The rising use of imaging cardiac stress tests has led to potentially unnecessary testing. Interventions designed to reduce inappropriate stress testing have focused on the ambulatory setting. We developed a computerized order entry tool intended to reduce the use of imaging cardiac stress tests and improve appropriate use in hospitalized patients. The tool was evaluated using preimplementation and postimplementation cohorts at a single urban academic teaching hospital. All hospitalized patients referred for testing were included. The co-primary outcomes were the use of imaging stress tests as a percentage of all stress tests and the percentage of inappropriate tests, compared between the 2 cohorts. There were 478 patients in the precohort and 463 in the postcohort. The indication was chest pain in 66% and preoperative in 18% and was not significantly different between groups. The use of nonimaging stress tests increased from 4% in the pregroup to 15% in the postgroup (p <0.001). Among very low–risk chest pain patients, the use of nonimaging stress tests increased from 7% to 25% (p <0.001). Inappropriate testing did not change significantly between groups (12% vs 11%). Inappropriate tests were most often preoperative evaluations (83%). In conclusion, our computerized ordering tool significantly increased the use of nonimaging cardiac stress tests and reduced the use of imaging tests yet was not able to reduce inappropriate use. Our study highlights the differences in cardiac stress testing between hospitalized and ambulatory patients.
The use of cardiac stress testing with imaging has increased dramatically in recent years, without concomitant improvements in outcomes. Appropriate use criteria were developed to minimize unnecessary testing. From 12% to 18% of stress tests with imaging are considered inappropriate, but studies have focused mostly or exclusively on testing in the ambulatory setting. We recently showed that a similar percentage of tests in hospitalized patients are inappropriate, although the testing indications are quite different between the settings, and the number of inappropriate tests in hospitalized patients may be artificially low. We designed a computerized order entry tool with the goal of reducing the use of stress tests with imaging in low-risk hospitalized patients and diverting appropriate patients toward treadmill electrocardiogram (ECG) testing without imaging instead.
Methods
Our study consisted of 2 cohorts, a preintervention cohort who were evaluated before the implementation of the computerized order entry tool, and a postintervention cohort, evaluated after the tool was in use 1 month, to allow for technical evaluation and to match the time of year in both cohorts. All hospitalized patients referred for cardiac stress tests (with or without imaging) from September 2010 to February 2011 were included in the preintervention cohort. The results of this group have been published previously. After designing and implementing the order entry tool, the postintervention cohort included all patients referred for stress tests from September 2011 to February 2012. All patient data were collected prospectively, as part of an ongoing quality improvement initiative, and individual informed consent was therefore not obtained. Permission to review the data for research purposes was granted by the Institutional Review Board at the Hospital University of Pennsylvania.
After evaluating the preintervention cohort, the order entry tool was designed specifically for hospitalized patients. It worked within the existing computerized order entry system in use at our institution (Sunrise; Allscripts, Chicago). Previously, there were separate orders for each type of test (nuclear imaging, echocardiography, electrocardiography only), and stress method (pharmacologic or treadmill). The order entry tool combined these into 1 order set. The order page also included links to relevant guidelines.
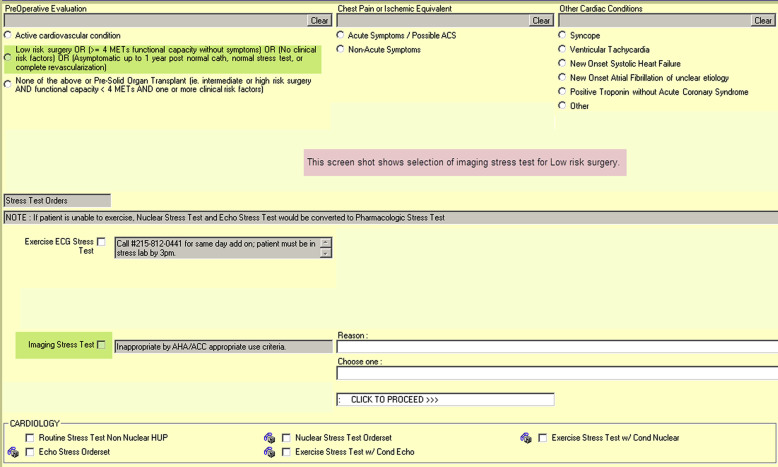
Providers were asked to select 1 of the 4 most common indications for testing in hospitalized patients: chest pain/ischemic equivalent, preoperative, asymptomatic, or other cardiac condition (which included several choices). Secondary prompts within each category included questions about functional capacity and coronary disease risk. Links were available to relevant risk calculators and SDs. For orders for stress tests with imaging that were inappropriate (e.g., low-risk preoperative evaluation), ordering providers had to click an acknowledgment and provide a reason if imaging was still requested ( Figure 1 ). For low-risk chest pain (Thrombolysis In Myocardial Infarction [TIMI] score ≤2), there was also a suggestion of treadmill ECG testing without imaging as the first choice. In all cases, the provider retained the option to choose any type of testing method he or she desired. The complete order entry algorithm is available in the Supplementary Figure 1 .
The order entry tool defaulted to use treadmill exercise as the stress method. Provider input allowed for patients with activity limitations to move directly to pharmacologic stress. For patients who were ordered treadmill stress, there were prompts to allow conversion to pharmacologic stress if the patient could not exercise to target during the study. Similarly, patients undergoing treadmill ECG testing could be converted to pharmacologic testing with imaging if they were unable to exercise to target during the study at the provider’s request.
Once the new ordering system was implemented all ordering providers received a brief in-service regarding the rationale and goals of the initiative. The order page also included contact information for cardiology consultation if the provider needed further assistance.
Our study had 2 primary goals. One was to reduce the inappropriate use of stress tests with imaging as a proportion of all stress tests. The second goal was to reduce the use of imaging tests as a proportion of all tests, that is, to increase the use of treadmill ECG testing without imaging. Secondary goals included increasing the use of treadmill ECG testing for low-risk chest pain patients and increasing the use of treadmill exercise rather than pharmacologic stress as the mode of stress for all patients. Other prespecified secondary analyses included comparisons based on test indication and test method. Patient characteristics were collected prospectively.
Appropriate use was determined as described previously using the relevant stress echocardiography and nuclear guidelines. All tests were reviewed by 2 board-certified cardiologists with specialty certification in nuclear stress testing and echocardiography. For cases where there was disagreement, a third cardiologist made the determination. There are no Appropriate Use Criteria for treadmill ECG testing, so we considered class 3 indications from the most recent guidelines to be inappropriate. Because of the goals of our study, all tests were classified as inappropriate or not inappropriate, with “unclear” included in the not inappropriate category.
Continuous variables were compared using a t test for normal distributions and a Wilcoxon rank-sum test for nonnormal distributions. Categorical variables were compared using a Fisher’s exact test or chi-square test as appropriate.
Results
A total of 480 patients were referred for cardiac stress testing during the preintervention period. Of these, appropriate use criteria could not be applied in 2 cases. The remaining 478 patients comprise the preintervention cohort. During the second study period, 467 patients were referred for stress tests, in whom appropriate use criteria could not be applied in 4 cases. The remaining 463 patients comprise the postintervention cohort. The baseline characteristics of the preintervention and postintervention cohorts are listed in Table 1 . The indications for testing were similar in both cohorts. Chest pain or ischemic equivalent was the indication for 67% of the preintervention tests and 65% of the postintervention tests, whereas preoperative evaluation accounted for 19% in the initial group and 17% of the postintervention group (p = 0.12).
| Variable | All Patients (n=941) | Pre-Intervention (n=478) | Post-Intervention (n=463) | p value ∗ |
|---|---|---|---|---|
| Age (years) | 61.2 (±13.8) | 61.0 (±13.9) | 61.3 (±13.8) | 0.69 |
| Female | 45% (n=422) | 45% (n=215) | 45% (n=207) | 0.95 |
| White | 49% (n=465) | 47% (n=227) | 51% (n=238) | 0.24 |
| Prior Coronary Disease † | 27% (n=251) | 30% (n=143) | 23% (n=108) | 0.02 |
| Hypertension | 73% (n=688) | 75% (n=359) | 71% (n=329) | 0.16 |
| Diabetes Mellitus | 31% (n=292) | 29% (n=140) | 33% (n=152) | 0.26 |
| Hyperlipidemia | 55% (n=517) | 55% (n=265) | 54% (n=252) | 0.79 |
| Smoker | 26% (n=245) | 27% (n=129) | 25% (n=116) | 0.50 |
∗ p Value is comparing preintervention versus postintervention.
† Defined as a history of coronary stenosis by angiogram or previous percutaneous or surgical coronary intervention.
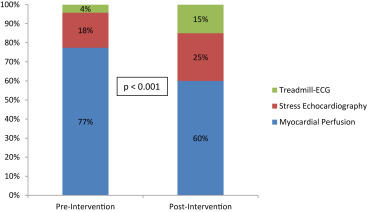
The intervention had a significant impact on the type of test that was ordered, with a nearly fourfold increase in nonimaging treadmill ECG testing ( Figure 2 ). The use of treadmill exercise as the stress method increased from 34% of all tests to 40% of all tests (p = 0.04). Among stress tests with imaging, the use of treadmill stress did not change significantly (30% vs 29%, p = 0.76), a reflection of the increased utilization of stress testing without imaging in the postintervention cohort.
The intervention did not have a significant impact on the frequency of inappropriate testing (12% vs 11%, p = 0.54). None of the treadmill ECG stress tests were inappropriate. Comparisons within the imaging stress tests based on testing method and most common indications are listed in Table 2 . Treadmill exercise was much less frequent among inappropriately tested patients (33% of appropriate tests vs 11% of inappropriate tests, p <0.001), suggesting that only a small percentage of inappropriate tests would have the option of being converted to a treadmill ECG test. The reasons tests were considered inappropriate are provided in the Supplementary Table 1 . There was no significant difference in inappropriate indications before and after the implementation of the order entry tool.
| Variable | Appropriate/Uncertain (n=745) | Inappropriate (n=106) | p value ∗ |
|---|---|---|---|
| Age (years) | 62.2 (±13.6) | 61.5 (±12.7) | 0.61 |
| Female | 46% (n=344) | 34% (n=36) | 0.02 |
| White | 44% (n=330) | 80% (n=74) | <0.001 |
| Prior Coronary Disease † | 31% (n=232) | 19% (n=20) | 0.009 |
| Hypertension | 77% (n=579) | 60% (n=64) | 0.10 |
| Diabetes Melllitus | 34% (n=254) | 21% (n=22) | 0.006 |
| Hyperlipidemia | 58% (n=431) | 44% (n=47) | 0.01 |
| Smoker | 26% (n=194) | 25% (n=27) | 0.99 |
| Chest Pain/ Ischemic Equivalent | 76% (n=564) | 4% (n=5) | <0.001 |
| Pre-operative | 11% (n=82) | 83% (n=88) | <0.001 |
| Nuclear Imaging | 76% (n=569) | 72% (n=76) | 0.33 |
| Post-Intervention | 46% (n=345) | 46% (n=49) | 0.99 |
| Exercise as Stress Modality | 33% (n=243) | 11% (n=12) | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


