Inferior Vena Cava Filter Removal
OLUFUNMI ONAOPEMIPO AWONUGA and MARC A. PASSMAN
Presentation
A 28-year-old woman with a history of morbid obesity, 10-pack-year history of smoking, and hypertension presents for a follow-up regarding her inferior vena cava (IVC) filter. An optional IVC filter was placed during admission to the trauma intensive care unit following a motor vehicle accident 2 months ago. Her injuries consisted of intraparenchymal hemorrhage, subdural hemorrhage, grade IV liver laceration, multiple rib fractures, and right hemopneumothorax, which precluded pharmacologic thromboprophylaxis with anticoagulation at that time. She was in the intensive care unit and was on a ventilator for 10 days, during which time a deep vein thrombosis (DVT) was identified on ultrasound without evidence of pulmonary embolism (PE) on additional imaging. An optional IVC filter was placed due to relative contraindications to therapeutic anticoagulation due to her injuries. It has been 30 days since IVC filter placement, and she has been home for 2 weeks, ambulating without difficulty. She presents for IVC filter removal consideration.
Discussion
Systemic anticoagulation is primary standard therapy for DVT and PE based on evidence-based guidelines from the American College of Chest Physicians (ACCP), with IVC filter placement reserved for patients with documented DVT or PE and a contraindication to anticoagulation, complication of anticoagulation, or recurrent venous thromboembolism (VTE) despite therapeutic anticoagulation. The recommendations are controversial for IVC filter use as prophylaxis in patients without documented DVT but at high risk due to medical conditions, such as trauma or critically illness, when primary pharmacologic thromboprophylaxis is not feasible secondary to bleeding risk. While ACCP recommends against prophylactic IVC filter use, the Eastern Association for the Surgery of Trauma (EAST) and the Society for Interventional Radiology (SIR) guidelines support selected use of IVC filter placement for VTE prophylaxis.
There are multiple different FDA-approved and commercially available filter designs (Table 1). When an IVC filter is placed, decision should be made regarding permanent versus optional filter placement based on perceived duration of filter need. Although all optional filters also carry an FDA indication for permanent use, if a permanent need is determined at time of placement, a filter specific to permanent use is preferred, while optional filters should be considered if a temporary need is determined. Patients chronically at high risk of clinically significant PE irrespective of management with primary therapy, short life expectancy, or noncompliance with primary therapy or follow-up appointments should have a permanent filter placed.
TABLE 1. Key Technical Steps and Potential Pitfalls
Known long-term risks associated with IVC filters include, but are not limited to, access site thrombosis, filter fracture, filter migration, filter embolization, and IVC perforation. Between 2005 and 2010, the FDA received 921 device adverse event reports involving IVC filters, of which 328 involved device migration, 146 involved embolizations (detachment of device components), 70 involved perforation of the IVC, and 56 involved filter fracture. Some of these events led to adverse clinical outcomes in patients. The FDA recommends retrievable IVC filters be removed as soon as protection from PE is no longer needed.
Several studies have indicated that a variable percentage of optional IVC filters are actually removed, ranging between 20% and 80%, with higher follow-up reported with actively managed protocols. If an optional filter is used, it should be placed with intention of retrieval, with a retrieval timeline determined at the time of placement. The time frame within which a filter should be retrieved is recommended for each device based on FDA indications for use (IFUs), but in practice is poorly defined. Recommended retrieval time frames for each filter vary significantly, and understanding of optimal retrieval times is important prior to placement. In general, an earlier time frame is associated with higher retrieval success rates and planned retrieval should be as soon as clinically indicated. Using standard timelines and retrieval techniques, 80% to 100% of filter retrieval attempts will be successful.
Workup
The patient undergoes a focused history and physical examination. She is fully ambulatory with no residual disabilities from her trauma. She did not have any planned procedures upcoming in the future. She has been wearing compression stockings and had no lower extremity swelling or evidence of venous congestion in her lower extremities. A lower extremity venous duplex ultrasound was performed that showed no evidence of residual DVT. Abdominal x-ray showed that a conical filter was upright in anatomic position within the IVC, right side of vertebral bodies with apical hook tip at L2-3 level, full expansion of base of filter, without tilt or filter leg distortion. Serum laboratory studies reveal a hemoglobin of 13 g/dL, a platelet count of 200,000, and a creatinine of 0.6 mg/dL.
Discussion
According to the SIR, IVC filters may be removed when the indication for the IVC filter is no longer present and/or when anticoagulation either therapeutic or prophylactic can be used based on decreasing potential for bleeding risk. Filters should be removed when the risk of clinically significant PE is acceptably low as a result of improved clinical status with decreased VTE risk, or achievement of sustained appropriate primary VTE treatment with anticoagulation and no further indication for filter need. Appropriate primary VTE treatment will vary depending on the VTE risk status of the patient. Patients should demonstrate the ability to tolerate sustained primary VTE treatment before removal of the filter. The period of time required will vary based on the patient’s clinical and functional status and ability to resume evidence-based standard therapy for VTE. Prior to discontinuation of the IVC filter, one should assure that the patient is not anticipated to return to a high-risk state for VTE because of interruption of primary treatment, change in clinical management, or change in clinical condition. The life expectancy of the patient should be long enough that the presumed benefits of discontinuation of filtration can be realized. Limited evidence suggests that some complications of filters may take years to manifest. Patients not anticipated to survive more than 6 months are unlikely to derive any discernible benefit from filter retrieval.
Prior to IVC filter retrieval, workup should include a physical examination to assess for signs of DVT. Lower extremity venous duplex ultrasound is performed prior to filter removal to confirm the presence or absence of DVT. A finding of a DVT on lower extremity venous duplex ultrasound requires initiation of anticoagulation therapy prior to filter removal. If patients are already on therapeutic anticoagulation for documented DVT, there should be consideration of conversion to a low molecular weight heparin bridge prior to filter retrieval with resumption of longer-acting oral anticoagulation postretrieval. Patients who require laboratory monitoring for anticoagulation should have stable measurements with no evidence of bleeding for at least 7 days before the discontinuation procedure. Patients with established VTE should not have clinical or objective evidence of failure or a complication of primary therapy before filter retrieval. Otherwise, continued IVC filter, possibly permanently, may be warranted.
Diagnosis and Treatment
Prior to IVC retrieval, the integrity of the IVC filter should be radiographically confirmed to make sure that there are no filter-related problems that would render retrieval technically challenging or impossible with endovascular techniques. Filter positioning and anatomic characteristics that are commonly cited as predictors of failure are filter tilt, caval penetration, and caval angulation. The most powerful predictors of failure in multiple studies have been hook apposition to the caval wall and increased filter dwell time.
Venography of the vena cava and implanted filter is performed at the time of the retrieval procedure. Position of the filter retrieval hook relative to the IVC wall and potential angulation issues are determined. Substantial filling defects present within the filter indicating clot preclude successful filter retrieval, and the procedure should be discontinued.
Case Continued
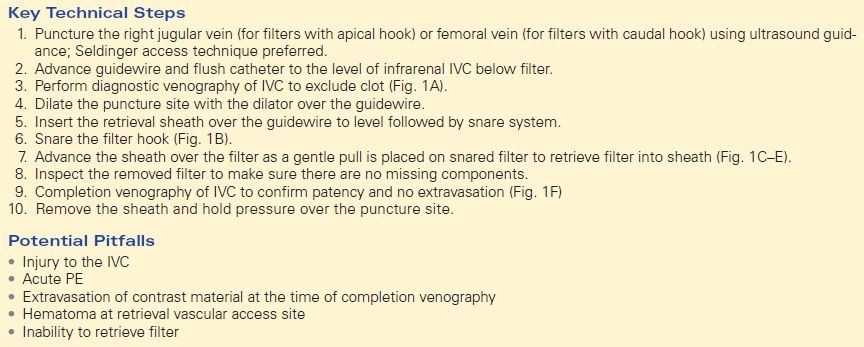
The patient was brought to the Endo Suite. She was placed supine on the operating room table. Intravenous sedation was provided. The right neck was prepped and draped in usual sterile fashion. With ultrasound guidance, the patency of the right internal jugular vein was confirmed, and with real-time imaging, a single puncture needle access was obtained using micropuncture needle, wire, and sheath. Sheath was then upsized to a 5-French sheath. A 0.035-inch glide wire was advanced down into the infrarenal IVC, followed by a flush catheter. Digital subtraction venography was performed with findings of an IVC filter in straight alignment to the IVC wall, apical hook at the level of the renal veins, and no evidence of filling defects within the filter device.
Surgical Approach
Depending on the type of optional IVC filter used, different approaches and techniques are required for filter removal and providers should be familiar with specific filter retrieval techniques and kits as per each device’s IFUs. Most filters require percutaneous access from either jugular approach or femoral approach, with need to engage the filter retrieval hook with a snare. Once the filter hook is engaged, the snared filter is retracted into an appropriately sized sheath (Table 1). Independent of filter type, during the retrieval process, difficulty releasing the filter from the IVC attachment may occur, and retrieval should be aborted if the filter does not release with modest tension. Retrieved filters should be inspected for integrity, directly and with postretrieval imaging to make sure there are no retained filter components (1).
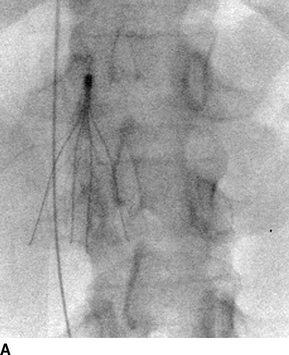
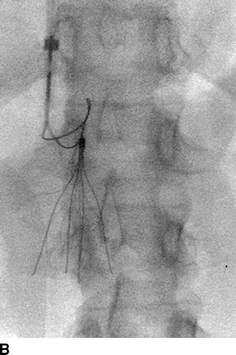
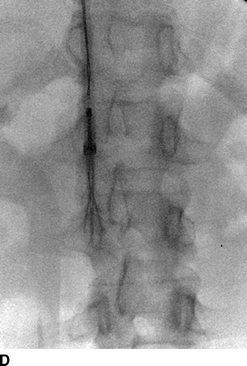
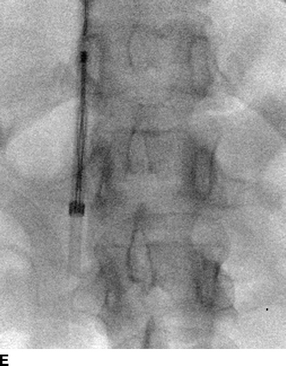

FIGURE 1 A: IVC filter in place with guidewire in the vena cava. B: Snare capture of the IVC filter apical hook. C: Advance the sheath over the filter. D, E:Retracting filter into sheath. F: Completion venogram.



