The accuracy of the admission electrocardiogram (ECG) in predicting the site of acute coronary artery occlusion in patients with ST-segment elevation myocardial infarction (STEMI) and multivessel disease is not well known. This study aimed to assess whether the presence of multivessel coronary artery disease (CAD) modifies the artery-related ST-segment changes in patients with acute coronary artery occlusion. We reviewed the admission ECG, clinical records, and coronary angiography of 289 patients with STEMI caused by acute occlusion of left anterior descending (LAD; n = 140), right (n = 118), or left circumflex (LCx; n = 31) coronary arteries. All patients underwent primary percutaneous coronary reperfusion during the first 12 hours. The magnitude and distribution of artery-related ST-segment patterns were comparable in patients with single (n = 149) and multivessel (n = 140) CAD. Occlusion of proximal (n = 55) or mid-distal (n = 85) LAD artery induced ST-segment elevation in leads V 1 to V 5 , but only the proximal occlusion induced reciprocal ST-segment depression in leads II, III, and aVF (p <0.001). Proximal and mid-distal occlusion of right (n = 45 and 73, respectively) or LCx (n = 15 and 16) coronary artery always induced ST-segment elevation in leads II, III, and aVF and reciprocal ST-segment depression in leads V 2 and V 3 . ST-segment elevation in lead V 6 >0.1 mV predicted LCx artery occlusion. In conclusion, patients with STEMI with single or multivessel CAD have concordant artery-related ST-segment patterns on the admission ECG; in both groups, reciprocal ST-segment depression in LAD artery occlusion predicts a large infarct. Subendocardial ischemia at a distance is not a requisite for the genesis of reciprocal ST-segment changes.
The patterns of ST-segment shift are currently used to identify the infarct-related coronary artery and the level of the occlusion in patients with ST-segment elevation myocardial infarction (STEMI). In patients with multivessel coronary artery disease (CAD), the acute occlusion of a coronary artery may be associated with ischemia at a distance and this may modify the pattern of the ST-segment changes. However, the ability of the admission electrocardiogram (ECG) to predict the site of coronary occlusion in patients with STEMI with multiple CAD has not been systematically analyzed. The purpose of this study was to compare the accuracy of the admission ECG in predicting the site of coronary occlusion in patients with STEMI with single and multivessel CAD.
Methods
We reviewed the clinical records of 373 consecutive patients with STEMI submitted to primary percutaneous coronary reperfusion in our institution from October 2009 to December 2010. The diagnosis of STEMI was based on typical chest pain lasting >30 minutes associated with ST-segment elevation of >0.1 mV in at least 2 consecutive electrocardiographic leads (0.2 mV for leads V 2 and V 3 ). Patients with ST-segment changes secondary to left bundle branch block (n = 19) or artificial ventricular paced rhythm (n = 5) were excluded.
Demographic, clinical, and echocardiographic data were extracted from the clinical records. The admission 12-lead ECG was recorded within the first 12 hours of the STEMI. Two independent investigators unaware of the clinical and angiographic data reviewed the electrocardiographic parameters. Positive and negative displacements of the ST segment were measured at the J-point level. Reciprocal ST-segment changes were defined as ST-segment depression of >0.1 mV in any electrocardiographic lead other than aVR (0.05 mV for V 2 and V 3 ).
Primary coronary angioplasty was performed in all patients within the first 4.3 ± 3.2 hours from the onset of symptoms. Angiographic findings were evaluated by 2 independent experienced observers blinded to the clinical and electrocardiographic data. The infarct-related artery was identified by total coronary artery occlusion or angiographic evidence of an intraluminal thrombus. Flow through the culprit lesion was graded using the Thrombolysis in Myocardial Infarction trial criteria. Any additional coronary stenosis of >70% was considered significant. We also assessed the presence of chronic total coronary artery occlusions, the distribution of collateral vessels, and the pattern of coronary dominance. Patients were divided into 3 groups according to the infarct-related artery: left anterior descending (LAD), right, and left circumflex (LCx). In each vessel we differentiated between the proximal and mid-distal location of the occlusion taking as a reference the first diagonal branch in the LAD group, the 1/2 distance to the acute margin of the heart in cases of the right coronary artery, and the first marginal branch in the LCx group.
Informed consent was obtained from each patient. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the ethics committee of our institution.
Continuous variables are presented as the mean value ± SD and discrete variables as absolute value and percentage. Comparisons between continuous variables were assessed by the Student t test. Discrete variables were compared by the chi-square test. A p value <0.05 was considered statistically significant. Statistical analysis was performed using the software PASW statistics 19.0 (SPSS Inc, Chicago, Illinois).
Results
Among the 349 initially screened patients, we further excluded 19 with normal coronary angiography, 16 with unidentifiable infarct-related artery, and 25 in whom the infarct-related artery was a secondary vessel (the diagonal branch of the LAD artery in 8 cases, the intermediate branch in 3, the posterior descending or posterolateral branches of the right coronary artery in 6, and the marginal branches of the LCx artery in 8). Thus, 289 patients were entered in the final analysis.
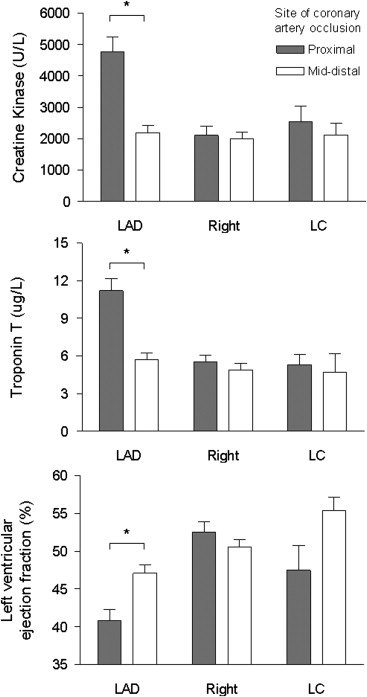
The demographic and clinical characteristics of patients with acute occlusion of the LAD, right, or LCx arteries were comparable ( Table 1 ). However, patients with proximal LAD artery occlusion showed the highest peak values of cardiac biomarkers and the lowest left ventricular ejection fraction ( Figure 1 ). Fourteen patients (4.8%) died during the hospital stay (cardiogenic shock in 13 patients and lethal arrhythmia in 1) and 11 of them presented with Killip class IV on admission. The in-hospital mortality distributed comparability among the 3 study groups with no further differences between patients with single or multivessel CAD.
| Variable | Coronary Artery Occluded | |||||
|---|---|---|---|---|---|---|
| LAD (n = 140) | Right (n = 118) | LCx (n = 31) | ||||
| Proximal (n = 55) | Mid-Distal (n = 85) | Proximal (n = 45) | Mid-Distal (n = 73) | Proximal (n = 15) | Mid-Distal (n = 16) | |
| Age (yrs) | 62.9 ± 16.3 | 61.9 ± 13.4 | 63.6 ± 11.9 | 61.5 ± 13.1 | 61.6 ± 15.1 | 57.3 ± 11.7 |
| Men | 44 (80) | 65 (77) | 37 (82) | 60 (82) | 12 (80) | 13 (81) |
| Body mass index (kg/m 2 ) | 27.7 ± 4.6 | 27.1 ± 3.5 | 26.8 ± 3.8 | 27.1 ± 4.0 | 28.5 ± 4.7 | 27.6 ± 5.5 |
| Hypertension | 30 (55) | 50 (59) | 23 (51) | 37 (51) | 9 (60) | 8 (50) |
| Dyslipidemia | 28 (51) | 42 (49) | 21 (47) | 34 (47) | 7 (47) | 10 (63) |
| Diabetes mellitus | 14 (26) | 24 (28) | 14 (31) | 15 (21) | 4 (27) | 3 (19) |
| Current smoker | 26 (47) | 41 (48) | 26 (58) | 43 (59) | 6 (40) | 9 (56) |
| Previous STEMI | 3 (6) | 3 (4) | 1 (2) | 7 (10) | 3 (20) | 0 |
| Previous non-STEMI | 0 | 3 (4) | 1 (2) | 3 (4) | 0 | 0 |
| Killip class | ||||||
| I | 34 (62) | 63 (74) | 37 (82) | 62 (85) | 10 (67) | 15 (94) |
| II | 13 (24) | 13 (15) | 4 (9) | 3 (4) | 2 (13) | 1 (6) |
| III | 2 (4) | 5 (6) | 0 | 1 (1) | 1 (7) | 0 |
| IV | 6 (11) | 4 (5) | 4 (9) | 7 (10) | 2 (13) | 0 |
| Hemoglobin (g/dl) | 14.0 ± 1.6 | 13.5 ± 1.8 | 13.3 ± 2.1 | 13.5 ± 1.7 | 12.8 ± 2.7 | 14.1 ± 2.2 |
| Creatinine (mg/dl) | 1.1 ± 0.5 | 1.0 ± 0.3 | 1.1 ± 0.6 | 1.0 ± 0.3 | 1.0 ± 0.4 | 1.1 ± 0.3 |
Coronary angiography evidenced single-vessel disease in 149 patients (51%) and multiple-vessel disease in the remaining 140 patients (48%; 2-vessel in 98 patients [34%] and 3-vessel in 42 patients [14%]). The percentage of patients with multivessel CAD, chronic coronary occlusion, or coronary collaterals was homogeneously distributed among the 3 study groups ( Table 2 ). A pattern of right coronary dominance was observed in most of the cases.
| Variable | Coronary Artery Occluded | |||||
|---|---|---|---|---|---|---|
| LAD (n = 140) | Right (n = 118) | LCx (n = 31) | ||||
| Proximal (n = 55) | Mid-Distal (n = 85) | Proximal (n = 45) | Mid-Distal (n = 73) | Proximal (n = 15) | Mid-Distal (n = 16) | |
| Number of coronary arteries narrowed | ||||||
| 1 | 26 (47)* | 49 (58)* | 22 (49) | 38 (52) | 6 (40) | 8 (50) |
| >1 | 29 (53)* | 36 (42)* | 23 (51) | 35 (48) | 9 (60) | 8 (50) |
| Collateral circulation | 18 (33) | 21 (25) | 25 (56) | 33 (45) | 4 (27) | 6 (38) |
| Chronic total occlusion | 6 (11) | 11 (13) | 4 (9) | 6 (8) | 2 (13) | 2 (13) |
| Right coronary dominance | 48 (87) | 73 (86) | 43 (96) | 73 (100) | 9 (60) | 12 (75) |
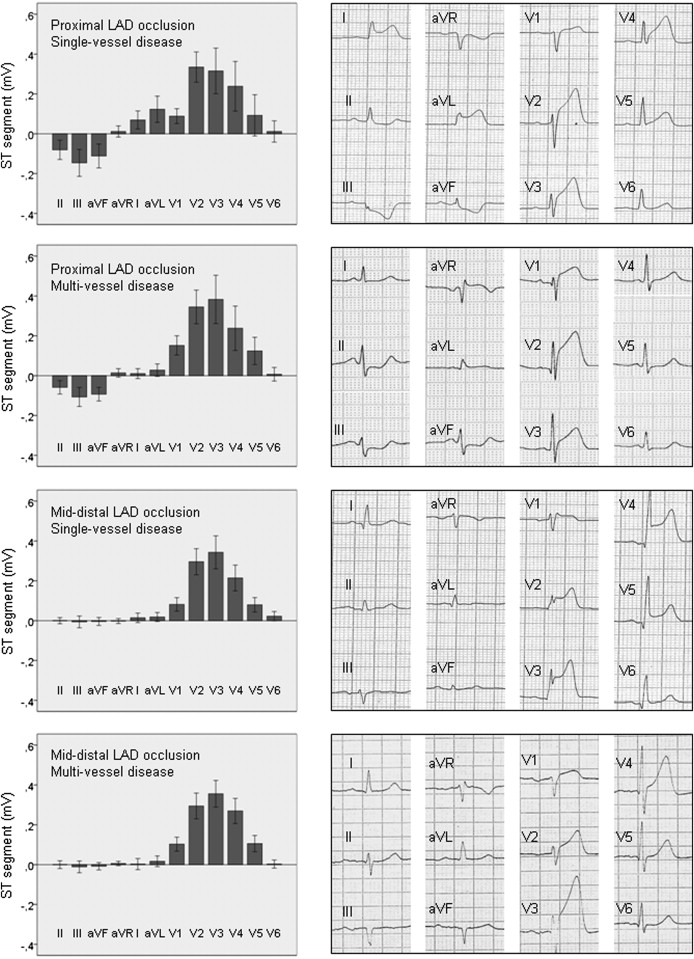
The first ECG was recorded within 183 ± 188 minutes from the onset of symptoms. The overall pattern and distribution of the ST-segment changes induced by acute proximal or mid-distal LAD artery occlusion was comparable in patients with single or multivessel CAD ( Figure 2 ). However, the multivessel group presented subtle differences: lower ST-segment elevation in leads I (0.01 ± 0.07 vs 0.07 ± 0.12 mV, p = 0.03) and aVL (0.03 ± 0.08 vs 0.12 ± 0.17 mV, p = 0.01) and greater ST-segment elevation in lead V 1 (0.15 ± 0.13 vs 0.09 ± 0.10 mV, p = 0.05). The first septal branch was involved in 36 of the 55 patients of the proximal LAD group. These patients showed greater ST-segment depression in leads III (−0.17 ± 0.16 vs −0.06 ± 0.10 mV, p = 0.02) and aVF (−0.13 ± 0.13 vs −0.06 ± 0.09 mV, p = 0.04).
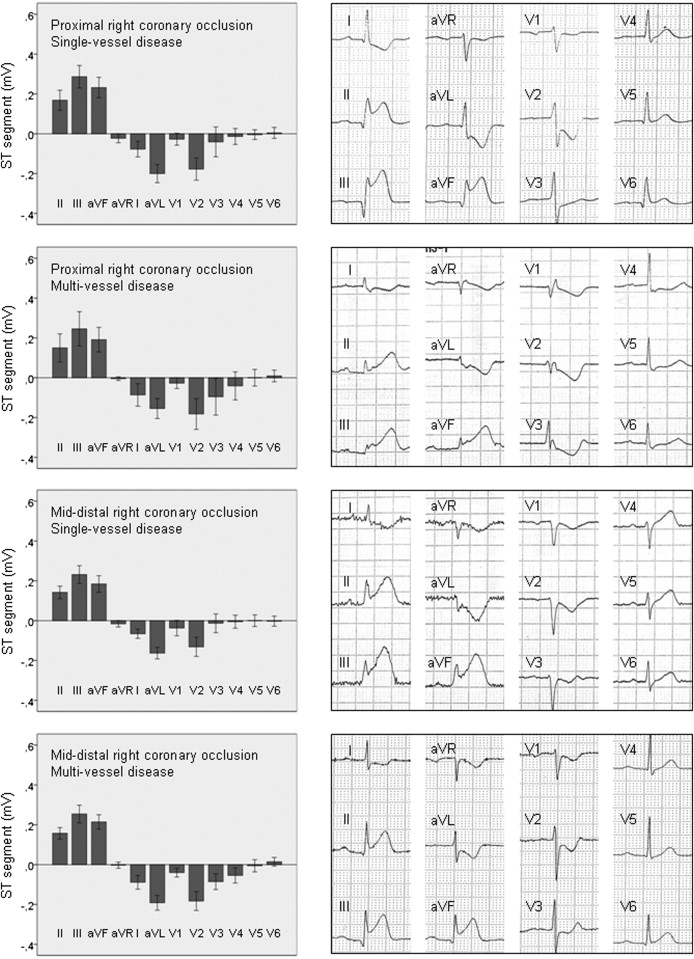
Proximal and mid-distal right coronary artery occlusion induced ST-segment elevation in leads II, III, and aVF, and reciprocal ST-segment depression in leads I, aVL, and V 2 in patients with either single or multivessel CAD ( Figure 3 ). In the latter cases, the reciprocal ST-segment changes extended to leads V 3 and V 4 (p = 0.02). The right ventricular branch was affected in 63 of the 118 patients with right coronary artery occlusion. The magnitude of ST-segment changes was comparable in patients with and without involvement of the right ventricular branch. Leads V 3 R and V 4 R were not routinely recorded.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


