The objective of this study was to evaluate the impact of diffuse coronary atherosclerosis on the functional evaluation of moderate coronary lesions in the proximal-mid segment of a coronary artery and its clinical implications. This was a prospective study including 100 consecutive patients with a moderate lesion (45 ± 9% diameter stenosis) in the proximal-mid coronary segment who were evaluated with fractional flow reserve (FFR) measurement. No patient had any other angiographic stenosis distal to the evaluated coronary stenosis. FFR measurements were obtained just distal (∼2 to 3 cm) to the lesion (FFR proximal measurement [FFR-PM]) and as distally as possible in the artery (FFR distal measurement [FFR-DM]) after administration of the same dose of intracoronary adenosine. Thirty-nine patients underwent dipyridamole or exercise myocardial single-photon emission computed tomography within 3 months of the FFR study. Mean FFR-PM was significantly higher compared to FFR-DM (0.84 ± 0.08 vs 0.78 ± 0.09, median gradient 0.06, 25th to 75th interquartile range 0.02 to 0.10, p <0.0001). FFR-DM was <0.75 in 33% of patients with FFR-PM ≥0.75, leading to the decision of revascularization in these patients. Performing FFR measurement in the left main/left anterior descending artery predicted a higher gradient between FFR-DM and FFR-PM (odds ratio 4.58, 95% confidence interval 1.4 to 15.03, p = 0.007). FFR-DM exhibited a better correlation with results of myocardial single-photon emission computed tomography compared to FFR-PM (kappa 0.33 vs 0.22, p <0.0001). In conclusion, significant differences between FFR-DM and FFR-PM were observed in patients with moderate coronary stenosis in the proximal-mid segment of a coronary artery, with FFR-DM exhibiting a better correlation with results of noninvasive functional tests. These differences influenced the treatment decision in about 1/3 of patients and highlight the potential clinical relevance of coronary pressure wire positioning for functional evaluation of lesions in the proximal-mid segment of the coronary arteries.
Coronary fractional flow reserve (FFR) is an established index for determining functional severity of coronary stenosis. Also, De Bruyne et al showed that in patients with coronary artery disease coronary arteries without angiographically visible stenosis exhibit a graded continuous pressure decrease along the length of the artery as evaluated by coronary pressure wire. However, the potential impact of this phenomenon on the functional evaluation of lesions in the proximal-mid segment of a coronary artery has not yet been extensively evaluated. In fact, the optimal distance up to which the pressure wire should be advanced into the coronary artery remains controversial. Although many studies do not specify the distance between the pressure wire and the coronary lesion, some investigators have recommended positioning the wire just distal or about 3 cm distal to the lesion, whereas others have proposed advancing the wire as distally as possible or up to the distal segment of the coronary artery. Indeed, the American Heart Association/American College of Cardiology scientific statement on the physiologic assessment of coronary artery disease made no formal recommendation concerning how distal the coronary pressure wire should be from the lesion being evaluated. Thus the objectives of this study were (1) to compare the FFR measurement obtained just distal (∼2 to 3 cm) to the lesion to those obtained as distally as possible in the same coronary artery and (2) to determine the predictive factors and clinical implications of the occurrence of significant differences, if any, between the 2 FFR measurements in patients with a single moderate lesion in the proximal-mid segment of a coronary artery.
Methods
This was a prospective study including 100 consecutive patients with a moderate coronary lesion (defined as approximately 50% diameter stenosis by visual estimation) in the proximal-mid segment of a coronary artery that was evaluated by coronary pressure wire with FFR measurement at maximal hyperemia. None of the patients included in the study had any other angiographically visible stenosis distal to the evaluated coronary stenosis. Coronary angiography was performed from the radial or femoral approach using standard catheters and conventional views. Quantitative coronary angiographic measurements of lesions were performed offline by an investigator blinded to clinical and FFR data using the Medis quantitative coronary angiographic system (Medis Medical Imaging Systems, Inc., Nuenen, Netherlands).
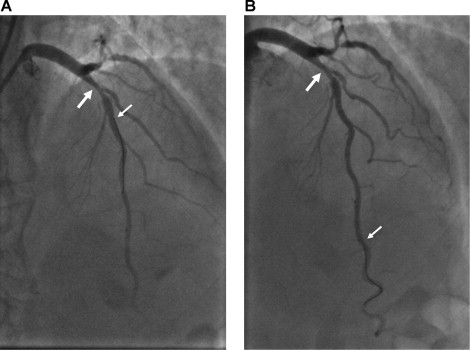
FFR measurements were performed with a 0.014-inch pressure-sensing guidewire (Radi Medical Systems, Uppsala, Sweden; or Volcano, San Diego, California). The coronary pressure guidewire was introduced through the catheter, calibrated, advanced into the coronary artery, and positioned ∼2 to 3 cm distal to the coronary stenosis ( Figure 1 ). Maximal hyperemia was induced by intracoronary administration of adenosine 300 μg for the left coronary artery and 150 μg for the right coronary artery. This first FFR measurement was called FFR proximal measurement (FFR-PM) and calculated as the ratio of mean hyperemic coronary pressure measured by the pressure wire to mean aortic pressure measured by the guiding catheter. After this first FFR measurement, the wire was advanced as distally as possible in the coronary artery ( Figure 1 ) and a new FFR measurement (FFR distal measurement [FFR-DM]) was obtained using the same dose of intracoronary adenosine. Special care was taken to avoid inserting the pressure wire into small branches or too deeply into the most distal part of the coronary artery. Angiographic acquisition showing the position of the pressure wire was obtained before FFR measurements in all patients. For lesions in the left main coronary artery, the pressure-sensing guidewire was calibrated at the level of the ascending aorta, and immediately after intracoronary injection of adenosine the tip of the catheter was retrieved from the left main coronary artery to obtain appropriate FFR measurements. FFR measurement was calculated as the ratio of mean hyperemic distal coronary pressure measured by the pressure wire to mean aortic pressure measured by the guiding catheter.
Thirty-nine patients included in the study had undergone myocardial scintigraphy (single-photon emission computed tomography [SPECT]) as a noninvasive functional test with potential for ischemia location within 3 months of coronary angiography and FFR measurements. Thirty-three patients underwent technetium-99 tetrofosmin SPECT with intravenous dipyridamole (0.14 mg/kg per minute for 4 minutes), and 6 patients underwent symptom-limited exercise technetium-99m tetrofosmin SPECT. All examinations were evaluated by observers unaware of coronary angiographic and FFR findings. Seventeen myocardial segments were evaluated according to the myocardial segmentation and nomenclature for tomographic imaging of the heart of the American Heart Association statement. Each segment was attributed to a coronary artery taking into account the coronary dominance and length of the left anterior descending coronary artery (LAD). A semiquantitative interpretation was performed and each segment was scored using a 5-point scoring system (0 = normal; 1 = equivocal; 2 = moderate; 3 = severe decrease of isotope; 4 = absence of detectable tracer uptake in a segment). A single-photon emission computed tomographic study was judged abnormal if the difference between scores during stress and at rest including all segments related to 1 artery was >2.
Revascularization deferral was based on results of FFR measurements. Coronary revascularization was performed if the FFR measurement was <0.75, deferred if the FFR measurement was >0.80, and an individualized decision based on additional clinical data was taken if the FFR measurement was 0.75 to 0.80. For this study the physicians responsible for the patient indicated in all cases whether performing the 2 FFR measurements changed their clinical decision regarding lesion revascularization. All patients were followed by telephone contact or clinical visits. The study was performed in accordance with the ethics committee and all patients signed the informed consent for the procedures.
Quantitative variables were expressed as mean ± SD or median (25th to 75th interquartile range) depending on variable distribution. Student’s t test or Wilcoxon test was used for comparisons between numerical variables, and chi-square test or Fischer’s exact test was used to compare qualitative variables. Multivariate logistic regression analysis including variables exhibiting a p value <0.2 in univariate analysis was used to determine factors associated with a higher (above the median) gradient between FFR-DM and FFR-PM. Level of agreement between FFR measurements and results of noninvasive functional tests were determined by the kappa test. Comparison of accuracy of FFR-DM and FFR-PM for detecting myocardial ischemia as evaluated by myocardial SPECT was performed with a generalized linear model. A p value <0.05 was considered statistically significant.
Results
Clinical characteristics of the study population are listed in Table 1 , and quantitative coronary angiographic and FFR measurement characteristics of intermediate lesions are listed in Table 2 . Most (64%) FFR-evaluated coronary lesions (mean diameter stenosis 45 ± 9%) were in the proximal-mid segment of the LAD. Mean FFR-PM was significantly higher compared to FFR-DM (0.84 ± 0.08 vs 0.78 ± 0.09, median gradient 0.06, 25th to 75th interquartile range 0.02 to 0.10, p <0.0001). FFR-DM was <0.75 in 42 patients, whereas only 13 patients had an FFR-PM <0.75. FFR-DM was therefore <0.75 and FFR-PM ≥0.75 in 29% of patients. Individual values for FFR-PM and FFR-DM are shown in Figure 2 , and patients grouped according to FFR values (<0.75, ≥0.75 to ≤0.80, and >0.80) obtained for FFR-PM and FFR-DM are shown in Figure 3 . Clinical, angiographic, and FFR measurement characteristics grouped according to coronary pressure gradient (proximal-distal, above or below median gradient, i.e., 0.06) are presented in Table 3 . Patients who exhibited a greater coronary pressure gradient between FFR-PM and FFR-DM were more frequently men, less frequently had a history of myocardial infarction, and FFR measurements were more frequently performed in the LAD than in the other 2 coronary arteries. In multivariate analysis location of the stenosis in the left main coronary artery/LAD was the only factor determining a greater difference (>0.06) between FFR-PM and FFR-DM (odds ratio 4.58, 95% confidence interval 1.4 to 15.03, p = 0.007).
| Age (years) | 62 ± 11 |
| Men | 73 (73%) |
| Current smoker | 22 (22%) |
| Hypertension ⁎ | 57 (57%) |
| Dyslipidemia † | 70 (70%) |
| Diabetes mellitus | 22 (22%) |
| Previous myocardial infarction | 25 (25%) |
| Previous coronary angioplasty | 30 (30%) |
| Ejection fraction (%) | 59 ± 9 |
| Clinical indication for angiography | |
| Stable angina pectoris | 28 (28%) |
| Unstable angina pectoris | 33 (33%) |
| Non–ST-segment elevation myocardial infarction | 15 (15%) |
| ST-segment elevation myocardial infarction | 7 (7%) |
| Atypical chest pain | 7 (7%) |
| Noninvasive functional test | 68 (68%) |
| Myocardial scintigraphy | 39 (39%) |
| Treadmill test | 44 (44%) |
| Angiographic characteristics | |
| 1 vessel with stenosis >70% | 25 (25%) |
| 2 vessels with stenosis >70% | 17 (17%) |
| 3 vessels with stenosis >70% | 3 (3%) |
⁎ Blood pressure ≥140/90 mm Hg or treatment with antihypertensive medication.
† Low-density lipoprotein cholesterol levels >3.50 mmol/L or treatment with lipid-lowering medication.
| p Value | ||
|---|---|---|
| Target coronary arteries | ||
| Left main | 17 (17%) | |
| Left anterior descending | 64 (64%) | |
| Left circumflex | 3 (3%) | |
| Right | 16 (16%) | |
| Quantitative coronary angiographic measurements | ||
| Lesion reference diameter (mm) | 2.88 ± 0.73 | |
| Lesion minimal lumen diameter (mm) | 1.56 ± 0.46 | |
| Lesion diameter stenosis (%) | 45.3 ± 8.8 | |
| Fractional flow reserve measurements | ||
| Proximal measurement ⁎ | 0.84 ± 0.08 | <0.0001 |
| Distal measurement † | 0.78 ± 0.09 | |
| Fractional flow reserve gradient proximal minus distal measurement, median (25th to 75th) | 0.06 (0.02–0.10) | |
| Proximal measurement <0.75 | 13 (13%) | <0.0001 |
| Distal measurement <0.75 | 42 (42%) | |
| Proximal measurement ≥0.75 and distal measurement <0.75 | 29 (29%) |
⁎ Coronary pressure wire positioned just distal to stenosis.
† Coronary pressure wire positioned as distally as possible.
| Variable | Gradient FFR-PM/FFR-DM ≤0.06 | Gradient FFR PM/FFR-DM >0.06 | p Value |
|---|---|---|---|
| (n = 61) | (n = 39) | ||
| Age (years) | 62 ± 11 | 60 ± 10 | 0.44 |
| Men | 40 (66%) | 33 (85%) | 0.04 |
| Current smoker | 12 (20%) | 10 (26%) | 0.62 |
| Hypertension | 35 (58%) | 22 (56%) | 1.00 |
| Dyslipidemia | 42 (70%) | 28 (72%) | 1.00 |
| Diabetes mellitus | 15 (25%) | 7 (18%) | 0.46 |
| Previous myocardial infarction | 20 (33%) | 5 (13%) | 0.03 |
| Previous coronary angioplasty | 21 (35%) | 9 (23%) | 0.27 |
| Ejection fraction (%) | 59 ± 10 | 61 ± 7 | 0.42 |
| Clinical indication for angiography | |||
| Stable angina pectoris | 16 (27%) | 12 (31%) | 0.66 |
| Unstable angina pectoris | 20 (33%) | 13 (33%) | 1.00 |
| Non–ST-segment elevation myocardial infarction | 11 (19%) | 4 (10%) | 0.39 |
| ST-segment elevation myocardial infarction | 3 (5%) | 4 (10%) | 0.43 |
| Atypical chest pain | 5 (8%) | 2 (5%) | 0.70 |
| Noninvasive functional test | |||
| Myocardial scintigraphy | 24 (39%) | 15 (39%) | 1.00 |
| Treadmill test | 25 (42%) | 19 (49%) | 0.68 |
| Target coronary arteries | |||
| Left main/left anterior descending | 45 (74%) | 36 (92%) | 0.03 |
| Left circumflex | 2 (3%) | 1 (3%) | |
| Right | 14 (23%) | 2 (5%) | |
| Fractional flow reserve proximal measurement | 0.84 ± 0.08 | 0.85 ± 0.06 | 0.27 |
| Quantitative coronary angiography | |||
| Lesion reference diameter (mm) | 2.95 ± 0.8 | 2.77 ± 0.5 | 0.18 |
| Lesion minimal lumen diameter (mm) | 1.61 ± 0.5 | 1.48 ± 0.3 | 0.14 |
| Lesion diameter stenosis (%) | 45.2 ± 8.3 | 45.4 ± 9.6 | 0.94 |
| Angiographic characteristics | |||
| No vessel with stenosis >70% | 36 (59%) | 19 (49%) | 0.18 |
| 1 vessel with stenosis >70% | 17 (28%) | 8 (20%) | |
| 2 vessels with stenosis >70% | 7 (11%) | 10 (26%) | |
| 3 vessels with stenosis >70% | 1 (2%) | 2 (5%) |
Myocardial SPECT demonstrated the presence of ischemia in the territory of the FFR-evaluated artery in 19 of 39 patients (49%). Comparisons between results of FFR-PM and FFR-DM and results of myocardial SPECT are presented in Table 4 . FFR-PM had a sensitivity of 26% and specificity of 95% for detection of myocardial ischemia (kappa 0.22, p = 0.065). FFF-DM showed a sensitivity of 53% and specificity of 80% for detection of myocardial ischemia (kappa 0.33, p = 0.033, p <0.0001 vs FFR-PM).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


