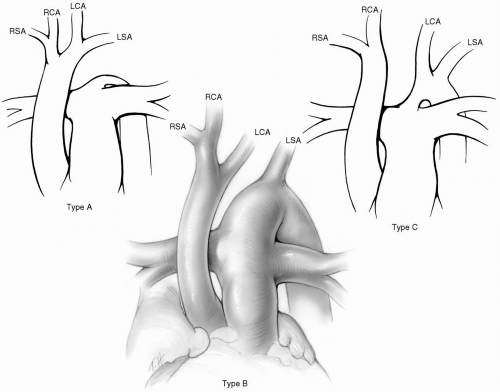 FIG 29-1. Interrupted arch, types A, B, and C. RSA, right subclavian artery; RCA, right carotid artery; LCA, left carotid artery; LSA, left subclavian artery. |
If an anomalous origin of the right subclavian artery from the descending aorta is present, the pressure in the right temporal artery should be monitored during low-flow cerebral perfusion.
Whether or not the cardiac lesion requires a systemic-pulmonary shunt, the surgeon may elect to sew a 3- or 3.5-mm GORE-TEX tube end-to-side to the innominate artery, and secure an olive-tipped or small arterial cannula inside the graft. Low-flow cerebral perfusion is then performed after clamping the takeoff of the innominate artery. Alternatively, a brief period of hypothermic arrest is used to open the arch. The arterial cannula is then placed into the innominate artery under direct vision. The tourniquet around the innominate artery is then snugged down, and low-flow cerebral perfusion is begun. The arch repair can now proceed.
Technique: Interrupted Aortic Arch
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



