Although cocaine ingestion may cause or contribute to myocardial infarction (MI), few contemporary data are available describing cocaine-associated MI. We describe the characteristics, management, and outcomes of patients with MI and recent cocaine use from the Acute Coronary Treatment and Intervention Outcomes Network Registry—Get With The Guidelines (ACTION Registry-GWTG) program. The study population was 102,952 patients enrolled in the American College of Cardiology ACTION Registry-GWTG from July 2008 to March 31, 2010 from 460 sites across the United States. Cocaine exposure was defined as self-reported cocaine use within the last 72 hours or a positive urine test for cocaine. Demographics and medical history, presenting characteristics, treatments, and in-hospital outcomes were reported on a standard case record form. A total of 924 patients (0.9%) were cocaine positive. Compared with cocaine-negative patients, cocaine-positive patients were younger and predominantly men with fewer cardiovascular risk factors. There was a higher percentage of ST elevation myocardial infarction (STEMI) (46.3% vs 39.7%) and cardiogenic shock at presentation in the cocaine-positive group, but the percentage of multivessel coronary artery disease was lower (53.3% vs 64.5%). Beta blockers within 24 hours (85.8% vs 90.1%, p <0.0001) and drug-eluting stents (40.1% vs 68.8%, p <0.0001 in patients with non-STEMI; 27.6% vs 54.6%, p <0.0001 in patients with STEMI) were used less commonly in cocaine-positive patients. Multivariable-adjusted in-hospital mortality was similar between cocaine-positive and cocaine-negative patients (adjusted odds ratio 1.00, 95% confidence interval 0.69 to 1.44, p value = 0.98). In conclusion cocaine-positive patients with acute coronary syndrome are younger with fewer risk factors, multivessel coronary artery disease and lower drug-eluting stent and β-blocker usage. Cocaine use was not associated with in-hospital mortality.
Cocaine-associated chest pain is commonly seen in emergency departments across America. Few data are available regarding the management of myocardial ischemia in cocaine users, and current recommendations for management of these patients are largely based on expert consensus. Moreover, little is known about the contemporary management of cocaine-associated myocardial infarction (MI), including treatment and outcomes. Registry databases therefore can provide useful insights into clinical features and management of these patients. Using data from the National Cardiovascular Data Registry Acute Coronary Treatment and Intervention Outcomes Network Registry—Get With The Guidelines (ACTION Registry-GWTG) program, we compared the clinical characteristics, contemporary in-patient management, and outcomes in patients with ST elevation myocardial infarction (STEMI) and non-STEMI among subjects who were using and not using cocaine before presentation.
Methods
The National Cardiovascular Data Registry ACTION Registry-GWTG is the largest quality improvement initiative focusing on patients admitted within 24 hours of acute MI. Random auditing of participating sites every year ensures data consistency and accuracy.
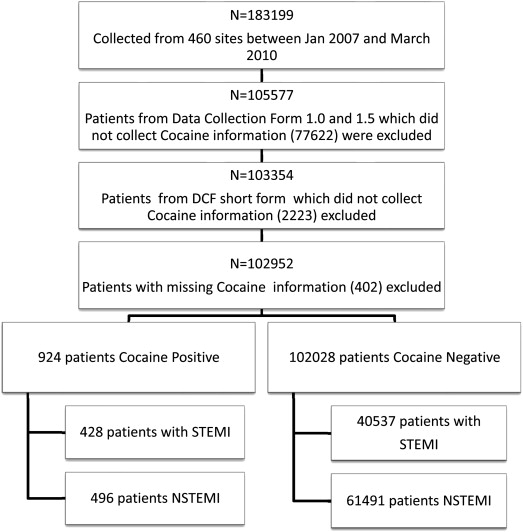
ACTION Registry-GWTG sites submit data from 270 clinical variables under the responsibility of a designated registry site manager at each participating institution. Coding for these variables is defined in data elements available on the National Cardiovascular Data Registry website for each registry. Cocaine exposure was added to the data collection form starting with version 2 in July 2008. Cocaine use is reported yes (cocaine positive) if the patient self-reports cocaine use within the last 72 hours or has a positive urine test for cocaine. Cocaine use is reported no (cocaine negative) if the patient self-reports no cocaine use, has a negative urine test for cocaine, or was not assessed for cocaine. Beta-blocker and other medication use during the first 24 hours of presentation is captured as “yes,” “no,” or “contraindicated.” This study evaluated all patients enrolled in the ACTION Registry-GWTG from January 2007 to March 31, 2010 with exclusions as mentioned ( Figure 1 ).
Categorical variables are summarized using percentages and were compared using Mantel-Haenszel chi-square test, whereas continuous variables are presented using median with interquartile range (twenty-fifth to seventy-fifth percentile) and compared using the Wilcoxon rank sum test. The association between in-hospital mortality and cocaine use was assessed using a multivariate logistic regression model with generalized estimating equations to account for clustering of observations from the same hospital. The variables used in the models for risk adjustment were adapted from the previously developed ACTION Registry-GWTG in-hospital mortality model that incorporates baseline characteristics at the time of presentation. The variables included were age; baseline serum creatinine level; systolic blood pressure at admission; baseline troponin ratio (compared with upper limit of normal); the presence of heart failure, cardiogenic shock, or both at admission; heart rate on admission (fitted as a linear spline with knot at 70 beats/min); electrocardiographic findings; and known history of peripheral arterial disease.
p Values <0.05 were considered statistically significant. All statistical analyses were performed at Duke Clinical Research Institute using SAS, version 9.2 (SAS Institute Inc., Cary, North Carolina).
Results
A total of 183,199 patients from 460 sites were documented in the registry during the study period. From this group, 77,662 patients with Data Collection Form versions 1.0 and 1.5 were excluded, as these versions of the form did not collect cocaine information. An additional 2,223 patients with data submitted using a limited data collection form were excluded as this form also did not collect cocaine information. Of the remaining patients, 402 had missing cocaine information and were excluded. This left 102,952 patients from 364 sites for the final analysis of which 924 patients (0.9%) were reported as cocaine positive.
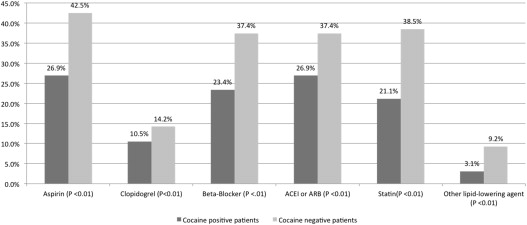
Compared with cocaine-negative patients, cocaine-positive patients were younger, more likely to be men, self-report African-American race, and had a lower body mass index. Although cocaine-positive patients were much more likely to smoke, other cardiac risk factors were less prevalent compared with cocaine-negative patients, as was the prevalence of known cardiac or vascular disease ( Table 1 ). Concurrent with decreased prevalence of risk factors, there was a lower rate of outpatient use of β blockers, angiotensin-converting enzyme inhibitors, and statins in the cocaine-positive patients before admission ( Figure 2 ).
| Variable | Cocaine Positive (n = 924) | Cocaine Negative (n = 102,028) | p Value |
|---|---|---|---|
| Age (yrs) | 50 (44.0–56.0) | 64 (54.0–76.0) | <0.01 |
| Women | 20.3 | 35.2 | <0.01 |
| Body mass index (kg/m 2 ) | 27.5 (24.1–31.6) | 28.3 (24.9–32.5) | <0.01 |
| White | 48.4 | 84.20 | <0.01 |
| Black | 45.3 | 8.7 | |
| HMO/private insurance | 25 | 56.8 | <0.01 |
| Medicare | 18.7 | 26.7 | |
| Medicaid | 15.8 | 3.5 | |
| Self/no insurance | 36.6 | 10.5 | |
| Recent smoker (<1 yr) | 79.3 | 35 | <0.01 |
| Hypertension | 64.8 | 71.2 | <0.01 |
| Dyslipidemia | 41.9 | 59.2 | <0.01 |
| Chronic lung disease | 10.7 | 14.1 | 0.00 |
| Diabetes mellitus | 23.2 | 30.5 | <0.01 |
| Previous MI | 27.4 | 25.3 | 0.14 |
| Previous heart failure | 11.9 | 12.5 | 0.62 |
| Previous percutaneous coronary intervention | 20.6 | 23.2 | 0.06 |
| Previous coronary bypass | 5.9 | 14.3 | <0.01 |
| Previous revascularization | 23.6 | 31.1 | <0.01 |
| Atrial fibrillation or flutter | 4.3 | 7.2 | 0.00 |
| Cerebrovascular disease | 8 | 11.6 | 0.00 |
| Peripheral arterial disease | 4.2 | 9.7 | <0.01 |
| Body mass index ≥30 kg/m 2 | 34.2 | 38 | 0.01 |
| Electrocardiographic findings | |||
| STEMI | 46.3 | 39.7 | <0.01 |
| ST depression or transient ST elevation | 11.1 | 15.3 | |
| T-wave inversion | 9.8 | 9 | |
| None | 32.7 | 35.9 | |
| Signs of CHF | 16.2 | 15.6 | 0.62 |
| Cardiogenic shock at first contact | 13 | 4.4 | <0.01 |
| Systolic blood pressure on admission (mm Hg) | 140 (120–162) | 144 (123–164) | 0.05 |
| Heart rate on admission (beats/min) | 84 (70–101) | 81 (69–96) | 0.00 |
| Tachycardia (rate >100/min) | 25.3 | 19.9 | <0.01 |
| Laboratory results | |||
| Initial creatinine level (mg/dl) | 1.1 (0.9–1.3) | 1.1 (0.9–1.3) | 0.07 |
| Glomerular filtration rate | 80.6 (62.7–98.3) | 70.7 (53.2–87.6) | <0.01 |
| Initial Hgb (g/dl) | 14.3 (13.2–15.6) | 14.0 (12.6–15.3) | <0.01 |
| Hemoglobin A 1c (%) | 6 (5.6–7.5) | 6.2 (5.7–7.5) | 0.04 |
| High-density lipoprotein (mg/dl) | 37 (30–45) | 36 (30–44) | 0.04 |
| Low-density lipoprotein (mg/dl) | 101 (75–128) | 98 (73–125) | 0.01 |
There were no appreciable differences in time from symptom onset to arrival at a health-care facility between the 2 groups. There were no significant differences in systolic blood pressure at presentation, although heart rates were generally higher with a larger percentage of patients having tachycardia in the cocaine-positive group. On presentation, a higher percentage of STEMI and cardiogenic shock was seen in the cocaine-positive subgroup. The proportion of patients with signs of congestive heart failure (CHF) at presentation was similar when comparing the entire cohort ( Table 1 ). However, in a subset analysis of patients with STEMI, a significantly higher percentage with cocaine use showed signs of CHF at presentation (15.9% vs 9.3%, p <0.0001).
Among patients with STEMI, there were no differences in rates of reperfusion whether using primary percutaneous coronary intervention or fibrinolysis between cocaine-positive and negative patients. Although cocaine-positive patients were slightly more likely to undergo coronary angiography, they were slightly less likely to receive a stent, and markedly less likely to receive a drug-eluting stent among patients undergoing primary percutaneous coronary intervention with stent ( Table 2 ).
| Variable | Cocaine Positive (n = 428) | Cocaine Negative (n = 40,537) | p Value |
|---|---|---|---|
| Noninvasive stress testing | 6.2 | 4.5 | 0.01 |
| Diagnostic catheterization | 85.8 | 83.6 | 0.06 |
| Catheterization within 24 h of arrival | 93 | 90.1 | 0.02 |
| No. of diseased vessels on catheterization | |||
| 0 | 5.3 | 2.3 | <0.01 |
| 1 | 39.1 | 34.8 | |
| 2 | 31.2 | 32.9 | |
| 3 | 23.9 | 29.5 | |
| LVEF | |||
| ≥50% | 46.5 | 49.2 | 0.21 |
| 40%–50% | 23.7 | 25.4 | |
| 25%–40% | 21.5 | 19.5 | |
| <25% | 6.9 | 4.7 | |
| Reperfusion strategy in STEMI | |||
| Overall reperfusion | 92.7 | 93.9 | 0.54 |
| Thrombolytic therapy | 9.3 | 12 | 0.13 |
| Primary PCI | 84.1 | 83.7 | 0.77 |
| Primary PCI stented | 86.9 | 91.3 | <0.01 |
| Bare-metal stent | 73.2 | 46.1 | <0.01 |
| Drug-eluting stent | 27.6 | 54.6 | <0.01 |
| PCI for STEMI (primary, facilitated, rescue, or subsequent) | 84.4 | 88.1 | 0.03 |
| Revascularization in STEMI | 87.6 | 92.2 | <0.01 |
| Coronary artery bypass grafting | 7.5 | 9.2 | 0.07 |
| In-hospital clinical events | |||
| Death | 6.2 | 5.8 | 0.73 |
| Death within 24 h of arrival | 1.4 | 1.9 | 0.47 |
| Postadmission infarction | 1.2 | 1 | 0.74 |
| Death or MI | 7.2 | 6.6 | 0.62 |
| Cardiogenic shock (new onset in facility) | 6 | 6.3 | 0.75 |
| CHF | 4.1 | 6.5 | 0.04 |
| Stroke | 0.5 | 0.8 | 0.42 |
| Hemorrhagic stroke in patients with stroke | 50 | 19 | 0.27 |
| Suspected bleeding event | 6.4 | 5.6 | 0.44 |
In the population without STEMI, a slightly greater proportion of cocaine-positive patients underwent noninvasive stress testing, but rates of cardiac catheterization were high overall and similar between the 2 groups. In contrast, there were markedly lower rates of drug-eluting stent use. Compared with the STEMI subgroup, the cocaine-positive subgroup without STEMI had a greater proportion of patients with multivessel coronary artery disease (CAD) than the cocaine-negative subgroup ( Table 3 ).
| Variable | Cocaine Positive (n = 496) | Cocaine Negative (n = 61,491) | p Value |
|---|---|---|---|
| Noninvasive stress testing | 8.1 | 5.60 | 0.02 |
| Diagnostic catheterization | 76.4 | 77 | 0.79 |
| Catheterization within 24 h of arrival | 44.1 | 47.6 | 0.12 |
| No. of diseased vessels on catheterization | |||
| 0 | 14.8 | 7.2 | <0.01 |
| 1 | 25.8 | 33.0 | |
| 2 | 29 | 25.6 | |
| 3 | 37 | 25.9 | |
| LVEF | |||
| ≥50% | 57 | 57.10 | 0.03 |
| 40%–50% | 16.3 | 19.8 | |
| 25%–40% | 17.1 | 16.5 | |
| <25% | 8.20 | 5.3 | |
| Percutaneous coronary intervention (PCI) | 38.9 | 44.5 | 0.01 |
| PCI within 24 h of arrival | 23.8 | 29.1 | 0.01 |
| PCI stented | 91.7 | 92.2 | 0.73 |
| Bare-metal stent | 59.3 | 32.2 | <0.01 |
| Drug-eluting stent | 40.1 | 68.8 | <0.01 |
| Revascularization | 46.6 | 54.7 | <0.01 |
| Medically managed | 23.2 | 22.5 | <0.01 |
| Medically managed after catheterization | 30 | 22.5 | |
| Bypass surgery | 8.1 | 10.9 | |
| In-hospital clinical events | |||
| Death | 2.1 | 3.9 | 0.04 |
| Death within 24 h of arrival | 0 | 0.7 | 0.07 |
| Postadmission infarction | 0.8 | 0.9 | 0.82 |
| Death or MI | 2.8 | 4.6 | 0.06 |
| Cardiogenic shock (new onset in facility) | 3.2 | 2.8 | 0.61 |
| CHF | 6.6 | 6.9 | 0.81 |
| Stroke | 0.8 | 0.7 | 0.75 |
| Hemorrhagic stroke in patients with stroke | 25 | 9.7 | 0.18 |
| Suspected bleeding event | 3.2 | 4.9 | 0.09 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


