Although taking a “quick look” at the heart using a small ultrasound device is now feasible, a formal ultrasound imaging protocol to augment the bedside physical examination has not been developed. Therefore, we sought to evaluate the diagnostic accuracy and prognostic value of a cardiopulmonary limited ultrasound examination (CLUE) using 4 simplified diagnostic criteria that would screen for left ventricular dysfunction (LV), left atrial (LA) enlargement, inferior vena cava plethora (IVC+), and ultrasound lung comet-tail artifacts (ULC+) in patients referred for echocardiography. The CLUE was tested by interpretation of only the parasternal LV long-axis, subcostal IVC, and 2 lung apical views in each of 1,016 consecutive echocardiograms performed with apical lung imaging. For inpatients, univariate and multivariate logistic regression analyses were performed to assess the relations between mortality, CLUE findings, age, and gender. In this echocardiographic referral series, 78% (n = 792) were inpatient and 22% (n = 224) were outpatient. The CLUE criteria demonstrated a sensitivity, specificity, and accuracy for a LV ejection fraction of ≤40% of 69%, 91%, and 89% and for LA enlargement of 75%, 72%, and 73%, respectively. CLUE findings of LV dysfunction, LA enlargement, IVC+, and ULC+ were seen in 16%, 53%, 34%, and 28% of inpatients. The best multivariate logistic model contained 3 predictors of in-hospital mortality: ULC+, IVC+ and male gender, with adjusted odds ratios (95% confidence intervals) of 3.5 (1.4 to 8.8), 5.8 (2.1 to 16.4), and 2.3 (0.9 to 5.8), respectively. In conclusion, a CLUE consisting of 4 quick-look “signs” has reasonable diagnostic accuracy for bedside use and contains prognostic information.
A cardiopulmonary limited ultrasound examination (CLUE) could provide the foundation for an “ultrasound-assisted” physical examination and can be derived using data that already exist within the fields of echocardiography and chest ultrasonography. However, the distillation of these 2 disciplines into 1 simplified examination for general use should be guided by evidence and practical considerations. Systolic left ventricular (LV) dysfunction, left atrial (LA) enlargement, pulmonary edema, and elevated central venous pressures have bedside prognostic and diagnostic importance in patients with suspected cardiopulmonary disease and are reasonable evidence-based targets to include in a modern-day ultrasound cardiac physical examination, just as they have been targets of physical examination for centuries. Moreover, these findings can be screened by subjective interpretation of only 4 ultrasound views: the cardiac parasternal long-axis view of the left ventricle, 2 longitudinal anterior views of the lung apices, and a subcostal longitudinal view of the inferior vena cava (IVC). Therefore, we sought to test the diagnostic accuracy and prognostic importance of a simple CLUE on patients already referred for echocardiography.
Methods
Data were obtained retrospectively from consecutive comprehensive transthoracic echocardiograms performed using conventional, fully featured echocardiographs (Philips iE33, Philips Healthcare, Andover, Massachusetts) and low-frequency 3-MHz phased-array cardiac transducers, during a 3-month period in a 300-bed tertiary medical center. Repeated, follow-up, or limited examinations were not included. The echocardiographic evaluation included parasternal, apical, and subcostal imaging using 2-dimensional, color, and spectral Doppler and M-mode according to published guidelines and 2 views of the lung apices to evaluate for lung comet tail artifacts as a part of the institution’s routine standard echocardiographic imaging protocol. Each echocardiogram was acquired by 1 of 7 randomly available experienced registered cardiac sonographers, and interpreted by 1 of 12 board-certified cardiologists rotating as reader-of-the-day. The Scripps Institutional Review Board for Scripps Mercy Hospital (San Diego, California) approved the study.
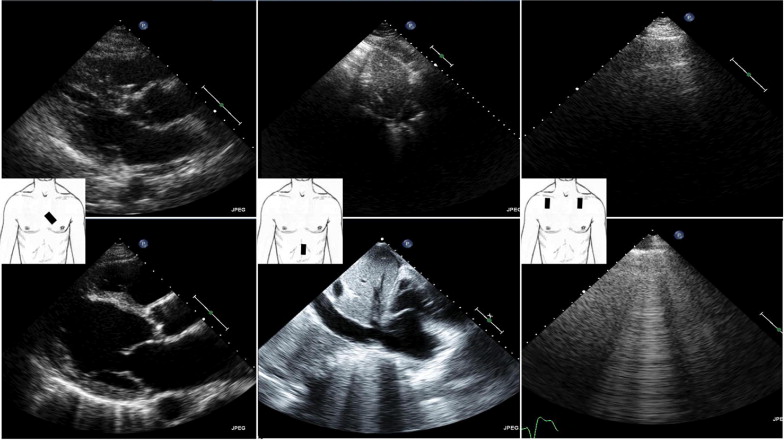
CLUE was defined a priori to consist of 4 video-looped views ( Figure 1 ) within the comprehensive echocardiographic study. The 4 specific CLUE views were interpreted by 1 cardiologist-echocardiographer who was unaware of the results of the comprehensive study and based his interpretation using the predetermined subjective “quick-look” criteria as follows. The first CLUE view was the standard echocardiographic parasternal LV long-axis view for the evaluation of LV systolic dysfunction and LA enlargement. LV dysfunction was defined as present by quick-look subjective estimation if the anterior leaflet of the mitral valve during diastole did not appear to encroach on the LV outflow tract and approach the septum to within 1 cm. LA enlargement was defined as present if the LA anteroposterior diameter appeared larger than the anteroposterior diameter of the overlying ascending aorta at the sinuses of Valsalva, throughout the cardiac cycle. The second CLUE view was the standard echocardiographic subcostal longitudinal view of the proximal intrahepatic inferior vena cava as it entered the right atrium. Elevated central venous pressures were considered present (IVC+) if the IVC subjectively appeared plethoric and dilated, as noted by parallel vessel walls and a luminal diameter reduction of <50% with respiratory motion of the diaphragm, without forced “sniffing”. The final 2 CLUE views were bilateral longitudinal views taken with the transducer probe in the midinfraclavicular region in the second intercostal space of each lung apex demonstrating the pleural line, typically framed by both rib shadows. An ultrasound lung comet tail artifact was considered present (ULC+) if, in this view, ≥3 vertical hyperechoic lines were seen to emanate from the pleural line in the near field and reach the far field, moving with respiration. The data were recorded as whether ULCs were demonstrated in either lung, noted as “any ULC+,” or both lungs, noted as “bilateral ULC+.”
The accuracy of the CLUE findings of LV dysfunction or LA enlargement were assessed using the results reported from the corresponding reference standard echocardiogram. As is common in standard “real-world” practice, multiple techniques provided estimates of the LV ejection fraction and LA size to the reader during the comprehensive study, each with a perceived accuracy dependent on the known limitations of the technique, patient body habitus, and the specific quality of the study data. For the ejection fraction, the techniques included Teicholz-based M-mode, the Simpson’s biplane method of disks (modified Simpson’s rule), and subjective estimates by the sonographer. For LA size, the standard anteroposterior LA diameter was obtained from M-mode and the LA volume index was routinely measured using the area-length method, with mild LA enlargement considered present when >4.0 cm and >28 ml/m 2 , respectively. The final interpretation of the LV ejection fraction and LA size was according to the discretion of the reader-of-the-day after the synthesis and review of all available data and subjective determinations and was included in the echocardiographic final report. Because CLUE acquisition and interpretation of the IVC+ and ULC+ findings used the same method as in the comprehensive echocardiogram, no separate reference standard echocardiographic assessment existed for validation of these parameters. The final standard echocardiographic reports were scrutinized for the presence of LV systolic dysfunction defined as a LV ejection fraction of ≤40% or any mention of greater than moderate systolic dysfunction. The presence of LA enlargement was considered present if any mention of its enlargement was found in the report or, in the absence of such, if the LA anteroposterior diameter using M-mode was >4.5 cm.
A comprehensive echocardiogram was considered “technically inadequate” if technically poor, limited, or difficult images were mentioned, and no interpretation of the LV ejection fraction or LA size was provided in the final report. Technically inadequate studies were excluded from the diagnostic analysis. CLUE images were thought to be technically inadequate if the data acquired were of such poor target resolution that they did not permit subjective evaluation by the predefined criteria or if the data were nonexistent owing to an inability to access the proper window because of bandages, wounds, or patient discomfort.
Inpatient echocardiographic mortality was defined as the ratio of the number of deaths of inpatients who had undergone echocardiography during their admission divided by the total number of inpatients undergoing echocardiography during the 3-month study period. Deaths that occurred within the emergency department were considered inpatient deaths. Outpatients were not included in the mortality analysis, because their outcomes were not known. The total inpatient mortality, a value calculated for comparison to the inpatient echocardiographic mortality, was estimated as the number of total deaths divided by the total number of unique patient admissions during the study period.
Patient age is expressed as the mean ± SD and categorical data as percentages. Statistical analysis was performed by a statistician (T.W.) using R software (R Foundation for Statistical Computing, Vienna, Austria). The inpatient and outpatient groups were compared using chi-square tests and t tests, depending on the data. The diagnostic sensitivity, specificity, accuracy, and positive and negative predictive values were derived for the CLUE diagnostic criteria for LV systolic dysfunction and LA enlargement by comparing the interpretation of technically adequate CLUE views with the results of LV ejection and LA enlargement from the reference standard echocardiogram.
For the mortality outcome analysis, only inpatient CLUE studies in which all 4 views were technically adequate were considered. The relation between inpatient mortality and CLUE variables of LV systolic dysfunction, LA enlargement, ULC+, and IVC+ and standard echocardiographic variables of LV ejection fraction of ≤40% and LA enlargement, and patient gender was examined using Pearson chi-square tests, and the relation with age examined using univariate logistic regression analysis. Odds ratios (ORs) with 95% confidence intervals (CIs) were computed for each variable of interest. Multivariate logistic regression analysis examined the joint effect of these predictors on mortality. The best-fit multivariate model using CLUE findings, patient age, and gender variables was selected using the Akaike Information Criterion. Significance was assessed at α = 0.05.
Results
Data consisted of 1,016 echocardiograms, of which 224 (22%) were outpatient and 792 (78%) were inpatient. The overall patient age was 65.6 ± 16.8 years (range 16.0 to 97.0), and 51% were male. Outpatients, compared to inpatients, were significantly younger (61.7 ± 17.0 years, range 18.0 to 94.0, vs 66.5 ± 16.6 years, range 16.0 to 97.0, p = 0.0002), and 48% were male compared to 52% of the inpatients (p = NS).
Regarding only the assessment of LV ejection fraction and LA enlargement, comprehensive echocardiography showed technical inadequacy in 2 (0.2%) and 28 (2.8%) final reports, respectively, and these were excluded from the diagnostic accuracy analysis. Because the CLUE findings were limited to an assessment from a single view, as expected, the rates at which each CLUE finding could not be delineated owing to technical limitations were greater: LV systolic dysfunction, 5.4%; LA enlargement, 4.3%; IVC+, 17%; and ULC+, 5.7%. Overall, the LV ejection fraction was 62.3 ± 13.8% (inpatients 61.6 ± 9.9% and outpatients 64.9 ± 14.7%, p = 0.0001), and the LA size was 3.9 ± 0.8 cm (inpatients 4.0 ± 0.9 cm and outpatients 3.8 ± 0.7 cm, p <0.0001). As expected, all CLUE findings were significantly more prevalent in the inpatients than in the outpatients ( Table 1 ).
| Variable | Outpatients | Inpatients | ORs for Inpatient Mortality (95% CI) |
|---|---|---|---|
| Age >65 years | 103/224 (46%) | 447/792 (56%) ⁎ | 0.68 (0.35–1.33) |
| Men | 108/224 (48%) | 415/792 (52%) | 2.5 ⁎ (1.2–5.2) |
| CLUE results | |||
| LV dysfunction | 16/219 (7%) | 117/742 (16%) ⁎ | 1.65 (0.69–3.95) |
| LA enlargement | 85/221 (38%) | 398/751 (53%) ⁎ | 0.77 (0.37–1.61) |
| IVC+ | 27/199 (14%) | 222/648 (34%) ⁎ | 6.36 ⁎ (2.66–15.21) |
| ULC+ (any) | 19/215 (9%) | 209/743 (28%) ⁎ | 4.6 ⁎ (2.21–9.56) |
| ULC+ (bilateral) | 9/215 (4%) | 115/743 (16)% ⁎ | 5.3 ⁎ (2.58–11.01) |
| Echocardiographic findings | |||
| LV ejection fraction ≤40% | 10/224 (5%) | 89/790 (11%) ⁎ | 2.47 ⁎ (1.08–5.62) |
| LA enlargement | 79/218 (36%) | 396/770 (51%) ⁎ | 1.0 (0.5–2.0) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


