Chapter 28 Infrainguinal Endovascular Reconstruction
Technique and Results
Patient Selection and Preoperative Imaging
Infrainguinal occlusive disease can be classified by its morphology, which assists in determining which patients are best managed with endovascular intervention and which ones require surgery. The TransAtlantic Inter-Society Consensus (TASC) classification (Box 28-1) and others have defined disease morphology in an effort to clarify the issue of lesion severity.1 The general concept is that endovascular techniques are preferred in patients with less severe forms of disease and among those with shorter life expectancies or greater periprocedural risk factors. Conversely, open surgical approaches have a better risk-benefit profile in patients with fewer medical comorbidities or more severe forms of disease, such as long-segment occlusions, in which endovascular procedures are less durable. The recommendation from the TASC group is that type A lesions be treated with endovascular intervention, type D lesions be treated with surgery, and types B and C lesions be treated with either, depending on the patient’s comorbidities, general medical condition, expected longevity, and availability of conduit for bypass.
Box 28-1
TransAtlantic Inter-Society Consensus Classification of Femoropopliteal Lesions
From Schneider PA, Nelken N, Caps MT: Angioplasty and stenting for infrainguinal lesions. In Yao JST, Pearse WH, Matsumura JS, editors: Trends in vascular surgery, Chicago, 2003, Parmentier Publishing, p 292.
Approaches
Percutaneous intervention for infrainguinal occlusive disease is usually performed through the contralateral femoral artery using an up-and-over approach or through the ipsilateral femoral artery using an antegrade approach (Table 28-1). Infrainguinal interventions can also be performed through the brachial artery, but this approach is rarely required and may be more challenging because of the longer distances involved and the higher likelihood of access-related complications. The primary advantages of the up-and-over approach, which is most commonly used, are the following: an aortogram with runoff can be easily converted to endovascular therapy; it permits evaluation of the inflow aortoiliac arteries before treatment of infrainguinal lesions; only a simple retrograde femoral puncture is required; and it facilitates selective catheterization of the superficial femoral artery (SFA) orifice and treatment of proximal SFA lesions, which can be difficult via the ipsilateral antegrade approach. Furthermore, puncture site management is contralateral to the intervention site rather than proximal to it. The antegrade approach may be used for better guidewire and catheter control in infrapopliteal intervention and also in patients who have contraindications to the up-and-over approach. The likely approach is determined before the procedure in order to facilitate room setup and the availability of supplies, but both groins are always prepared in case an alternative approach is required during the procedure.
TABLE 28-1 Comparison of Approaches to Infrainguinal Interventions: Up-and-Over versus Antegrade
| Up-and-Over Approach | Antegrade Approach | |
|---|---|---|
| Puncture | Simple retrograde femoral | More challenging, less working room |
| Catheterization | Challenging with tortuous arteries, narrow or diseased aortic bifurcation; easier to catheterize SFA when going up and over femoral | Entering SFA from antegrade approach requires proximal puncture and selective catheter |
| Guidewire and catheter control | Fair | Excellent |
| Catheter inventory | More supplies needed | Minimal, shorter catheters |
| Specialty items | Up-and-over sheath, long balloon catheters | None |
| Indications | Proximal SFA disease, CFA disease ipsilateral to infrainguinal lesion, obesity | Infrapopliteal disease, patients with contraindication to up-and-over approach |
CFA, Common femoral artery; SFA, superior femoral artery.
From Schneider PA: The infrainguinal arteries—advice about balloon angioplasty and stent placement. In Endovascular skills, ed 2, New York, 2003, Marcel Dekker, p 316.
Technique
Up-and-Over Approach
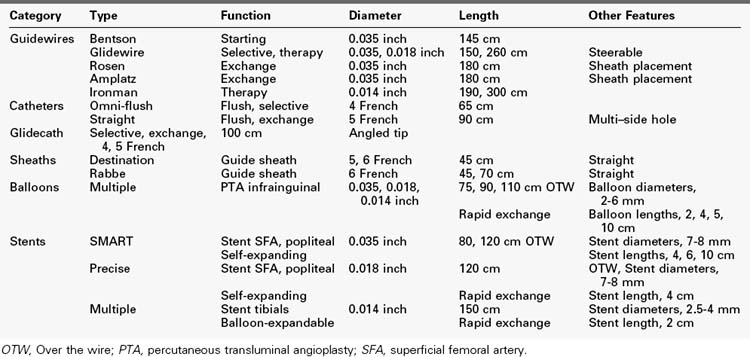
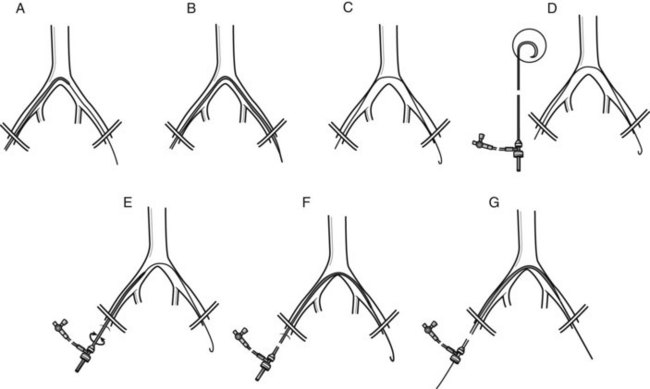
Supplies required for an up-and-over approach are listed in Table 28-2. This approach requires longer guidewires, catheters, and sheaths than the antegrade approach. A standard retrograde common femoral artery puncture is performed contralateral to the symptomatic side. A floppy-tipped guidewire is passed into the aorta. A hook-shaped, multi–side-hole flush catheter, such as a 65-cm Omni-flush (AngioDynamics), is passed into the aorta, and an aortoiliac arteriogram is obtained. If bilateral runoff is required, it can be performed at that time with the catheter head placed in the infrarenal aorta. When only unilateral runoff on the symptomatic side is indicated, the catheter is passed over the aortic bifurcation, and lower extremity arteriography is performed. After evaluating the infrainguinal lesions, determining that the aortic bifurcation can accommodate an access sheath, and deciding that the up-and-over approach is best, an up-and-over sheath is placed (Figure 28-1).
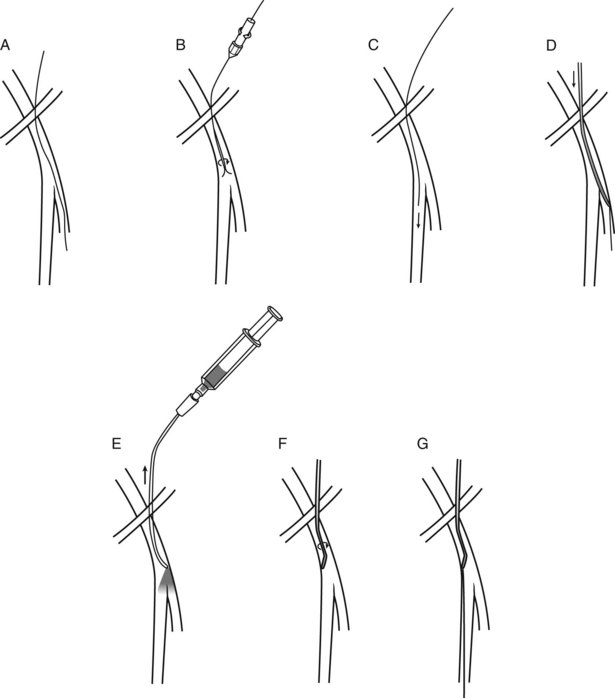
Figure 28-2 demonstrates the steps required for infrainguinal intervention using an up-and-over approach. The exchange guidewire is replaced with a steerable 260-cm Glidewire (Terumo Medical). The diseased infrainguinal segment is road-mapped through the side arm of the sheath, and the Glidewire is used to cross the lesion to be treated. Lesion crossing is facilitated by supporting the Glidewire with a hydrophilic catheter, such as a 5-French Angled Glidecath (Cook Medical) or Quick Cross catheter (AngioDynamics). If treatment of tibial lesions is planned, a 5-French, 100-cm-long catheter is advanced into the distal popliteal artery, and road mapping is performed through this catheter. A low-profile guidewire, usually an 0.014-inch hydrophilic wire such as an Asahi Grandslam (Abbott Vascular) is used to cross the tibial lesions, and the 5-French diagnostic catheter is exchanged for a 135-cm–long, 0.014-inch Quick Cross catheter (AngioDynamics) to support the wire. Interval arteriography may be performed through the side arm of the sheath or through the selective catheter using a Tuohy-Borst adapter during attempts at lesion crossing. Once the lesion has been crossed, the supporting catheter is advanced down to the level of the reconstituted artery, the wire is removed to assess for blood return from the catheter lumen, and confirmatory angiography is performed to demonstrate the intraluminal position of the catheter.
Antegrade Approach
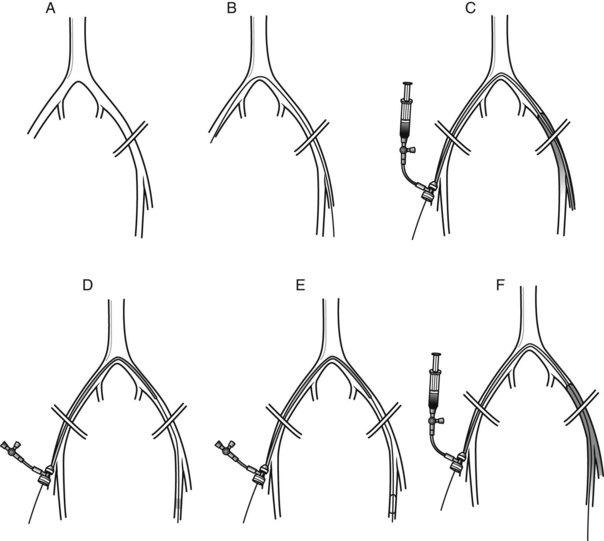
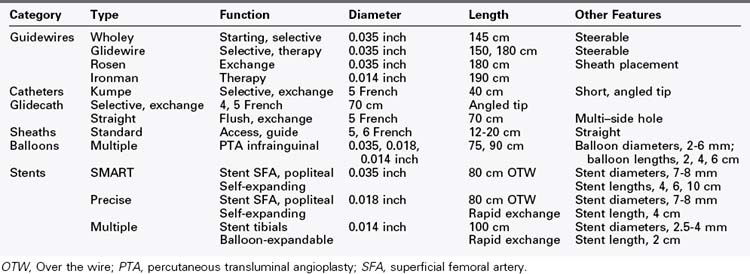
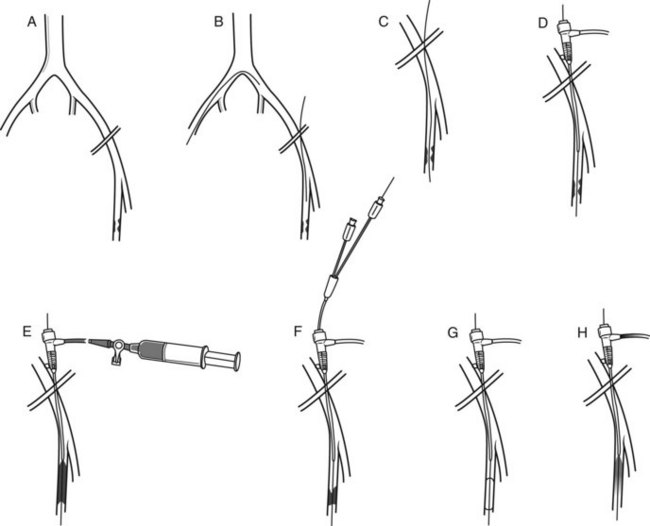
Supplies required for an antegrade approach are listed in Table 28-3. An antegrade common femoral artery puncture is performed ipsilateral to the symptomatic side. This approach is well suited to patients who have normal aortoiliac inflow, especially if tibial angioplasty is required or if there is a need to limit the use of contrast material. The puncture should be performed as proximally as possible along the common femoral artery to leave some working room between the puncture and the origin of the SFA. A steerable guidewire, such as the Wholey guidewire (Mallinckrodt, Hazelwood, Md.), is used; the shaft of this guidewire is more supportive for catheter and sheath passage than a Glidewire. The Wholey guidewire can often be steered anteromedially into the SFA. If not, the guidewire is advanced into the deep femoral artery, and an angled-tip catheter is placed over it (Figure 28-3). The image intensifier is placed in the ipsilateral anterior oblique position to open the femoral bifurcation, and the catheter is withdrawn enough to perform road mapping by refluxing contrast material into the SFA. The catheter is used to steer the guidewire into the SFA.
If the lesion is in the proximal to mid SFA, the artery is road mapped using the catheter, and the guidewire is advanced across the lesion (Figure 28-4). The same guidewire can be used for sheath placement. If the lesion is more distal in the artery, the guidewire is advanced without crossing the lesion, and the sheath is placed. The sheath size required may be 4, 5, or 6 French, depending on the platform used and treatment modality desired. An appropriately sized dilator is used to enlarge the arteriotomy before sheath placement.
Treatment Modalities
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree