We evaluated the influence of coronary computed tomographic angiography (CTA) as a first-line diagnostic test on patient treatment and prognosis. A total of 1,055 consecutive patients with suspected stable angina pectoris (mean age 55 ± 10 years, 56% women) and a low to intermediate pretest likelihood of coronary artery disease (CAD) were included in the present study. The patients were followed for a median of 18 months. The use of downstream diagnostic testing and medical therapy after CTA were recorded. The CTA result was normal in 49%, and nonobstructive and obstructive CAD (≥50% stenosis) was demonstrated in 31% and 15% of the patients, respectively. Coronary CTA was inconclusive in 5% of the patients. The use of antiplatelet therapy decreased with normal findings from CTA, and the use of antiplatelet and lipid-lowering agents increased in patients with CAD. Additional testing was performed in 2% of patients with normal CTA findings and in 7% and 82% of patients with nonobstructive or obstructive CAD, respectively. No patients without CAD, 0.9% of patients with nonobstructive CAD, and 1.9% of patients with obstructive CAD met the primary end point (cardiovascular death and myocardial infarction, p = 0.008). No patients without CAD, 1.5% of patients with nonobstructive CAD, and 30% patients with obstructive CAD met the secondary end point (cardiovascular death, myocardial infarction, and coronary revascularization, p <0.0001). In conclusion, in patients suspected of having angina, the findings from CTA influence patient treatment without resulting in excessive additional testing. Coronary CTA provides important prognostic information, with excellent intermediate-term outcomes in patients with normal CTA findings.
Consistent, high-diagnostic performance of coronary computed tomographic angiography (CTA) has been demonstrated in patients suspected of having coronary artery disease (CAD). Although CTA has been proposed as an appropriate noninvasive diagnostic test in symptomatic patients with a low to intermediate pretest likelihood of significant CAD, no universal agreement of its mainstream diagnostic use has been established. Also, the clinical benefit of CTA has been questioned, because this modality seems to identify more patients with coronary atherosclerosis than do conventional functional tests and, thus, introduces the risk of unnecessary additional diagnostic and therapeutic procedures. However, data on disease management, including downstream testing and therapy after a CTA based diagnostic strategy have been limited. To further delineate the role of CTA in contemporary practice, the expansion of current data on CTA outcomes in relation to downstream patient management and prognosis is essential. The aim of the present study was to assess the influence of CTA on patient treatment and prognosis in patients with suspected angina pectoris.
Methods
Coronary CTA has been used as the preferred frontline diagnostic test in outpatients with suspected angina pectoris and a low to intermediate pretest likelihood of CAD at our institution since 2007. Patients with a high pretest risk of CAD are preferably referred for invasive coronary angiography (ICA), with myocardial perfusion imaging, stress testing, or ICA considered in patients with contraindications to CTA (i.e., renal insufficiency, contrast allergy, extreme obesity, pregnancy). Before testing, the patients were evaluated by cardiologists with 12-lead electrocardiography and echocardiography. All patients suspected of having stable angina pectoris and referred for CTA at our institution from March 1, 2007 and March 31, 2009 were consecutively included in the present study. Patients with known CAD, heart failure, arrhythmia, or recent acute coronary syndrome were excluded. The Danish Data Protection Agency approved the study, with a waiver for individual informed consent from the regional ethical committee.
Symptoms, medical history, current medication, and standard cardiovascular (CV) risk factors were prospectively recorded. The symptoms were categorized into typical, atypical angina or nonanginal pain. The traditional CV risk factors were categorized, as previously described. The patients were classified according to age, gender, and symptoms into low (<13.4%), intermediate or high (>87.2%) pretest likelihood of significant CAD (≥50% coronary artery lumen reduction).
Coronary CTA was performed using a 64-slice dual-source CT scanner (Somatom Definition, Siemens Medical Solution, Forcheim, Germany), as previously reported. In brief, a prospective electrocardiogram-gated, sequential, nonenhanced scan was acquired, and an Agatston score was established (syngo calcium scoring, Siemens Medical Solution). Coronary CTA was performed with tube current modulation when possible and with lower tube voltage (100 kV) in patients weighing <85 kg. The radiation exposure for the nonenhanced scan and CTA was estimated from the dose-length product multiplied by a chest region conversion factor (0.014 mSv · mGy −1 · cm −1 ). All scans were assessed using axial images and multiplanar reconstructions by expert observers and reported as normal (no CAD), nonobstructive CAD, obstructive CAD (≥50% lumen reduction), or inconclusive (≥1 nonevaluable segment in the absence of obstructive CAD).
The decision to proceed with CTA after the initial nonenhanced scan was determined primarily from the Agatston score and heart rate at the discretion of the scan-performing cardiologist. In general, an Agatston score of >400 and/or heavily proximal coronary calcification was considered limiting for the diagnostic performance of CTA. Decisions on medical treatment and referral for additional testing were determined by patient symptoms, clinical examination, and the CTA result, at the discretion of the referring cardiologist. Medical therapy before CTA and changes according to the CTA result were recorded from the electronic patient files. Patients in whom CTA was not performed because of extensive coronary calcification were considered to have an increased risk of significant CAD and were preferably referred for ICA, as were patients with obstructive CAD. Patients with an inconclusive CTA result were referred for additional testing on the basis of their symptoms, risk profile, and Agatston score at the discretion of the referring cardiologist. If obstructive CAD was demonstrated using ICA, the cardiologists and cardiac surgeons at the local university center reviewed the invasive angiographic findings and relevant clinical information, and reached a consensus concerning therapy.
The median interval of follow-up was 18 months (interquartile range 14 to 25, range 9 to 34). The follow-up data, including downstream testing, coronary interventions, and serious cardiac events, were obtained from the patient records, National Patient Registry, Civil Registration System, and National Causes of Death Registry. All-cause and CV death, nonfatal myocardial infarction, and coronary revascularization were registered. No patients were lost to follow-up. The composite primary end point included CV death and nonfatal myocardial infarction. The composite secondary end point included CV death, nonfatal myocardial infarction, and coronary revascularization. The primary end point was adjudicated from the patient records and death certificates by 2 cardiologists who were unaware of the patient demographics and CTA findings.
Continuous data are presented as mean ± SD or median (interquartile range, range) and analyzed using unpaired 2-sided t test or Wilcoxon-Mann-Whitney test, as appropriate. Categorical data are presented as numbers (proportions) and analyzed using Fisher’s exact test. Individual changes in medical therapy after CTA were analyzed using McNemar’s test. Kaplan-Meier curves stratified according to the CTA findings were constructed among patients with a conclusive CTA result. Comparisons of event-free survival were performed using log-rank statistics. Cox hazard regression analyses were performed to evaluate the association between baseline covariates/CTA findings and clinical outcome. The assumption of proportional hazards was not fulfilled when the group with normal CTA findings was included. The Cox hazard regression analyses were therefore confined to patients with nonobstructive and obstructive CAD. Owing to the limited number of primary end points, these analyses were restricted to the secondary end point. A crude hazard ratio with 95% confidence intervals was computed. The change-in-estimate method was applied to identify possible confounding factors among the characteristics presented in Table 1 . A change in the crude hazard ratio of >10% for the association of CTA findings and outcome was considered to reflect the presence of a confounder. Because early coronary revascularization (<3 months) may be considered precipitated by the CTA result per se, additional secondary end point analyses were performed in which patients were censored at the occurrence of early revascularization. A 2-tailed p value <0.05 was considered significant. Statistical analyses were performed using STATA\IC, version 10 (StataCorp, College Station, Texas).
| Variable | All Patients (n = 1,154) | Normal CTA (n = 516) | Nonobstructive CAD (n = 327) | Obstructive CAD (n = 161) | Inconclusive CTA (n = 51) | Calcium Score Scan (n = 99) |
|---|---|---|---|---|---|---|
| Women | 634 (55%) | 325 (63%) | 162 (50%) | 69 (43%) | 35 (69%) | 43 (43%) |
| Age (years) | 56 ± 11 | 52 ± 10 | 59 ± 9 | 59 ± 11 | 55 ± 11 | 63 ± 10 |
| Body mass index (kg/m 2 ) | 26 ± 4 | 26 ± 6 | 27 ± 4 | 26 ± 4 | 26 ± 4 | 27 ± 5 |
| Family history of premature CAD | 536 (46%) | 230 (45%) | 147 (45%) | 88 (55%) | 28 (55%) | 43 (43%) |
| Hypertension | 476 (41%) | 165 (32%) | 145 (44%) | 85 (53%) | 22 (43%) | 59 (60%) |
| Hypercholesterolemia | 625 (54%) | 219 (42%) | 204 (62%) | 106 (66%) | 31 (61%) | 65 (66%) |
| Diabetes mellitus | 69 (6%) | 17 (3%) | 15 (5%) | 23 (14%) | 3 (6%) | 11 (11%) |
| Current smoker | 302 (26%) | 134 (26%) | 68 (21%) | 58 (36%) | 14 (27%) | 28 (28%) |
| Ischemia test before computed tomographic angiography | 162 (14%) | 85 (16%) | 41 (13%) | 25 (16%) | 3 (6%) | 8 (8%) |
| Positive ischemia test before computed tomographic angiography | 67 (6%) | 40 (8%) | 13 (4%) | 12 (7%) | 1 (2%) | 1 (1%) |
| Negative ischemia test before computed tomographic angiography | 73 (6%) | 35 (7%) | 23 (7%) | 8 (5%) | 6 (12%) | 1 (1%) |
| Inconclusive ischemia test before computed tomographic angiography | 22 (2%) | 10 (2%) | 5 (2%) | 5 (1%) | 1 (2%) | 1 (1%) |
| Nonanginal chest pain | 638 (55%) | 315 (61%) | 197 (60%) | 70 (43%) | 24 (47%) | 32 (32%) |
| Atypical angina pectoris | 406 (35%) | 168 (33%) | 95 (29%) | 73 (45%) | 25 (49%) | 45 (45%) |
| Typical angina pectoris | 64 (6%) | 17 (3%) | 22 (7%) | 14 (9%) | 2 (4%) | 10 (10%) |
| Dyspnea ⁎ | 46 (4%) | 16 (3%) | 13 (4%) | 4 (2%) | 0 (0%) | 12 (12%) |
| Pretest likelihood of coronary artery disease | ||||||
| Median | 22 | 19 | 22 | 28 | 22 | 54 |
| Interquartile range | 14–54 | 8–32 | 19–54 | 19–59 | 8–46 | 28–67 |
| Low (<13.4%) | 277 (24%) | 188 (36%) | 43 (13%) | 22 (14%) | 17 (33%) | 7 (7%) |
| Intermediate | 833 (72%) | 320 (62%) | 265 (81%) | 131 (81%) | 32 (63%) | 85 (86%) |
| High (>87.2%) | 44 (4%) | 8 (2%) | 19 (6%) | 8 (5%) | 2 (4%) | 7 (7%) |
⁎ Dyspnea considered as angina equivalent; ischemia testing before CTA included exercise stress testing (n = 136), myocardial perfusion imaging (n = 20) or both (n = 6).
Results
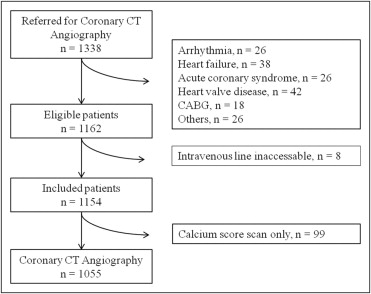
A total of 1,162 patients met the inclusion criteria ( Figure 1 ). The patient characteristics are presented in Table 1 . Eight patients (1%) were excluded because of an inaccessible intravenous line. In 99 patients (9%) only a calcium scan was performed owing to elevated Agatston scores (n = 73) and/or arrhythmias (n = 12) or other causes (n = 14). The median Agatston score for these patients was 557 (interquartile range 271 to 948, range 0 to 4,264). Coronary CTA was inconclusive in 51 patients (5%) because of respiratory artifacts (n = 4), poor contrast enhancement (n = 3), or motion artifacts (n = 44). The median Agatston score for patients completing a CTA study was 0 (interquartile range 0 to 26, range 0 to 1,616). An ischemia test was performed <6 months before CTA in 162 patients (14%; an exercise test in 136, myocardial perfusion imaging in 20, and both in 6). The patients in whom an ischemia test had been performed were younger (53 ± 11 years vs 57 ± 11 years, p <0.001), had a lower median pretest likelihood of CAD (19% vs 22%, p <0.001), and less frequently had hypercholesterolemia (38% vs 57%, p <0.001) than the rest of the study cohort. Otherwise, no differences in patient demographics or risk profile were demonstrated between the 2 groups. The mean ± SD estimated radiation dose was 1.6 ± 1 mSv for the calcium score scans and 6.6 ± 4 mSv for the CTA studies.
Information on medical therapy before and after CTA according to the scan result is listed in Table 2 . The use of antiplatelet therapy was significantly reduced after normal CTA findings. The use of antiplatelet and lipid-lowering therapy increased in patients with CAD. The diagnostic consequences of CTA are listed in Table 3 . In 83 patients with a calcium scan only, ICA detected obstructive CAD in 41 (49%), 1-vessel disease (VD) in 21 patients, 2-VD in 14 patients, and 3-VD in 6 patients. Of the 843 patients with a normal CTA result or with nonobstructive CAD, ICA was performed in 13 (2%), in whom the absence of obstructive CAD was confirmed. In patients with obstructive CAD at CTA, ICA confirmed this in 61 (50%) of 121 patients, 1-VD in 43 patients, 2-VD in 12 patients, and 3-VD in 6 patients. In patients with an inconclusive CTA result, ICA detected obstructive CAD in 2 (9%) of 23 patients, 1-VD in 1, and 3-VD in 1 patient. No differences in the proportions of downstream testing in patients with or without an ischemia test before CTA could be demonstrated. The clinical outcome according to the CTA result is presented in Table 4 . Kaplan-Meier curves for the event-free survival according to the CTA findings are presented in Figure 2 . Patients with nonobstructive CAD or obstructive CAD more frequently met the primary end point than did the patients without CAD (log-rank, p = 0.008). The secondary end point was more frequent in patients with obstructive CAD than in patients with a normal CTA result or nonobstructive CAD with or without early revascularization included in the analyses (log-rank, p <0.0001). The cumulative event-free survival rate for the secondary end point was 100%, 98.5%, and 70%, with 100%, 98.5%, and 88% censoring for early revascularization in patients with a normal CTA result, nonobstructive CAD, and obstructive CAD, respectively. The crude hazard ratio for the occurrence of the secondary end point was 22.8 (95% confidence interval 9.1 to 57.3) and 10.2 (95% confidence interval 3.8 to 27.3) censoring patients undergoing early revascularization. One patient with nonobstructive CAD died from an unknown cause. Classifying this event as CV death did not significantly change the results. None of the baseline variables acted as confounders for the association between the CTA findings and the clinical outcomes. No significant difference was found in the clinical outcome in patients with or without an ischemia test before CTA.
| Variable | Patients (n) | Antiplatelet Therapy ⁎ | Lipid-Lowering Therapy | β-Blocking Agents | ACEI/ARB | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before † | After † | p Value | Before † | After † | p Value | Before † | After † | p Value | Before † | After † | p Value | ||
| Normal computed tomographic angiographic findings | 516 | 231 (45%) | 122 (24%) | <0.001 | 134 (26%) | 136 (26%) | 0.68 | 126 (24%) | 98 (19%) | <0.001 | 83 (16%) | 79 (15%) | 0.10 |
| Nonobstructive coronary artery disease | 327 | 170 (52%) | 275 (84%) | <0.001 | 128 (39%) | 268 (82%) | <0.001 | 79 (24%) | 78 (24%) | 0.80 | 85 (26%) | 82 (25%) | 0.18 |
| Obstructive coronary artery disease ‡ | 161 | 101 (63%) | 151 (94%) | <0.001 | 74 (46%) | 146 (91%) | <0.001 | 48 (30%) | 72 (45%) | <0.001 | 49 (30%) | 47 (29%) | 0.41 |
| Inconclusive computed tomographic angiographic findings | 51 | 23 (45%) | 31 (61%) | 0.02 | 16 (31%) | 25 (49%) | 0.003 | 14 (27%) | 17 (33%) | 0.083 | 12 (24%) | 12 (24%) | 1.0 |
| Calcium score scan | 99 | 59 (60%) | 82 (83%) | <0.001 | 44 (44%) | 80 (81%) | <0.001 | 28 (28%) | 35 (35%) | 0.008 | 34 (34%) | 33 (33%) | 0.32 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


