In ST-segment elevation myocardial infarction (STEMI) impairment of microcirculatory function is a negative independent predictor of myocardial function recovery. In the Impact of Thrombectomy with EXPort Catheter in Infarct-Related Artery during Primary Percutaneous Coronary Intervention (PCI; EXPIRA) trial we found that manual thrombectomy resulted in a better myocardial reperfusion expressed by an improved procedural outcome and a decrease of infarct size compared to conventional PCI. The aim of the present study was to investigate whether the early efficacy of thrombus aspiration translates into very long-term clinical benefit. We randomized 175 patients with STEMI with occlusive thrombus at baseline undergoing primary PCI to thromboaspiration with a manual device (Export Medtronic, n = 88) or standard PCI (n = 87). No differences in baseline, clinical, and angiographic preprocedural findings were observed between the 2 groups except for incidence of hypertension and cholesterol levels. After 24 months major adverse cardiac events were 13.7% versus 4.5% (p = 0.038, log-rank test) and cardiac death was 6.8% versus 0% (p = 0.012, log-rank test). A strict correlation was observed between cardiac death incidence and tissue reperfusion parameters (postprocedural myocardial blush grade and ST-segment resolution). In conclusion, manual thrombus aspiration before stenting of the infarct-related artery in selected patients with STEMI improving myocardial reperfusion significantly decrease cardiac death and major adverse cardiac events at 2 years.
Primary percutaneous coronary intervention (PPCI) is gold-standard treatment in patients presenting with ST-segment elevation myocardial infarction (STEMI). However, myocardial tissue reperfusion is often decreased due to the occurrence of distal atherothrombotic debris embolization, limiting the efficacy of PPCI. Numerous evidences have suggested that manual aspiration thrombectomy during PPCI represents an useful adjunct to pharmacotherapy able to prevent distal embolization, decreasing microvascular damage and getting better myocardial perfusion. We previously observed in the Impact of Thrombectomy with EXPort Catheter in Infarct-Related Artery during Primary Percutaneous Coronary Intervention (EXPIRA) trial that manual thrombectomy during primary angioplasty to prevent thrombus embolization preserves microvascular integrity and decreases infarct size as assessed by cardiac magnetic resonance. Our data showed a lower rate of death in the thrombus aspiration group at 9-month follow-up. A lack of data exists on clinical follow-up >1 year. The aim of our study was to investigate whether the early efficacy of thrombus aspiration translates into clinical benefit after 2 years.
Methods
Details of the EXPIRA trial have been previously reported. EXPIRA investigated whether thrombus aspiration as adjunctive therapy in PPCI was better than standard PCI in patients with STEMI and angiographic evidence of a large thrombus burden. The trial was a single-center, randomized, open study with blinded assessment of end points.
One hundred seventy-five consecutive patients admitted with STEMI and candidates for PPCI were enrolled at the Policlinico Umberto I, “Sapienza” University of Rome, from March 2004 to September 2006. Patients were randomly assigned in a 1:1 manner to Export Medronic PCI (EM-PCI) or standard PCI ( Figure 1 ).
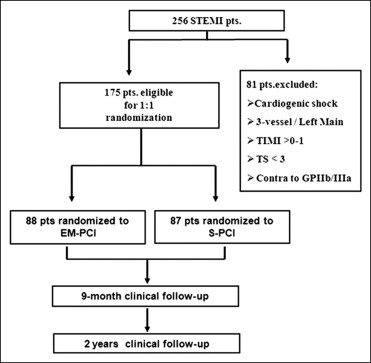
Inclusion criteria were diagnosis of first STEMI (evidence of ischemic chest pain for >30 minutes and new ST-segment elevation ≥2 mm in ≥2 contiguous electrocardiographic leads) within 9 hours from symptom onset, de novo coronary artery lesion, native vessel ≥2.5 mm in diameter, angiographically identifiable thrombus (presence of filling defect within the coronary lumen surrounded by contrast medium observed in multiple projections, without calcium within the filling defect, or persistence of contrast medium within the coronary lumen), thrombus score ≥3, Thrombolysis In Myocardial Infarction (TIMI) grade 0 to 1 flow, and age >18 years.
Exclusion criteria were previous PCI in an infarct-related artery, previous MI or coronary artery bypass grafting, cardiogenic shock, 3-vessel disease, left main coronary artery disease, severe valvular heart disease, rescue PCI, facilitated PCI, contraindication to glycoprotein IIb/IIIa inhibitors, and current participation in another study.
Clinical characteristics of patients (age, gender, hypercholesterolemia, diabetes, family history of coronary artery disease, hypertension, and smoking) were collected.
The institutional review board approved the study and all patients included in the trial provided written informed consent.
All patients were pretreated with aspirin 300 mg orally, heparin intravenously to maintain an activated clotting time >250 seconds. Abciximab (0.25-mg/kg bolus followed by an intravenous infusion at 0.125 μg/kg/min) was administered before revascularization and prolonged for 12 hours. PPCI was performed according to standard clinical practice using a femoral artery Judkins approach with a 7F sheath insertion in the right groin. After crossing the target occlusive lesion with the guidewire, ≥2 passages across the lesion from proximal to distal were performed by slowly advancing the aspiration thrombectomy catheter. When necessary for stent delivery, balloon dilation was done before stenting. Conventional PPCI was performed according to standard clinical practice. Subsequently, patients received heparin for 48 hours, aspirin 100 mg/day, and clopidogrel (300-mg loading dose followed by 75 mg/day for ≥12 months). Other adjunctive pharmacotherapy was administered according to operator discretion. Standard therapies after PCI included β blockers, lipid-lowering agents, and angiotensin-converting enzyme inhibitors or angiotensin II receptor antagonists, according to current guidelines.
The primary efficacy end points of the EXPIRA trial were occurrence of final myocardial blush grade ≥2 and rate of ST-segment resolution >70%.
In this study we evaluated the following major adverse cardiac events (MACEs): occurrence of cardiac death regarded as cardiac unless an unequivocal noncardiac cause of death was established, reinfarction defined as recurrent symptoms with new ST-segment elevation and increase of cardiac markers to ≥2 times the upper limit of normal, and target vessel revascularization defined as clinically driven percutaneous revascularization or bypass of the target lesion or any segment of the epicardial coronary artery containing the target lesion. Angiographically proved stent thrombosis was defined as complete or partial occlusion within the stented segment, with evidence of thrombus and decreased anterograde flow (TIMI grade <3 flow) with a concurrent acute clinical ischemic event.
Clinical follow-up with medical examination was performed at 9 months and at 2 years in all patients to assess the occurrence of the following MACEs: cardiac death, nonfatal reinfarction, and target vessel revascularization. Written questionnaires were also used to obtain information on medical therapy during medical clinical follow-up. Vital status was also obtained from a central population registry. Incidence of stent thrombosis was also evaluated. All MACEs were assessed and classified by an interventional cardiologist who was unaware of treatment allocation.
Statistical analysis was performed using SPSS 16.0 for Windows (SPSS, Inc., Chicago, Illinois). Mean ±SD was calculated for quantitative variables and percentage for qualitative variables. Differences between quantitative variables were tested by Student’s t test or Mann-Whitney test for variables that were not normally distributed. Differences between qualitative variables were tested by Pearson chi-square test.
Event-free survival curves for death and combined major cardiac events were constructed by the Kaplan-Meier method, and statistical differences between curves were assessed by log-rank test. A multivariate Cox proportional hazards regression model was used to identify independent predictors of cardiac death. All variables presenting a significant value (p <0.25) at univariate analysis were included in the final model. The “enter” method was used in the multivariate final model and hazard ratios (HRs) with 95% confidence intervals (CIs) were calculated.
Differences were considered statistically significant at a 2-sided p value <0.05.
Results
Baseline clinical and angiographic characteristics were well-balanced between the 2 groups with the exception of hypertension, smoke and cholesterol levels. Procedural angiographic results previous published are also reported ( Table 1 ).
| Variables | Total | Standard PCI | EM-PCI | p Value |
|---|---|---|---|---|
| (n = 175) | (n = 87) | (n = 88) | ||
| Age (years) | 65.3 ± 11.2 | 64.6 ± 12.5 | 66.7 ± 14.1 | 0.298 |
| Men | 105 (60.0%) | 48 (55.1%) | 57 (64.7%) | 0.218 |
| Risk factors | ||||
| Hypertension | 102 (58.3%) | 43 (49.4%) | 59 (67.0%) | 0.021 |
| Diabetes mellitus | 37 (21.1%) | 16 (18.4%) | 21 (23.8%) | 0.459 |
| Smoking | 66 (37.7%) | 23 (26.4%) | 43 (48.8%) | 0.003 |
| Body mass index >30 kg/m 2 | 7 (4.0%) | 2 (2.3%) | 5 (5.7%) | 0.443 |
| Cholesterol (mg/dl) | 163 ± 27 | 167 ± 15 | 161 ± 11 | 0.002 |
| Triglycerides (mg/dl) | 122 ± 37 | 125 ± 26 | 124 ± 31 | 0.817 |
| Renal failure | 14 (8.0%) | 7 (8.0%) | 7 (7.9%) | 1.00 |
| Killip class III | 42 (24.0%) | 25 (28.7%) | 17 (19.3%) | 0.160 |
| Symptoms to balloon (hours) | 6.1 ± 1.3 | 6.1 ± 1.8 | 6.2 ± 0.9 | 0.642 |
| Left ventricular ejection fraction (%) | 41 ± 13 | 40.7 ± 9.3 | 42 ± 10.5 | 0.192 |
| ST-segment elevation (mV) | 22.9 ± 13.5 | 22.3 ± 9.3 | 23.6 ± 10.5 | 0.384 |
| Procedural characteristics | ||||
| Location of infarct-related coronary artery | ||||
| Left anterior descending | 76 (43.4%) | 38 (43.7%) | 38 (43.2%) | 1.00 |
| Left circumflex | 42 (24.0%) | 20 (23.0%) | 22 (25.0%) | 0.859 |
| Right coronary | 57 (32.6%) | 29 (33.3%) | 28 (31.8%) | 0.872 |
| Bari score (%) | 28.9 ± 10.3 | 28.1 ± 9.2 | 29.7 ± 6.1 | 0.17 |
| Multivessel coronary disease | 37 (26.8%) | 16 (18.4%) | 21 (23.8%) | 0.459 |
| Bifurcation | 23 (13.1%) | 11 (12.7%) | 12 (13.6%) | 1.00 |
| Prethrombectomy thrombus score | ||||
| 3 | 18 (10.3%) | 9 (10.3%) | 9 (10.6%) | 1.00 |
| 4 | 62 (35.4%) | 32 (36.8%) | 30 (34.1%) | 0.753 |
| 5 | 95 (54.3%) | 47 (54.0%) | 48 (54.5%) | 1.00 |
| “Direct” stenting | 69 (39.4%) | 2 (2.3%) | 67 (76.2%) | 0.0001 |
| Drug-eluting stent | 102 (58.3%) | 53 (60.9%) | 49 (55.7%) | 0.540 |
| Creatine kinase-MB peak (ng/ml) | 105 ± 125 | 108 ± 111 | 109 ± 119 | 0.605 |
| 90-minute ST-segment resolution >70% | 90 (51.4%) | 34 (39.1%) | 56 (63.6%) | 0.001 |
| ST-segment elevation (mV) | 10.2 ± 15.3 | 12.8 ± 12.3 | 7.6 ± 9.7 | 0.002 |
| Thrombolysis In Myocardial Infarction flow grade after stenting | ||||
| ≥2 | 174 (99.4%) | 86 (98.9%) | 88 (100%) | 0.975 |
| 0–1 | 1 (0.6%) | 1 (1.1%) | 0 | 0.997 |
| Myocardial blush grade after stenting | ||||
| ≥2 | 130 (74.3%) | 52 (59.8%) | 78 (88.6%) | <0.0001 |
| 0–1 | 45 (25.7%) | 35 (40.2%) | 10 (11.4%) | <0.0001 |
Written questionnaires to obtain information on vital status, hospital admissions, and current medical therapy were available for all patients in each group.
No significant differences in current medical therapy were observed between groups at 2-year follow-up ( Table 2 ).
| Pharmacologic Therapy | Total | Standard PCI | EM-PCI | p Value |
|---|---|---|---|---|
| (n = 169) | (n = 81) | (n = 88) | ||
| Aspirin | 152 (86.8%) | 67 (82.7%) | 76 (86.4%) | 0.53 |
| Clopidogrel | 10 (5.9%) | 4 (4.9%) | 5 (5.7%) | 1.00 |
| Coumarin derivatives | 5 (2.9%) | 2 (2.4%) | 3 (3.4%) | 1.00 |
| Statins | 155 (91.7%) | 74 (91.3%) | 81 (92%) | 1.00 |
| β blocker | 148 (87.6%) | 69 (85.2%) | 79 (89.7%) | 0.44 |
| Calcium channel blockers | 30 (17.7%) | 13 (16.0%) | 17 (19.3%) | 0.68 |
| Nitrates | 15 (8.9%) | 6 (7.4%) | 9 (10.2%) | 0.59 |
| Angiotensin-converting enzyme inhibitor | 100 (59.2%) | 47 (58.0%) | 53 (60.2%) | 0.87 |
| Angiotensin II receptor antagonists | 35 (20.7%) | 15 (18.5%) | 20 (22.7%) | 0.57 |
| Diuretics | 40 (23.7%) | 19 (23.4%) | 21 (23.8%) | 1.00 |
In the control group 6 patients (6.8%) died during 2-year follow-up, with none in the EM-PCI group ( Table 3 ). All deaths were of cardiac origin, of which 4 (4.6%) occurred during first 9 months. According to Kaplan-Meier curves cardiac deaths at 9 months (4.6% vs 0.0%, p = 0.023, log-rank test) and at 2 years (6.8% vs 0.0%, p = 0.012, log-rank test) were significantly lower in the EM-PCI group. At 9 months, no differences were observed in cumulative MACEs (10.3% vs 4.5%, p = 0.14, log-rank test), whereas at 2 years the rate of MACEs was significantly higher in the standard PCI group (13.6% vs 4.5%, p = 0.038, log-rank test; Figure 2 ). No stent thrombosis was observed in either group. Occurrence of cardiac death and MACEs was significantly related to myocardial blush grade and ST-segment resolution ( Figure 3 ). Variables entered in the final model of multivariable analysis for predictors of cardiac death are listed in Table 4 . Independent predictors of cardiac death were randomization to thrombectomy (HR 0.12, 95% CI 0.006 to 0.251, p = 0.006), age (HR 1.508, 95% CI 1.055 to 2.156, p = 0.024), and symptoms to balloon time (HR 1.322, 95 CI 1.078 to 2.156, p = 0.007).
| Variables | Thrombus Aspiration | Conventional PCI | HR (95% CI) | p Value |
|---|---|---|---|---|
| (n = 88) | (n = 87) | |||
| Major adverse clinical events | 4 (4.5%) | 12 (13.6%) | 3.105 (1.002–9.629) | 0.050 |
| Cardiac death | 0 (0%) | 6 (6.8%) ⁎ | 6.657 (1.642–8.457) | 0.0001 |
| Reinfarction | 0 (0%) | 1 (1.1%) | — | 0.999 |
| Target vessel revascularization | 4 (4.5%) | 5 (5.7%) | 1.302 (0.351–4.848) | 0.651 |
| Angiographically proved stent thrombosis | 0 (0%) | 0 (0%) | — | — |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


