Atrioventricular (AV) conduction impairment is well described after surgical aortic valve replacement, but little is known in patients undergoing transcatheter aortic valve implantation (TAVI). We assessed AV conduction and need for a permanent pacemaker in patients undergoing TAVI with the Medtronic CoreValve Revalving System (MCRS) or the Edwards Sapien Valve (ESV). Sixty-seven patients without pre-existing permanent pacemaker were included in the study. Forty-one patients (61%) and 26 patients (39%) underwent successful TAVI with the MCRS and ESV, respectively. Complete AV block occurred in 15 patients (22%), second-degree AV block in 4 (6%), and new left bundle branch block in 15 (22%), respectively. A permanent pacemaker was implanted in 23 patients (34%). Overall PR interval and QRS width increased significantly after the procedure (p <0.001 for the 2 comparisons). Implantation of the MCRS compared to the ESV resulted in a trend toward a higher rate of new left bundle branch block and complete AV block (29% vs 12%, p = 0.09 for the 2 comparisons). During follow-up, complete AV block resolved in 64% of patients. In multivariable regression analysis pre-existing right bundle branch block was the only independent predictor of complete AV block after TAVI (relative risk 7.3, 95% confidence interval 2.4 to 22.2). In conclusion, TAVI is associated with impairment of AV conduction in a considerable portion of patients, patients with pre-existing right bundle branch block are at increased risk of complete AV block, and complete AV block resolves over time in most patients.
Severe symptomatic aortic valve stenosis constitutes an important health problem in elderly patients owing to its incidence of 2% to 5% in the general population and the associated impact on morbidity and mortality. Surgical aortic valve replacement improves symptoms and survival but is associated with an increased risk of adverse events in elderly and high-risk patients. Transcatheter aortic valve implantation (TAVI) has emerged as an alternative treatment option in this patient population. In Europe, 2 devices are approved for clinical use: the Edwards Sapien valve (ESV; Edwards Lifesciences, Irvine, California) and the Medtronic CoreValve Revalving System (MCRS; Medtronic, Minneapolis, Minnesota). The aim of the present study was to investigate the incidence and predictors of atrioventricular (AV) conduction impairment after TAVI using the MCRS and ESV prostheses.
Methods
From August 2007 to December 2008, 79 consecutive patients underwent TAVI at our institution. The MCRS and ESV prostheses were used, and all patients were prospectively followed in our registry. To be considered for TAVI the following inclusion criteria had to be fulfilled: (1) severe symptomatic aortic valve stenosis with an echocardiographic mean gradient >40 mm Hg or a calculated aortic valve area <1 cm 2 and (2) age ≥80 years and/or a logistic European System for Cardiac Operative Risk Evaluation score >15%, or age >60 years and ≥1 of the following criteria: previous cardiac surgery, pulmonary insufficiency (forced expiratory volume during 1 second <1 L), severe pulmonary hypertension (>60 mm Hg), porcelain aorta, history of mediastinal radiotherapy, or severe frailty (body mass index <18 kg/m 2 ).
The technical and anatomical feasibility of TAVI was assessed by right and left heart catheterization, computed tomography and transthoracic or transesophageal echocardiography. For clinical risk assessment the linear and logistic European System for Cardiac Operative Risk Evaluation score and Society of Thoracic Surgeons score were used. An interdisciplinary team of cardiac surgeons and interventional cardiologists reviewed all cases and formed a consensus on treatment selection (surgical aortic valve replacement versus TAVI). For this study, patients with previous permanent pacemaker (PPM) implantation before TAVI (n = 10) and those without procedural success (n = 2) were excluded from analysis. The study population consisted of 67 patients. The prospective registry was approved by the local ethics committee and all subjects gave written, informed consent.
According to anatomic characteristics the transfemoral or transapical approach was chosen. Transfemoral TAVI was performed using the MCRS or the ESV, whereas only the ESV was used for transapical access. After vascular access, the stenotic valve was crossed using a straight wire advanced through an Amplatz left catheter (AL1) catheter. A stiff wire was then placed into the left ventricular cavity and a large introducer sheath (18Fr for the MCRS or 22/24Fr for the ESV) carefully advanced. The optimal projection for valve implantation was chosen by identifying an angiographic plane with perpendicular orientation of the base of all 3 aortic valve sinuses. Balloon dilatation of the native aortic valve was performed under rapid right ventricular pacing (180 to 200/min) using a temporary pacemaker. After successful dilatation of the valve the MCRS or ESV was introduced and deployed under fluoroscopy. The result was checked by aortography and hemodynamic measurements using simultaneous recording of the left ventricular and aortic pressure curves.
Transapical TAVI was performed by a small anterolateral thoracotomy and exposure of the left ventricular apex. A purse-string suture was placed, followed by left ventricular wall puncture and sheath placement. After predilatation and valve deployment with the help of rapid right ventricular pacing, the access site was closed with pledgeted sutures. The temporary pacemaker was left in place for ≥48 hours in every patient.
Single 12-lead electrocardiograms obtained before and the first day after the intervention (18 to 24 hours) were systematically analyzed. For PPM implantation after TAVI, electrocardiographic findings leading to PPM implantation were also analyzed. During the follow-up period, treating physicians were asked to provide an electrocardiogram obtained ≥30 days after the intervention. To assess AV conduction in patients with a PPM after TAVI, an electrocardiogram was obtained with the PPM programmed to single-chamber modus (VVI) at a rate of 30/min.
All electrocardiograms were evaluated by 1 experienced electrophysiologist with assessment of heart rhythm, PR interval, QRS width, and AV conduction. Presence of a left or right bundle branch block was defined using standard criteria. Second-degree AV block included type I and II second-degree AV blocks, second-degree AV block with 2:1 AV conduction, and advanced second-degree AV block. Complete AV block was defined as absence of AV conduction.
Implantation of a PPM was performed if 1 of the following criteria was met: (1) transient or persistent complete or second-degree AV block after TAVI, (2) left bundle branch block and increasing PR interval after TAVI, or (3) left bundle branch block with increasing QRS width after TAVI.
Categorical variables are expressed as numbers and percentages, continuous variables as median and interquartile range. Categorical variables were compared with chi-square test or Fisher’s exact test, continuous variables with Mann-Whitney test or Wilcoxon test, as appropriate. For comparisons of PR interval and QRS width before TAVI, after TAVI, and during follow-up, only paired data with measurements on all 3 occasions were included (n = 43 for PR interval and n = 46 for QRS width). Univariable and multivariable Poisson regression analyses were used to obtain relative risk estimates of the development of complete AV block after TAVI. A p value <0.05 was considered statistically significant. Analyses were performed using SPSS 15.0 (SPSS, Inc., Chicago, Illinois) and STATA 10.1 (STATA Corp., College Station, Texas).
Results
Baseline clinical patient characteristics are presented in Table 1 . Electrocardiogram was obtained in all patients before and after TAVI. During follow-up, electrocardiogram was obtained in 55 patients at a median follow-up of 79 days (30 to 192). Eight patients (5 patients with PPM) died before a follow-up electrocardiogram was obtained (cause of death progressive heart failure in 6 and stroke in 2). Of the remaining patients, follow-up electrocardiogram was available in 93% and in all surviving patients with a PPM. Median time to follow-up electrocardiogram in patients with a PPM was 74 days (61 to 246).
| Variable | Overall | MCRS | ESV | p Value |
|---|---|---|---|---|
| (n = 67) | (n = 41) | (n = 26) | ||
| Clinical characteristics | ||||
| Age (years) ⁎ | 83 (80–85) | 84 (80–87) | 83 (81–85) | 0.18 ‡ |
| Women | 36 (54%) | 21 (51%) | 15 (58%) | 0.61 § |
| Access femoral | 50 (75%) | 41 (100%) | 9 (35%) | <0.001 § |
| Valve size 23 mm | 14 (21%) | 5 (12%) | 9 (35%) | — |
| Valve size 26 mm | 32 (48%) | 15 (37%) | 17 (65%) | — |
| Valve size 29 mm | 21 (31%) | 21 (51%) | — | — |
| Annulus diameter (mm) ⁎ | 23 (22–25) | 23 (22–25) | 23 (22–23) | 0.21 ‡ |
| Balloon size (mm) ⁎ | 23 (20–25) | 23 (22–25) | 20 (20–23) | <0.001 ‡ |
| Annulus/balloon ratio ⁎ | 1.0 (0.96–1.10) | 1.0 (0.96–1.05) | 1.05 (1.0–1.14) | 0.008 ‡ |
| Left ventricular ejection function (%) ⁎ | 51 (35–60) | 55 (41–60) | 50 (30–60) | 0.40 ‡ |
| Mean gradient (mm Hg) ⁎ | 50 (36–57) | 50 (36–60) | 40 (37–54) | 0.33 ‡ |
| Aortic valve area (cm 2 ) ⁎ | 0.60 (0.47–0.76) | 0.61 (0.44–0.78) | 0.60 (0.50–0.75) | 0.81 ‡ |
| Hypertension | 48 (72%) | 33 (81%) | 15 (58%) | 0.044 § |
| Diabetes mellitus | 15 (22%) | 7 (17%) | 8 (31%) | 0.19 § |
| Coronary artery disease † | 37 (55%) | 23 (56%) | 14 (54%) | 0.86 § |
| Log EuroSCORE (%) ⁎ | 23 (13–34) | 21 (12–31) | 23 (16–38) | 0.51 ‡ |
| Society of Thoracic Surgeons score (%) ⁎ | 6 (4–9) | 6 (4–8) | 6 (4–10) | 0.70 ‡ |
| Rhythm | ||||
| Sinus rhythm | 57 (85%) | 34 (83%) | 23 (89%) | 0.73 ∥ |
| Atrial fibrillation | 8 (12%) | 5 (12%) | 3 (12%) | 1.00 ∥ |
| Atrial flutter | 2 (3%) | 2 (5%) | 0 | 0.52 ∥ |
| Atrioventricular conduction | ||||
| PR interval (ms) ⁎ | 200 (170–220) | 195 (168–220) | 200 (180–220) | 0.72 ‡ |
| QRS width (ms) ⁎ | 110 (90–140) | 110 (90–140) | 105 (90–133) | 0.93 ‡ |
| Right bundle branch block | 13 (19%) | 8 (20%) | 5 (19%) | 0.98 § |
| Left bundle branch block | 11 (16%) | 6 (15%) | 5 (19%) | 0.74 ∥ |
| Medication | ||||
| β Blocker | 33 (49%) | 16 (39%) | 17 (65%) | 0.035 § |
| Calcium channel blocker | 3 (5%) | 2 (5%) | 1 (4%) | 1.00 ∥ |
| Digoxin | 7 (10%) | 6 (15%) | 1 (4%) | 0.23 ∥ |
| Amiodarone | 6 (9%) | 5 (12%) | 1 (4%) | 0.39 ∥ |
⁎ Median (interquartile range).
† Any patient with coronary artery narrowing ≥50% or history of coronary revascularization.
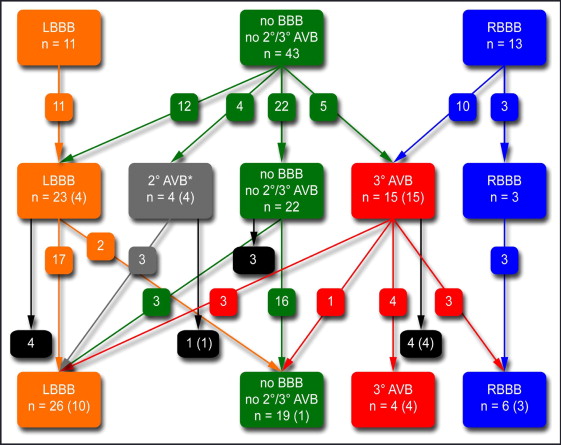
Figure 1 provides an overview of AV conduction before and after TAVI and during follow-up. After TAVI, AV conduction remained unchanged (no new bundle branch block, second-degree or complete AV block) except for PR interval prolongation in 36 patients (54%), whereas new left bundle branch block was observed in 15 patients (22%), second-degree AV block in 4 (6%), and complete AV block in another 15 patients (22%). During follow-up, new left bundle branch block developed in 3 patients, and left bundle branch block resolved in 2 patients. Four patients with complete AV block died before follow-up electrocardiogram was performed. In the remaining 11 patients, complete AV block had resolved in 7 patients (64%). Complete AV block had resolved to right bundle branch block in 3 patients, to left bundle branch block in 3 patients, and to normal QRS width with first-degree AV block (PR interval 420 ms) in 1 patient. Complete AV block persisted in 4 of 55 patients (7%) during long-term follow-up.
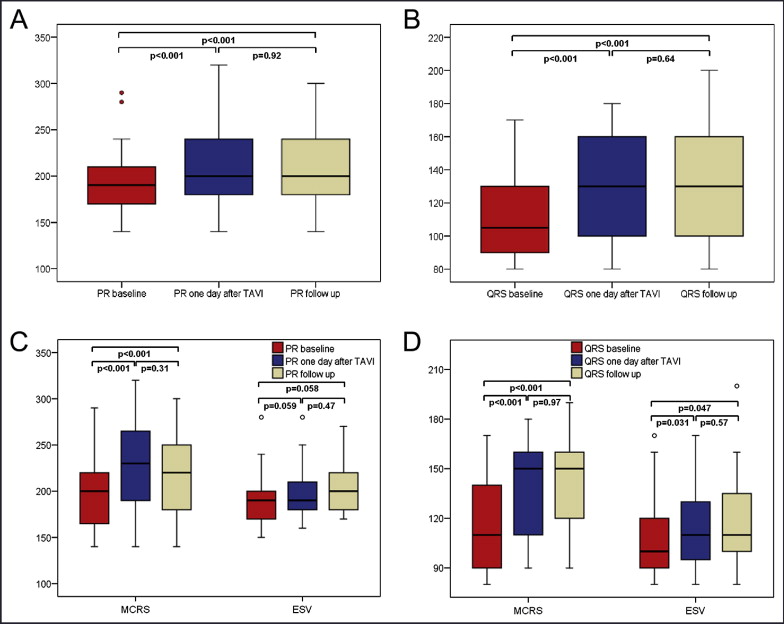
Overall PR interval significantly increased after TAVI compared to baseline measurements (190 ms, interquartile range 170 to 215, vs 200 ms, 180 to 245, p <0.001) but remained unchanged during long-term follow-up (200 ms, 180 to 240; Figure 2 ). Similarly, QRS width significantly increased from baseline to the first day after TAVI (105 ms, interquartile range 90 to 130, vs 130 ms, 100 to 160, p <0.001) without additional changes during long-term follow-up (130 ms, 100 to 160; Figure 2 ).
After TAVI, a PPM was implanted in 23 patients (34%) with a median delay of 3 days (1 to 7) without related complications ( Figure 1 ). Of the PPMs, 11 (48%) had single chamber and 12 (52%) had dual chamber. Characteristics of patients undergoing PPM implantation are presented in Table 2 . Indications for PPM implantation were (1) complete AV block in 15 patients (22%), with 2 patients developing complete AV block >1 day after TAVI and PPM implantation 7 and 10 days after TAVI, respectively, and these 2 patients initially had left or right bundle branch block after TAVI; (2) second-degree AV block in 4 patients (6%), and 3 of these patients also had left bundle branch block and 1 developed left bundle branch block >1 day after TAVI; and (3) left bundle branch block with increasing PR interval or QRS width in 4 patients (6%).
| Age (years)/Sex | Anulus Size (mm) | Balloon Size (mm) | Valve Type | Baseline | After TAVI | Time Delay to PPM (days) | FU | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rhythm | PR Interval (ms) | QRS Width (ms) | BBB | PR Interval (ms) | QRS Width (ms) | BBB | AV Block | PR Interval (ms) | QRS Width (ms) | BBB | AV Block | |||||
| 77/M | 26 | 30 | MCRS | SR | 170 | 140 | RBBB | — | — | — | 3° | 1 | — | — | — | 3° |
| 77/M | 22 | 20 | MCRS | SR | 220 | 160 | RBBB | — | — | — | 3° | 1 | — | — | — | 3° |
| 78/M | 23 | 20 | ESV ⁎ | AFib | — | 130 | RBBB | — | — | — | 3° | 3 | 160 | 180 | RBBB | — |
| 79/F | — | 22 | MCRS | AFlu | — | 110 | — | — | — | — | 3° | 3 | no FU | no FU | no FU | no FU |
| 80/M | 22 | 23 | MCRS | SR | 220 | 110 | — | 280 | 150 | LBBB | — | 7 | 290 | 170 | LBBB | — |
| 80/M | 25 | 25 | MCRS | SR | 240 | 90 | — | 240 | 100 | — | 2° | 3 | 250 | 150 | LBBB | — |
| 81/F | 23 | 20 | ESV ⁎ | SR | 240 | 180 | RBBB | — | — | — | 3° | 2 | no FU | no FU | no FU | no FU |
| 81/F | 25 | 22 | MCRS | AFib | — | 180 | RBBB | — | — | — | 3° | 1 | — | 160 | RBBB | — |
| 83/F | 22 | 23 | ESV ⁎ | AFib | — | 140 | RBBB | — | — | — | 3° | 3 | — | — | — | 3° |
| 83/F | 22 | 22 | MCRS | SR | 180 | 90 | — | — | — | — | 3° | 10 | 250 | 170 | LBBB | — |
| 83/M | 22 | 25 | MCRS | SR | 370 | 160 | RBBB | — | — | — | 3° | 3 | no FU | no FU | no FU | no FU |
| 83/M | 24 | 25 | MCRS | SR | 290 | 110 | — | 440 | 160 | LBBB | 2° | 9 | 370 | 160 | LBBB | — |
| 83/M | 25 | 25 | MCRS | AFlu | — | 140 | RBBB | — | — | — | 3° | 3 | — | — | — | 3° |
| 84/M | 25 | 25 | MCRS | AFib | — | 150 | RBBB | — | — | — | 3° | 2 | no FU | no FU | no FU | no FU |
| 84/M | 26 | 30 | MCRS | SR | 180 | 150 | LBBB | 280 | 150 | LBBB | — | 3 | 200 | 160 | LBBB | — |
| 84/M | 27 | 25 | MCRS | SR | 210 | 90 | — | 320 | 170 | LBBB | — | 4 | 220 | 190 | LBBB | — |
| 85/F | 22 | 23 | MCRS | SR | 160 | 90 | — | — | — | — | 3° | 1 | 180 | 140 | LBBB | — |
| 85/F | 23 | 30 | MCRS | SR | 160 | 100 | — | 180 | 160 | LBBB | 2° | 8 | 180 | 160 | LBBB | — |
| 86/M | 21 | 22 | MCRS | SR | 430 | 80 | — | — | — | — | 3° | 0 | 420 | 80 | — | — |
| 87/M | 26 | 25 | MCRS | SR | 200 | 160 | RBBB | — | — | — | 3° | 7 | 200 | 160 | RBBB | — |
| 89/F | 27 | 22 | MCRS | SR | 180 | 110 | — | 180 | 150 | LBBB | — | 2 | 180 | 150 | LBBB | — |
| 90/F | 22 | 23 | MCRS | SR | 250 | 90 | — | 340 | 90 | — | 2° | 11 | no FU | no FU | no FU | no FU |
| 91/F | 23 | 22 | MCRS | SR | 160 | 80 | — | — | — | — | 3° | 1 | 150 | 130 | LBBB | — |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


