Current recommendations discourage elective radiofrequency ablation in patients <5 years old and/or weighing <15 kg, primarily because of the greater complication rate. To describe the current use, complications, and immediate outcomes of cryoablation in this patient population, a multicenter retrospective review of all patients <5 years old and/or weighing <15 kg who were treated with cryoablation for arrhythmia was performed. Eleven centers contributed data for 68 procedures on 61 patients. Of those, 34% were elective and 24% (n = 16) were both cryoablation and radiofrequency ablation. The median age and weight at ablation was 3.5 years (range 8 days to 9.9 years) and 15.2 kg (range 2.3 to 23), respectively. Congenital heart disease was present in 23% of the patients. The immediate success rate of cryoablation alone was 74%. No major complications occurred with cryoablation only; however, 2 of the 16 patients who underwent cryoablation and radiofrequency ablation had major complications. Of the 50 patients receiving cryoablation, 8 (16%) had variable degrees of transient atrioventricular block. The recurrence rate was 20% after cryoablation and 30% after cryoablation plus radiofrequency ablation. In conclusion, cryoablation appears to have a high safety profile in these patients. Compared to older and larger patients, the efficacy of cryoablation in this small, young population was lower and the recurrence rates were higher. Cryoablation’s effect on the coronary arteries has not been fully elucidated and requires additional research.
In 2002, the North American Society for Pacing and Electrophysiology issued an Expert Consensus on radiofrequency (RF) catheter ablation in children. The committee reported that the Pediatric RF Registry data “consistently demonstrated that age <4 years or weight <15 kg are independent risk factors for complications.” The guidelines placed age limits on the indications for RF ablation, recommending the use of ablation in patients <5 years old as class IIB only after antiarrhythmic medications “including sotalol and amiodarone” have failed. Since the development of these guidelines, cryoablation technology has become an important tool for the pediatric electrophysiologist for ablation in high-risk areas such as the atrioventricular node slow pathway or near coronary arteries. It was hypothesized that cryoablation is a safe alternative to RF ablation in patients <5 years old or weighing <15 kg as an alternative to medication in the treatment of arrhythmias in this population.
Methods
The present study was an international multicenter retrospective review of cryoablation in infants and children <5 years old and/or weighing <15 kg at the ablation procedure, including those in whom cryoablation was unsuccessful and RF was then used. Members of the Pediatric and Congenital Electrophysiology Society retrospectively collected data from the existing patient records at each of their respective institutions. The data were submitted to the primary investigators for analysis. All participating centers provided institutional review board approval. The data were collected on the preprocedural, procedural, and postprocedural variables. “Incessant” defined an arrhythmia present for >50% of the day. Permanent junctional reciprocating tachycardia (PJRT) was used to define slowly conducting accessory pathways (APs) producing long RP tachycardia. Cryomapping was defined as a cryoapplication lasting <30 seconds or set to a minimum temperature of −30° to −40°C. Cryoablation was defined as a minimum temperature reaching ≥−60°C applied for >30 seconds. For the purposes of the present study, “cryoablation failure” was defined as the act of changing from cryoenergy to RF (because this was a retrospective study across multiple centers, a more exact definition of cryoablation failure was not possible). The procedural outcomes and complications were queried as 2 separate groups: cryoablation only and those using both cryoablation and RF during the same procedure. No patients undergoing only RF ablation were included in the present study. Complications were characterized as “transient”—resolved before case completion, “prolonged”—persisted after case completion, “delayed”—diagnosed within 24 hours of case completion but not during the procedure, and “late”—diagnosed >24 hours after procedure completion. Major intraprocedural complications were considered, including death, emergent operation, mechanical cardiovascular support, initiation of inotropes, neurologic damage, emergent pacemaker implantation, myocardial infarction, pericardiocentesis, prolonged or permanent atrioventricular block (AVB) (second or third degree only), coronary artery stenosis, new valve regurgitation, and femoral vessel occlusion. The chi-square test was used to compare the proportions of RF success versus cryoablation success and the incidence of adverse effects with each modality.
Results
Eleven centers participated, contributing data on a total of 68 procedures performed on 61 patients. The diagnosis at initial presentation is listed in Table 1 . Congenital heart disease was present in 14 (23%) of the 61 patients. Of the 61 patients, 4 had undergone a previous heart operation (3 atriotomies and 1 ventriculotomy). A total of 10 patients (16%) had signs of congestive heart failure before the ablation procedure—8 of these were in incessant tachycardia (5 with PJRT and 3 with focal atrial tachycardia). One patient was receiving extracorporeal membrane oxygenation for incessant supraventricular tachycardia. An echocardiogram was obtained 1 week before ablation for 50 (74%) of the 68 procedures. Moderate to severely decreased ventricular function was present in 8 patients (16%): 7 with incessant tachyarrhythmia, 1 with congenital heart disease, and 3 without clinical signs of heart failure. The antiarrhythmic drug treatment regimens before ablation varied widely. Of the 61 patients, 9 (15%) had received no antiarrhythmic drug therapy. β Blocker and/or digoxin were used initially in 47 (78%) of 61 patients, and 27 patients proceeded to ablation after treatment with only these 2 medications. The percentage of patients treated with each drug was 78% with a β blocker, 50% with digoxin, 40% with 1C, 32% with amiodarone, 23% with sotalol, 4% with class 1A, 4% with calcium channel blocker, and 2% with class 1B.
| Diagnosis | Presenting Diagnosis (n = 61 Patients) | Electrophysiologic Study Diagnosis (n = 68 Procedures) |
|---|---|---|
| Uncharacterized supraventricular tachycardia | 19 | |
| Concealed accessory pathway-mediated tachycardia | 10 | 21 |
| Permanent junctional reciprocating tachycardia | 7 | 10 |
| Atrioventricular nodal re-entry tachycardia | 6 | 17 |
| Manifest accessory pathway; no tachycardia | 5 | 5 |
| Junctional tachycardia | 5 | 4 |
| Ectopic atrial tachycardia | 4 | 7 |
| Long RP tachycardia | 1 | |
| Ventricular tachycardia | 1 | 1 |
| Wolff-Parkinson-White syndrome | 1 | 1 |
| Dilated cardiomyopathy with electrical dyssynchrony | 1 | |
| Nonfocal atrial tachycardia | 1 | |
| Nodoventricular | 2 |
The primary indications for ablation and patient age and weight data are listed in Table 2 . Seven procedures were performed in patients with no history of tachycardia: 5 for pre-excitation and 2 for dilated cardiomyopathy with ventricular dyssynchrony. In the 9 patients who had received no previous antiarrhythmic therapy, the indications for the procedure were elective in 4, pre-excitation with an apparent life-threatening event in 2, ventricular dysfunction in 2, and planned atrial septal defect closure in 1. The median interval between the initial diagnosis and the cryoablation procedure was 1.4 years (range 1 week to 6 years). Of the 5 patients undergoing ablation at <1 month of age, 4 had incessant supraventricular tachycardia (2 of whom were in heart failure, including 1 patient receiving extracorporeal membrane oxygenation). The fifth patient had a high-risk AP and atrial septal defect closure was planned. The remaining 6 patients who were <1 year old included 4 with incessant supraventricular tachycardia and/or heart failure. Six patients had >1 ablation procedure included in the study. Five of these patients had recurrences of their initially successful ablation and underwent a second ablation. Their diagnoses were PJRT, nodoventricular pathway, atrioventricular nodal re-entry tachycardia (AVNRT), AP-mediated tachycardia, and focal atrial tachycardia. One patient initially had a right inferior paraseptal AP ablated and returned for AVNRT cryoablation.
| Variable | Value |
|---|---|
| Primary indication for ablation ⁎ | |
| Medication failure or side effects | 31 (45%) |
| Elective | 23 (34%) |
| Incessant tachycardia | 22 (33%) |
| Ventricular dysfunction | 10 (17%) |
| Syncope and ventricular pre-excitation | 2 (4%) |
| Planned surgical atrial septal defect closure | 1 (2%) |
| Median age (range) at ablation (years) | 3.5 (1 week to 6 years) |
| Age <1 month at ablation | 5 (7%) |
| Age <1 year at ablation | 11 (16%) |
| Median weight (range) at ablation (kg) | 15.2 (2.3–23.6) |
| Weight <5 kg | 6 (9%) |
| Weight 5–10 kg | 4 (6%) |
| Weight 10–15 kg | 26 (38%) |
| Weight >15 kg | 32 (47%) |
⁎ Note, overlap present between categories of “elective,” “medication side effects,” and “ventricular pre-excitation” because these were reported together as indications by some centers; overlap was also present between “mediation failure” and “incessant tachycardia.”
The electrophysiologic study diagnoses are listed in Table 1 . Left atrial access was required in 12 patients (6 used an existing interatrial communication and 6 required a Brockenbrough transeptal puncture). Coronary angiograms were obtained during 8 procedures before cryoablation. Of the 68 procedures, 33 used a 4-mm tip cryoablation catheter, 24 used a 6-mm tip, 9 used both a 4- and 6-mm tip, and 1 used an 8-mm tip. Mapping lesions were used in 44 procedures (65%). The mean number of cryoablation applications per procedure was 5.9 ± 5.4 (range 1 to 34). The mean number of 4-minute applications was 3.6 ± 3.2 (range 0 to 15).
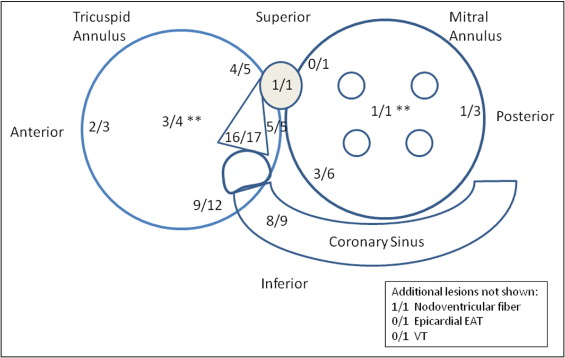
Of the 68 procedures, 50 (74%) were successful using cryoablation. The locations of the targeted substrates are shown in Figure 1 . Two cryoablation procedures were unsuccessful and not treated with RF: 1 patient had junctional tachycardia and 1 had a right superior paraseptal AP. The other 16 procedures (24%) used RF after cryoablation failure. The mean number of cryoablation lesions placed before switching to RF was 13.6 (range 2 to 31). Thirteen of these (81%) resulted in an acutely successful ablation, yielding a total procedural success rate of 93% (63 of 68) when both cryoablation and RF were considered. The 3 patients not successfully ablated were 1 patient with ventricular tachycardia and 2 with manifest APs. A comparison of cryoablation success versus RF success using the chi-square test showed no significant difference.