CHAPTER 75 Injury to the Heart and Great Vessels
BLUNT CARDIAC INJURY
Historical Perspective
Cardiac chamber rupture and myocardial contusion were first reported after autopsy findings as early as 1679 by Borch1 and in 1764 by Akenside.2 In 1868, 76 cases reported by Fischer3 described 7 myocardial contusions and 69 traumatic ruptures. Experimental animal work and clinical autopsies by Beck and Bright4 demonstrated that severe forces are responsible for an entire range of cardiac trauma, whereas enormous force is required to rupture the heart. Recovery is the general rule, and rupture is the exception. In 1958, Parmley5 performed a hallmark study reviewing a large series of autopsy cases at the Armed Forces Institute of Pathology and demonstrated that blunt traumatic heart injury had a 0.1% incidence, with the majority being isolated chamber ruptures (right then left ventricle, followed by right and left atria in decreasing order of occurrence) and some associated with combined aortic ruptures. Blunt cardiac injury is the most commonly seen form of cardiac trauma and rarely results in death. Cardiac chamber or aortic rupture is usually fatal.
Mechanism, Pathophysiology, and Incidence
These forces result in a continuous spectrum of cardiac injury ranging from simple contusion to fatal cardiac chamber rupture, including commotio cordis, described as sudden cardiac arrest from a sternal blow.6 Myocardial contusion, characterized by patchy areas of muscle necrosis and hemorrhagic infiltrate, may also impair ventricular contraction and lead to arrhythmia.
Clinical Presentation and Diagnosis
The rupture of a cardiac chamber or blunt injury to a coronary artery, a major intrapericardial vein, or the ascending aorta is usually fatal because of acute pericardial tamponade. The few patients who survive do so only because of tears in a cavity under low pressure.7–9 Blunt cardiac injury (myocardial contusion) induces cardiac failure and arrhythmia that improves with time.10,11 Injury to a coronary artery can lead to immediate or delayed myocardial infarction with spasm or dissection of the arterial wall.12 Valvular tears resulting in aortic or mitral insufficiency can develop into cardiac failure, ranging from a few hours to a few weeks, whereas tricuspid insufficiency may appear only after several years.13–15
Paramount to an accurate diagnosis is information derived from the history and physical findings. A history or findings of pain and tenderness over the anterior chest wall (which may be indistinguishable from a classic myocardial infarction), evidence of chest wall contusion, ecchymosis, anterior rib fractures, and flail chest are all associated with cardiac injury.16 Many patients, however, do not present with characteristic history, signs, or symptoms.11,17,18 Complex arrhythmias, subtle findings of a precordial thrill, or a murmur may also be noted on physical examination. Cardiac injury can also be manifested by hemodynamic instability marked by refractory hypotension and elevated venous and cardiogenic shock. External jugular vein distention may be absent in cases of blood loss.
Electrocardiography
Serial 12-lead electrocardiography has traditionally been used to screen patients for conduction disturbances; however, no pathognomonic finding exists that specifically establishes the diagnosis of blunt cardiac injury.16 Electrocardiographic abnormalities that have been reported in blunt cardiac injury range from sinus tachycardia, the most common, to supraventricular arrhythmias such as atrial flutter and atrial fibrillation, ventricular tachycardia, premature ventricular contractions, ventricular fibrillation, right bundle branch block with first-degree heart block or hemiblock, third-degree heart block, and T-wave or ST-segment abnormalities.16,17 Normal electrocardiography in a patient who is hemodynamically stable warrants no further investigation.
Cardiac Enzymes and Troponins
Measurement of the creatine kinase–myocardial band isoenzyme (CK-MB) has been shown to be unreliable,11,18–24 except when it is combined with the more specific muscle proteins, including troponin (cardiac troponins T and I).25–28 Combined abnormalities in electrocardiography and serial cardiac troponin I (cTnI) levels have been promising in showing increased sensitivity (62% if both are positive) and specificity (100% if both are negative)29,30 versus cTnI alone, which demonstrated low sensitivity (23%) but high specificity (97%).31
Two-Dimensional Transthoracic or Transesophageal Echocardiography
Bedside echocardiography has become an important diagnostic tool in trauma patients, detecting abnormalities in the heart (ventricular dyskinesia and valvular dysfunction) and thoracic aorta as well as the presence of pericardial fluid.16,32–35
There are limitations. Transthoracic echocardiography cannot be performed in 25% to 30% of patients because of chest wall edema, fractured ribs, and flail chest. Transesophageal echocardiography, a more useful adjunct in elucidating periaortic hematoma and other cardiac injuries, is limited by expertise. Transesophageal echocardiography frequently requires intubation and cannot be performed in patients with facial or cervical trauma.32,33
Radionuclide Scans
Technetium Tc 99m pyrophosphate, thallium Tl 201, single-photon emission computed tomography, and multiple gated acquisition scans use the concept of radioactive substances binding to myocardial injuries or infarcts. However, all have been abandoned secondary to low sensitivity and specificity in the detection of blunt cardiac injury.16
Spectrum of Blunt Cardiac Injury: Assessment and Management
Pericardial Injury
Blunt rupture of the pericardium can occur from direct forceful impact to transmitted force from sudden increased intra-abdominal pressure. Left pericardial tears parallel to the phrenic nerve are most common, followed by diaphragmatic and right mediastinal tears.7 The heart might eviscerate into the abdominal cavity or herniate through the pericardial sac with torsion of the great vessels. Stable patients are assessed and injuries are diagnosed with chest radiography, sonography, or computed tomography. Hemodynamically compromised patients are treated with immediate surgical intervention (emergency department thoracotomy), with diagnosis made at thoracotomy. The heart is reduced into the pericardial sac. The pericardium may be closed with or without a Gore-Tex patch to achieve a tension-free repair and help prevent recurrent cardiac herniation.
Valvular, Papillary Muscle–Chordae Tendineae, and Septal Injury
Valvular injuries rarely occur, but when they do, the aortic valve is the one most commonly affected, followed by the mitral valve. Rapid displacement of blood secondary to crushing or compressive forces applied to the thoracic cage during ventricular diastole may lacerate cardiac valve leaflets (most common in the left coronary cusp followed by the noncoronary cusp), papillary muscles, or chordae tendineae, leading to valvular insufficiency.5 The classic signs of valvular insufficiency (new murmur, thrill, or left ventricular dysfunction with cardiogenic shock and associated pulmonary edema) may not be immediately recognized secondary to other concomitant life-threatening injuries. In stable patients, such findings should prompt further diagnostic studies, depending on clinical status of the patient, and prompt repair or replacement as necessary. Septal rupture is also uncommon, and prompt repair is necessary if the patient is symptomatic from significant left-to-right shunting.36
Blunt Coronary Artery Injury
Injuries of the coronary arteries are extremely rare. The proximal right coronary and, more commonly, the left anterior descending artery (due to the location relative to the sternum) become injured with direct compression of sternum to coronary vessel or stretching of the vessel secondary to cardiac torsion, leading to thrombosis or intimal disruption. The result is no different from an acute myocardial infarction. Long-term sequelae of these injuries can also lead to ventricular aneurysm and eventual rupture, ventricular failure, production of emboli, or malignant arrhythmia.5
Cardiac Chamber Rupture
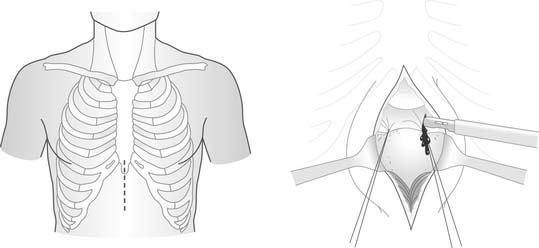
Cardiac chamber rupture is relatively uncommon7,37–39; only a small percentage of patients survive to reach the hospital. Several mechanisms for blunt cardiac rupture have been postulated7: direct precordial impacts; compression of the heart between the sternum and vertebral body; transmission of pressure through the abdomen into the venous return, rupturing particularly the atria; acceleration-deceleration injuries, leading to tears of the heart at the attachment sites to the great vessels; blast effects; and concussive blows thought to be fatal secondary to the production of malignant arrhythmias. Patients usually present with persistent hypotension with evidence of pericardial tamponade. Diagnosis of widened mediastinum on chest radiography or evidence of pericardial fluid on sonographic examination requires prompt intervention. Once popular as an initial diagnostic modality, subxiphoid window (Fig. 75-1) should be avoided, as it consumes valuable time, results in a secondary thoracic incision, and exposes a ruptured heart from a tiny abdominal incision. For patients who present with cardiopulmonary arrest, an emergency department thoracotomy may be their only chance, although survival statistics are dismal.
PENETRATING CARDIAC INJURY
Historical Perspective
Historically, an injury to the heart has been considered a death sentence. As early as the Iliad,42 Sarpedon died of an impalement to the heart by a lance. Hippocrates,43 Aristotle,44 Galen,45 Fabricius,46 and Boerhaave47 described such wounds to the heart as futile. Morgagni,48 in 1761, described the compressive effects of blood on the heart with hemopericardium. Larrey49 was credited for pioneering the technique of pericardial window to release pericardial tamponade. Ludwig Rehn50 performed the first successful repair of a cardiac injury in 1896 in Frankfurt.
Duval51 first described the median sternotomy incision; Spangaro,52 in 1906, first described the left anterolateral thoracotomy incision. Beck, in 1926, described the triad physiology of cardiac tamponade and later described the repair technique of placing mattress sutures under the coronary vessels to spare ligation.53,54
Harken,55 in 1946, described the removal of foreign bodies adjacent to the heart and great vessels. Beall56–59 first described emergency department thoracotomy and along with Cooley58 reported the potential benefits of cardiopulmonary bypass in the management of selected intracardiac injuries. Mattox60–62 further refined emergency department thoracotomy and cardiorrhaphy including emergency cardiopulmonary bypass.
Mechanism, Pathophysiology, and Incidence
In the military arena, most soldiers do not survive the high-velocity automatic rifle injuries seen in battle. The majority of these patients have sustained injuries from fragments of grenades or shrapnel. Rich63 described 96 patients with penetrating injuries arriving at treatment facilities based on data from the Vietnam conflict.
Penetrating cardiac injuries are uncommon and are most often described in busy urban trauma centers. However, even iatrogenic penetrating cardiac injury can be seen in any clinic or hospital, especially after pericardiocentesis. The true incidence is difficult to ascertain because the numbers fluctuate in conjunction with the incidence of violent crimes involving firearms or penetrating objects. Feliciano64 described a 1-year experience of 48 cardiac injuries at Ben Taub Hospital in Houston. Mattox,65 in 1989, described a 30-year experience from the same institution, reporting 539 cardiac injuries. Asensio66,67 reported a total of 165 cardiac injuries within a 3-year period at Los Angeles County–University of Southern California Medical Center. In 2000, Tyburski68 reported an 18-year experience of 302 patients with penetrating heart injuries undergoing emergency thoracotomy.
Clinical Presentation and Diagnosis
Most cardiac injuries caused by stab wounds are logically based on the trajectory of the insult. This is not so with gunshot wounds, which can injure the heart from precordial and extra-precordial entrance sites.69 Mattox70 described 26% associated cardiac injuries in 82 patients presenting with combined thoracoabdominal injuries; Asensio71 reported 44% incidence of associated penetrating cardiac injuries in his series of 73 patients who sustained thoracoabdominal injuries.
Frank penetrating injuries to the cardiac chambers may lead to acute cardiac tamponade and death; similarly, hemorrhage through the lacerated pericardium into the hemithorax can lead to death as well. Patients surviving such injuries have intact pericardium that prevents fatal exsanguinating hemorrhage and allows them to reach the trauma center alive but with varying degrees of hemodynamic instability63,66 secondary to pericardial tamponade. Interestingly, Beck’s triad (muffled heart sounds, jugular venous distention, and hypotension) and Kussmaul’s sign (jugular venous distention with inspiration) are present in only 10% of patients69 with pericardial tamponade.
Moreno,72 in a retrospective study looking at 100 patients with penetrating cardiac injuries, reported higher survival (77% versus 11%) in patients who present with pericardial tamponade, and right-sided chamber injuries confer a higher survival (79%) versus left-sided chamber injuries (28% survival).
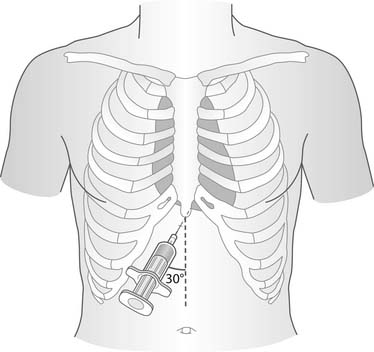
Subxiphoid Pericardial Window
The reliability of this technique (see Fig. 75-1) versus pericardiocentesis (Fig. 75-2) has been controversial in the evaluation and treatment of penetrating cardiac injury.73–78 These techniques might demonstrate hemopericardium when two-dimensional echocardiography (applied in focused abdominal sonography for trauma) is not available; however, such techniques are time-consuming, result in exposure of a cardiac injury through a very small incision, and lead to a secondary thoracic operation. A transdiaphragmatic pericardial exploration at the time of laparotomy79 has been reported to be effective in patients who sustained combined thoracoabdominal injuries.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree