Common Syndromes in Pulmonary Infectious Diseases |
Upper respiratory tract infections are the most common infections and the most frequent reasons for office visits in the United States. Most upper respiratory infections are minor and self-limiting and do require specific antimicrobial therapy, but some (e.g., peritonsillar abscess [PTA], epiglottitis, invasive fungal sinusitis) may be life-threatening.1
THE COMMON COLD
The common cold is a mild, self-limiting infection and is the most frequent acute illness in the United States.2 Approximately 500 million noninfluenza viral respiratory infections occur yearly, resulting in estimated direct costs of $17 billion and indirect costs of $22.5 billion annually.3 Six major viral families are responsible: rhinovirus (30%–40% of cases); influenza virus (25%–30%); coronavirus (10%–15%); adenovirus (5%–10%); parainfluenza virus (5%); and respiratory syncytial virus (RSV) (5%). Each virus has several serotypes; rhinovirus has 100. More recently recognized viruses, such as human metapneumovirus and bocavirus can also cause the common cold.4 Adults have an average of two to four colds and children six to eight colds per year.
In the United States, the incidence of colds is seasonal, with most occurring fall through spring. Young children are the main reservoir of respiratory viruses, and adults with children have more colds than those without. Transmission probably occurs either by inhalation of infectious droplets or by hand-to-nose “self-inoculation” after touching infectious secretions. The pathogenesis of rhinovirus infections is thought to include viral entry into the nose followed by infection of the epithelial cells of the upper airway. Frequent use of alcohol-based hand sanitizers or virucidal impregnated nasal tissues may reduce transmission.5 Symptoms (sneezing, nasal discharge and congestion, and a “scratchy” throat) develop 16 to 72 hours after inoculation, and last for 1 to 2 weeks. Fever is uncommon in adults but may occur in children. Acute viral bronchitis is commonly associated with the common cold in adults. The peak of rhinoviral excretion in nasal secretions coincides with the peak of clinical illness. Complications of the common cold include bacterial superinfections of the upper respiratory tract, such as acute otitis media (AOM) and acute sinusitis, and exacerbations of asthma.6
Treatment of the common cold is symptomatic. Symptoms of rhinorrhea and sneezing may be improved by the use of intranasal ipratropium.7 Antihistamine use alone in patients with the common cold is of minimal benefit and frequently results in troublesome side effects.8 Guidelines from the American College of Chest Physicians do not recommend use of cough suppressants (codeine or dextromethorphan) for cough associated with upper respiratory infections.9 Treatment with antibiotics for uncomplicated upper respiratory tract infections causes more harm than benefit and should not be used.10,11 The value of zinc, vitamin C, Echinacea, and other herbal products has not been definitely proven.12–14 Careful hand washing and use of hand disinfectants may be the most effective preventive measures.15
PHARYNGITIS
Acute pharyngitis is one of the most frequent illnesses for which physicians are consulted, with an estimated 12 million visits per year in the United States.16 The great majority of cases are caused by viruses and often occur as part of the common cold for which antimicrobial therapy is not warranted. These cases are mild, nonexudative, and self-limiting.
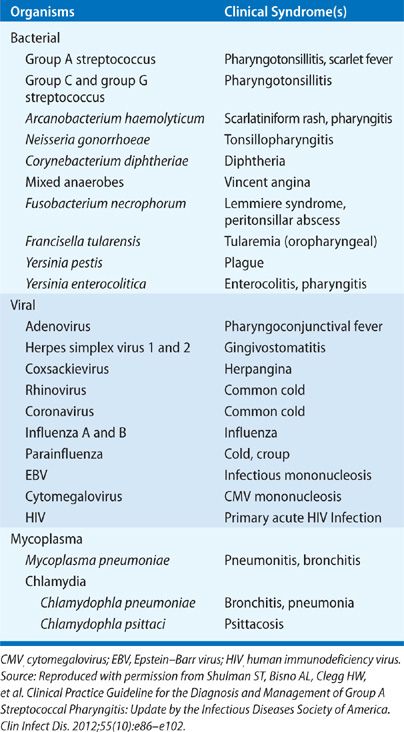
The major causes of pharyngitis are listed in Table 126-1. Bacterial agents other than Group A streptococcus (GAS) that may cause pharyngitis include Mycoplasma pneumoniae, Chlamydia pneumoniae, Neisseria gonorrhoeae, groups C and G streptococci, Arcanobacterium haemolyticum, Fusobacterium necrophorum, and Corynebacterium diphtheriae.
Patients with pharyngitis typically complain of sore throat, particularly when swallowing. Fever is lacking for most viral infections but often present with GAS. Patients may note “swollen glands” or anterior neck pain related to lymphadenopathy. When throat symptoms are due to a viral upper respiratory, symptoms such as nasal congestion, coryza, hoarseness, sinus discomfort, ear pain, or cough are common. A severe, usually exudative pharyngitis occurs in about half of the patients with either adenovirus infection or Epstein–Barr virus mononucleosis. The pharyngitis seen in herpangina, due to group A coxsackievirus, is characterized by a vesicular enanthem. Lesions (usually only two to six) begin as papules on the soft palate between the uvula and tonsils. These vesiculate and then ulcerate. Primary herpes simplex virus may cause a severe vesicular or ulcerative pharyngitis; when there is an overlying exudate, it may mimic streptococcal pharyngitis.
GAS is the most important bacterial cause of pharyngitis because of its suppurative (e.g., PTA) and nonsuppurative complications (e.g., rheumatic fever, acute post streptococcal glomerulonephritis).17 Patients with GAS may have a severe exudative pharyngitis accompanied by fever, leukocytosis, and cervical lymphadenopathy, or they may have a mild pharyngitis that mimics that of the common cold. Manifestations independently associated with group A streptococcal pharyngitis include tonsillar exudates, cervical lymphadenitis, lack of cough, and history of fever. However the signs and symptoms of GAS and nonstreptococcal pharyngitis overlap so broadly that diagnosis on this basis of clinical grounds alone lacks acceptable accuracy.
Diagnosis of streptococcal pharyngitis is made by culture or by rapid antigen detection test.17 The latter is 95% specific but not as sensitive as culture. Therefore, a negative test requires culture confirmation in children and adolescents, whereas a positive test is sufficient for the diagnosis. In adults, practice guidelines suggest that it is not necessary in usual circumstances to require culture backup because of the low incidence of GAS pharyngitis in adults and because the risk of subsequent acute rheumatic fever is generally exceptionally low in adults with acute pharyngitis. The use of a clinical algorithm without microbiological confirmation has been suggested as an acceptable alternative basis for the diagnosis of infection in adults (based on the presence of fever, adenopathy, and exudates, and lack of cough).18 However, use of this diagnostic strategy would result in treatment of an unacceptably large number of adults with nonstreptococcal pharyngitis; that is an undesirable result in this age group, which has a low prevalence of GAS pharyngitis and a very low risk of rheumatic fever or rheumatic carditis.
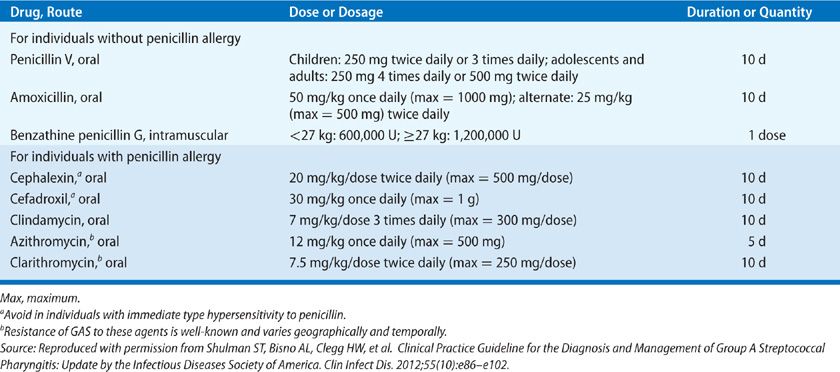
Penicillin or amoxicillin is the recommended drug of choice for GAS. Treatment in penicillin-allergic individuals may include a first-generation cephalosporin (for those not anaphylactically sensitive) for 10 days, clindamycin or clarithromycin for 10 days, or azithromycin for 5 days (Table 126-2). A PTA (quinsy) may follow untreated streptococcal pharyngitis—see Deep Neck Infections.
Other bacteria may also cause pharyngitis. Group C and G streptococci may cause an exudative pharyngitis and may be endemic or related to foodborne outbreaks. A. haemolyticum may cause an exudative pharyngitis along with a maculopapular rash, and typically occurs in children and young adults. Diphtheria, caused by C. diphtheriae, is rare in the United States. Sore throat is a common symptom (in 90%), and findings include mild pharyngeal injection and an overlying adherent gray membrane (especially over the tonsillar pillars) that bleeds if removal is attempted. N. gonorrhoeae may cause a mild pharyngitis, although most cases are asymptomatic. Neisseria meningitidis has rarely been noted as a cause of pharyngitis, but it is often isolated from throat cultures because the meningococcal carrier state is common. Carriers are not treated except in epidemic situations or if they have had close contact with a case of invasive meningococcal disease. C. pneumoniae and M. pneumoniae may cause a mild pharyngitis.
The anaerobe F. necrophorum is the causative agent of most cases of Lemmiere syndrome, septic thrombophlebitis of the internal jugular vein, which often results in metastatic pulmonary infections.19 Lemmiere syndrome should be suspected in patients with pharyngitis (usually severe), unilateral neck pain with swelling, septic pulmonary emboli, and persistent fever despite antimicrobial therapy. Patients typically present acutely with high fever (>39ºC) and rigors, often accompanied by respiratory distress. Since F. necrophorum is often β-lactamase producing, empiric therapy should include a β-lactamase resistant β-lactam antibiotic, such as ampicillin–sulbactam (3 g every 6 hours), piperacillin–tazobactam (4.5 g every 6 hours), ticarcillin–clavulanate (3.1 g every 6 hours), or monotherapy with a carbapenem. Surgical ligation or excision of the internal jugular vein may be necessary. The role of anticoagulation for jugular vein suppurative thrombophlebitis is controversial and generally not recommended.
ORAL CAVITY INFECTIONS
The oral cavity extends from the lips to the circumvallate papillae of the tongue. Various streptococci (e.g., Streptococcus mutans, Streptococcus mitis, Streptococcus salivarius) and anaerobes (e.g., Peptostreptococcus, Veillonella, Lactobacillus, Bacteroides, Prevotella) heavily colonize this area, and are the main pathogens in dental and oral cavity infections. S. mutans is a major pathogen in dental cavities. Gingivitis and periodontitis are associated with anaerobic gram-negative rods such as Prevotella intermedia and Porphyromonas gingivalis. Mouth anaerobes are the major cause of Vincent angina (acute necrotizing ulcerative gingivitis, or trench mouth). Patients have gingival pain, halitosis, cervical adenopathy, and ulcerations of the interdental papillae. Treatment is with oral clindamycin or penicillin plus metronidazole.20
DEEP NECK INFECTIONS
Deep neck infections include PTA (quinsy), retropharyngeal abscess, parapharyngeal space abscess, and infections of the sublingual or submandibular spaces.21,22 Pharyngeal space infection most often arises via contiguous spread of infection from a peritonsillar or retropharyngeal abscess. PTA is located between the tonsil and pharyngeal muscles. Most PTAs present as a severe sore throat (usually unilateral), fever, subdued voice; drooling and trismus are often present. Examination of the oral pharynx includes an extremely swollen and fluctuant tonsil with deviation of the uvula to the opposite side. If drooling is present care must be taken not to be aggressive during the examination of the oral cavity in case if epiglottis is present. Computed tomography (CT) with IV contrast distinguishes PTA from cellulitis and also demonstrates the spread of infection to contiguous deep neck spaces. PTAs are often polymicrobial. The predominant bacterial species are Streptococcus pyogenes, Staphylococcus aureus, and respiratory anaerobes. Management consists of drainage (needle aspiration or incision and drainage) and antimicrobial therapy (e.g., ampicillin–sulbactam or clindamycin).23
Ludwig angina is a rapidly spreading cellulitis of the sublingual and submandibular spaces. It usually begins from the floor of the mouth from an infected mandibular molar tooth. The sublingual area becomes edematous, pushing the tongue to the roof of the mouth. The infection is bilateral and can cause acute airway obstruction. Patients present with fever, difficulty swallowing, drooling, and prominent submandibular and sublingual swelling. They may lean forward to maximize the airway diameter and may have a muffled voice. CT is the imaging modality of choice for the diagnosis of Ludwig angina and other deep neck space infections. They should be admitted for airway monitoring, as intubation or tracheostomy may be necessary. Intravenous antibiotics active against streptococci and anaerobes should be given (e.g., ampicillin/sulbactam, clindamycin, penicillin G plus metronidazole). Surgical incision of the infected soft tissue compartment may be necessary. Mediastinitis is a rare complication resulting from spread into the parapharyngeal space and from there to the retropharyngeal space and the superior mediastinum.
LARYNGITIS
Laryngitis, or inflammation of the larynx, is characterized by hoarseness. Acute laryngitis is usually caused by the same viruses that cause the common cold, usually resolves within 3 weeks, and treatment is symptomatic.24 Hoarseness may accompany infections with human metapneumovirus and primarily associated with bronchiolitis in young children. Herpes simplex virus may cause acute laryngitis; ulcerations or vesicles are typically seen. Streptococcal pharyngitis may be associated with laryngitis and should be treated with penicillin. Patients with chronic hoarseness often have gastroesophageal reflux disease, but must be examined for laryngeal malignancies. In rare instances, fungi or mycobacteria may cause chronic laryngitis. In chronic progressive disseminated histoplasmosis, ulcers may occur on the larynx, as well as on the tongue, buccal mucosa, and gingiva (see Chapter 134). Blastomycosis may also produce laryngeal ulcers. Tuberculosis (TB) may cause laryngeal lesions that mimic a laryngeal neoplasm. Patients typically present with hoarseness but often lack systemic symptoms to suggest TB (see Chapter 131).25 They may have negative sputum smears for acid-fast bacilli and a clear chest radiograph. In a retrospective study of 22 patients with laryngeal TB, had clear lungs and only 7 had active pulmonary TB.26 The patients with concurrent pulmonary TB characteristically had multiple ulcerative lesions on their vocal cords, whereas those with clear lungs had nonspecific, polypoid, single laryngeal lesions.
CROUP
Croup, or acute laryngotracheitis, is characterized by inflammation of the larynx and trachea, associated with subglottic edema and occurs most often in children ages 3 months to 3 years old, with peak incidence in the second year of life.27 It is more common in boys. Most cases occur in fall, winter, and spring; the most common cause, parainfluenza virus (usually type 1), has caused biennial epidemics in the fall in the United States. Croup is characterized by fever, inspiratory stridor, and a “seal’s bark” cough. In severe cases, there is both inspiratory and expiratory stridor. There is typically a fluctuating course, and there can be alternating clinical improvement and worsening within an hour. Croup usually follows the onset of upper respiratory tract infection symptoms by 1 to 2 days. Other viruses that can also cause croup include RSV, adenovirus, human coronaviruses; influenza and M. pneumoniae are uncommon causes.
The diagnosis of croup is based primarily on clinical grounds. A diagnosis of the viral etiology may be made by one of the rapid viral antigen detection techniques (e.g., PCR) on nasopharyngeal swabs. The most important differential diagnosis in the acute clinical setting is epiglottitis (see below). Children with epiglottitis usually lack the characteristic seal’s bark cough of croup, appear more toxic, and their illness worsens more rapidly.
Appropriate management of croup depends upon an assessment of severity of illness. A commonly used scoring system for evaluating the severity of croup is the Westley croup score, the elements (and score) are as follows28:
• Level of consciousness: Normal, including sleep = 0; disoriented = 5
• Cyanosis: None = 0; with agitation = 4; at rest = 5
• Stridor: None = 0; with agitation = 1; at rest = 2
• Air entry: Normal = 0; decreased = 1; markedly decreased = 2
• Retractions: None = 0; mild = 1; moderate = 2; severe = 3
Children with mild symptoms, defined by a Westley croup score of ≤2, can be treated as outpatients and be treated symptomatically with humidity, fever reduction, and oral fluids. Close follow-up of response is recommended. Patients with moderate to severe croup (score ≥3) should be evaluated in a facility equipped to handle airway obstruction.
Treatment of croup consists of nebulized epinephrine, corticosteroids, and humidified air, although the value of humidified air has been questioned.29,30 Nebulized epinephrine is associated with clinically and statistically significant transient reduction of symptoms of croup 30 minutes posttreatment. Children should be monitored for rebound edema for several hours after initiation of therapy. Corticosteroids are also beneficial.31–33 Dexamethasone and budesonide are effective in relieving the symptoms of croup as early as 6 hours after the treatment. Fewer return visits and/or (re)admissions are required and the length of time spent in hospital is decreased. Oral or intramuscular dexamethasone has shown benefit for moderate to severe croup, and a single dose of oral dexamethasone is beneficial for mild croup.
EPIGLOTTITIS
Acute epiglottitis (supraglottitis) is a medical emergency, as it can rapidly lead to airway obstruction. It begins as a cellulitis between the base of the tongue and the epiglottis, pushing the epiglottis posteriorly. It then involves the epiglottis itself, with rapid swelling and airway compromise. Epiglottitis has become a rare disease in children since the advent of vaccination against Haemophilus influenzae type b (Hib) in 1985, which decreased the incidence of all types of invasive Hib disease by over 99%.34 In the prevaccine era, the incidence of epiglottitis was highest in children ages 2 to 4. Disease in children is due to rare cases of Hib vaccine failure or to other organisms, including nontypable H. influenzae. In one study, the incidence of acute epiglottitis in children was 0.02 cases/100,000 population/y.35 The incidence in adults was a mean of 1.9 cases/100,000 population/y. Two uniquely recognized vulnerable populations for epiglottitis are infants and the elderly. Blood cultures are usually negative in adults and cultures of the epiglottis difficult or dangerous to obtain, so the etiology is often unknown. Pathogens isolated from throat cultures in adults with supraglottitis include H. influenzae, H. parainfluenzae, Streptococcus pneumoniae, GAS, and S. aureus. Viral epiglottitis is very rare and poorly substantiated. In children, the onset of symptoms occurs rapidly, usually within 6 to 12 hours, and patients appear toxic. Patients are febrile, irritable, complain of sore throat and dysphagia, prefer to sit leaning forward, and may be drooling. Inspiratory stridor may occur, but the barking cough seen in croup is absent. Adolescents and adults usually have a less fulminant presentation, often with 2 to 3 days of symptoms.36 Severe sore throat, odynophagia, and fever are the main presenting symptoms, each occurring in 90% of adults in a recent study; muffled voice was present in 70%. In adults, diagnosis is made by direct flexible fiberoptic nasolaryngoscopy, a procedure that takes just minutes to perform in the emergency room by an otolaryngologist. A swollen, erythematous epiglottis is seen. Examination of a child in whom epiglottitis is a consideration should occur in a setting where the airway can be secured immediately if necessary.37,38 Children suspected of having epiglottitis should be transported, sitting up, to the operating room for direct endoscopic visualization of the epiglottis. An uncuffed endotracheal (or nasotracheal) tube should be immediately inserted (or, if necessary, a tracheostomy performed) if a “cherry red” edematous epiglottis is seen. Lateral neck radiographs, used in the past to demonstrate the “thumb sign” of an edematous epiglottis, are rarely used now as they may be falsely negative and may cause a critical delay in securing the airway.
All patients with epiglottitis should be monitored in an intensive care unit. Children with epiglottitis should be intubated for airway protection, whereas adults whose endoscopic examination reveals no impending airway compromise may be managed with close observation. The empiric regimen generally should provide coverage against the following pathogens: H. influenzae; Penicillin-resistant S. pneumoniae; β-hemolytic streptococci; S. aureus, including community-acquired methicillin-resistant S. aureus (MRSA) strain (e.g., combination therapy with a third-generation cephalosporin—ceftriaxone or cefotaxime – and an antistaphylococcal agent active against MRSA—clindamycin or vancomycin). If the patient with epiglottitis due to H. influenzae has household contacts that include an unvaccinated child younger than 4 years, the patient and all members of the household should receive rifampin prophylaxis to eradicate carriage of the organism.
BACTERIAL TRACHEITIS
This rare disorder, sometimes called membranous croup, presents acutely like epiglottitis but primarily involves the subglottic region like croup.39,40 Bacterial tracheitis almost always occurs in the setting of prior airway mucosal damage, as occurs with antecedent viral infection. It may represent bacterial superinfection of a viral tracheitis. The majority of cases occur in the fall and winter, coinciding with the typical seasonal epidemics of parainfluenza, RSV, and seasonal influenza. It usually affects children between 3 weeks and 13 years of age, and is uncommon in adults. Patients present with the acute onset of high fever, stridor, and dyspnea after a viral prodrome. Drooling is uncommon. They usually have leukocytosis. They do not respond to racemic epinephrine or corticosteroids. Lateral neck or anteroposterior radiographs typically show narrowing of the subglottic trachea that may be indistinguishable from that in viral croup. On endoscopy, patients have a normal epiglottis but the subglottic trachea is covered with a thick exudate. Inspissated secretions may produce a pseudomembrane. Cultures of tracheal secretions yield S. aureus in approximately half of the cases; other organisms include GAS, S. pneumoniae, and H. influenzae. Gram-negative bacilli have been rarely described. Treatment consists of maintenance of the airway, fluid resuscitation (if needed), and administration of appropriate antimicrobial agents. Many patients require immediate intubation; some require tracheostomy. Up to 60% will have concurrent pneumonia. Management consists of broad-spectrum intravenous antibiotics active against S. aureus and H. influenzae (e.g., ceftriaxone plus vancomycin), along with airway humidification and aggressive pulmonary toilet.
SINUSITIS (RHINOSINUSITIS)
Sinusitis is defined as an inflammation of the mucosal lining of the paranasal sinuses and can be caused by various factors including allergy, environmental irritants, and infection by viruses, bacteria, or fungi.41–44 It is more appropriately referred to as rhinosinusitis because there is almost always coexisting inflammation in the nasal mucosa. Rhinosinusitis can be classified on the basis of duration of symptoms into acute, subacute, and chronic. Acute rhinosinusitis lasts up to 4 weeks and is usually caused by a viral or bacterial infection. Chronic sinusitis lasts more than 12 weeks and may result from a wide range of allergic and nonallergic causes. Rhinosinusitis is an extremely common condition. In a national health survey conducted during 2008, nearly one in seven (13.4%) of all noninstitutionalized adults were diagnosed with rhinosinusitis within the previous 12 months.41 Incidence rates among adults are higher for women than men (by 1.9-fold), and adults between 45 and 74 years are most commonly affected. Recent estimates suggest that the direct annual costs of sinusitis are approximately $5.8 billion in the United States.41 Rhinosinusitis ranks among the top five reasons for antibiotic prescriptions for adults. Ninety percent to 98% of patients presenting with symptoms of sinusitis have viral causes and will not benefit from antibiotics. The overuse of antibiotics among this population has contributed largely to the emergence of antimicrobial resistance.
The paranasal sinuses develop as outpouches of the nasal cavity. The maxillary and ethmoid sinuses are present at birth, the frontal sinus develops after age 2, and the sphenoid sinus develops after age 7. The sinuses are lined with respiratory epithelium that includes ciliated cells and mucus-producing goblet cells. The cilia normally move the mucus blanket toward the sinus ostia (and then to the nasopharynx) at a speed of up to 1 cm/min. Inflammation causes a marked decrease in the beat frequency of the cilia, as well as narrowing or obstruction of the sinus ostia due to mucosal edema. The resulting disruption of mucociliary transport results in sinusitis. The frontal, anterior ethmoid, and maxillary sinuses open into the middle meatus, whereas the posterior ethmoid and sphenoid sinuses open into the superior meatus. The osteomeatal complex, an area between the middle and inferior nasal turbinates representing the confluence of drainage from the paranasal sinuses, is a particularly important anatomic site because of its potential for mucosal thickening and impaired drainage from viral infection leading to sinus infection. A viral etiology associated with a URI or the common cold is the most frequent cause of acute rhinosinusitis. Secondary bacterial infection of the paranasal sinuses following an antecedent viral URI is relatively uncommon, estimated to be 0.5% to 2% of adult.41 Viral infections increase the amount of mucus produced and may damage ciliated cells. Another predisposing factor for sinusitis is allergic rhinitis, which may cause ostial obstruction by mucosal edema or polyps. Dental infections, especially of the upper teeth that abut the maxillary sinus (second bicuspid, first and second molars), may cause some cases of maxillary sinusitis. Anatomic obstruction of the sinus ostia due to a deviated septum, tumor, granulomatous disease (e.g., granulomatous polyangiitis, formerly known as Wegener granulomatosis), or nasotracheal or nasogastric tubes may also lead to sinusitis. Barotrauma from deep-sea diving or airplane travel, chemical irritants, and mucus abnormalities (e.g., cystic fibrosis) are other risk factors for sinusitis.
 ACUTE BACTERIAL RHINOSINUSITIS
ACUTE BACTERIAL RHINOSINUSITIS
Symptoms of acute bacterial rhinosinusitis (ABRS) include purulent nasal or postnasal drainage, nasal congestion, and sinus pain or pressure. Nasal discharge and cough (which may be worse at night) are both common, whereas the presence of fever headache, or facial pain is more variable. The location of this pain depends on the sinus affected. Patients usually complain of pain in their cheek or upper teeth in maxillary sinusitis, the sides of the bridge of the nose in ethmoid sinusitis, supraorbital or frontal pain in frontal sinusitis, and retroorbital, frontal, occipital, or vertex pain in sphenoid sinusitis. Fever occurs in about half of the adults with ABRS. The gold standard for the diagnosis of ABRS is the recovery of bacteria from the cavity of a paranasal sinus.45 However, sinus aspiration is an invasive, time-consuming, and potentially painful procedure that does not have utility in the daily practice of primary care physicians. Endoscopically guided cultures of the middle meatus may be used as a surrogate for sinus aspirates in patients with ABRS. Performance of such cultures is beyond the scope of most primary care physicians, and its validity in children has not been established. Thus, the diagnosis of ABRS in most randomized controlled trials (RCTs) of antimicrobial is based on suggestive clinical manifestations.
Appropriate therapy is based on the presence of compatible symptoms and signs of acute rhinosinusitis with radiographic confirmation of sinus involvement. Unfortunately, these diagnostic criteria do not adequately distinguish bacterial from viral infection. Imaging studies such as plain radiographs or CT are frequently used by clinicians for the diagnosis of ABRS. Unfortunately, these studies are nonspecific and also do not distinguish bacterial from viral rhinosinusitis46 With no simple test to quickly determine whether an infection is viral or bacterial, many physicians prescribe antibiotics to play it safe. Such practices can lead to increased antibiotic resistance, exposure to drug side effects, and higher costs without resolution of their symptoms. Recent guidelines suggest antimicrobial therapy is appropriate in the following scenarios41:
• Symptoms of sinusitis lasting for more than 10 days without improving.
• Severe symptoms of sinusitis associated with fever of 102º F (38.9ºC) or higher, nasal discharge, and facial pain for 3 to 4 days.
• Symptoms of viral sinusitis that continue to gradually worsen more than 5 or 6 days and are accompanied by new fever, headache, or increased nasal discharge, typically following a viral upper respiratory infection of 5 or 6 days.
The bacteriology of sinusitis has been well defined only for acute, community-acquired maxillary sinusitis.45,47 Sinus puncture studies of adults with this infection have revealed that over 50% of cases are due to S. pneumoniae or nontypable H. influenzae (Table 126-3. Other pathogens include other streptococci, anaerobes, Moraxella catarrhalis, and rarely S. aureus. Studies of sinuses other than the maxillary sinus are hindered by the difficulty of obtaining culture material that is not contaminated by nasal flora.



