Data on the impact of initial Thrombolysis In Myocardial Infarction (TIMI) flow in the culprit coronary artery on myocardial damage after ST-elevation myocardial infarction (STEMI) are limited. Aim of this multicenter study was, therefore, to elucidate the impact of TIMI flow grade before percutaneous coronary intervention (PCI) on infarct size (IS), myocardial salvage index (MSI), and microvascular obstruction (MVO) assessed by cardiac magnetic resonance (CMR) imaging in patients with STEMI. We enrolled 738 patients with STEMI reperfused by primary PCI within 12 hours after symptom onset at 8 centers. Impaired coronary flow was defined as an initial coronary TIMI flow grade ≤1, whereas preserved coronary flow was defined as an initial coronary TIMI flow grade ≥2. CMR was performed in median 3 days (interquartile range 2 to 4 days) after infarction using a standardized infarction protocol. IS, MVO, and MSI were determined in central core laboratory–masked analyses. The primary clinical end point of the study was the time to major adverse cardiac events defined as death, reinfarction, and new onset of heart failure within 12 months after infarction. TIMI flow ≤1 before PCI was present in 507 patients (68.7%) and was significantly associated with larger IS (19% left ventricular [LV] vs 9% LV; p <0.001), less MSI (0.46 vs 0.65; p <0.001), reduced left ventricular ejection fraction (49% vs 55%; p <0.001), and a higher extent of MVO (0.6% LV vs 0.0% LV; p <0.001). Moreover, TIMI flow before PCI was identified as an independent predictor of IS, MVO, and MSI. However, there were no significant differences in major adverse cardiac event rates between groups (6.1% vs 7.5%; p = 0.48). In conclusion, TIMI flow pre-PCI is reversely associated with myocardial injury and is an independent predictor of myocardial damage assessed by CMR.
Despite improved treatment of patients with ST-elevation myocardial infarction (STEMI), the risk of future cardiovascular events in survivors of STEMI remains substantial. Therefore, early assessment of the individual risk after reperfusion therapy is recommended by current guidelines for tailored management and treatment of patients with STEMI. Over the last years, several promising predictors for risk stratification after STEMI were evaluated including different clinical, biochemical, angiographic, and imaging parameters. One extensively studied angiographic parameter is the Thrombolysis In Myocardial Infarction (TIMI) flow grade, a semi-quantitative classification of coronary flow, frequently used in clinical trials to correlate coronary flow before and after primary percutaneous coronary intervention (PCI) with clinical outcome. Patients who underwent PCI in whom initial TIMI flow grade 3 in the culprit coronary artery is present have improved early and late survival rates. The mechanism underlying this survival benefit in these patients is most likely reduced myocardial damage because of less pronounced ischemia in the setting of preserved blood flow and, thus, oxygen supply. Cardiovascular magnetic resonance (CMR) is the reference standard to quantify myocardial injury by means of infarct size (IS), myocardial salvage, and microvascular obstruction (MVO) after acute myocardial infarction. To date, the impact of TIMI flow on CMR markers of myocardial damage has only been assessed in small single-center studies and is, therefore, not precisely explored. Aim of this study was to evaluate the relation between TIMI flow grade before PCI and IS, MVO, and myocardial salvage index (MSI) assessed by CMR imaging in a large cohort of patients with STEMI reperfused by primary PCI.
Methods
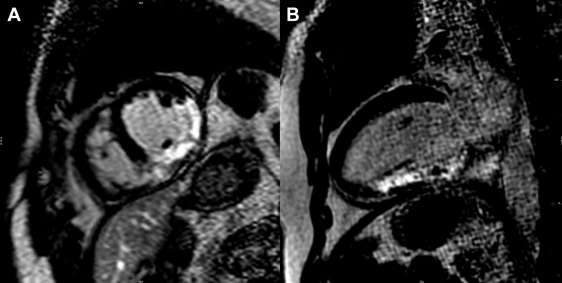
The present study is a subanalysis of the prospective, randomized, multicenter abciximab intravenous versus intracoronary in ST-Elevation Myocardial Infarction (AIDA STEMI) trial. The study randomized 2,065 patients with STEMI reperfused by primary PCI <12 hours after symptom onset to either intracoronary or intravenous abciximab bolus. The trial showed no differences between the treatment groups with respect to the occurrence of major adverse cardiac events (MACE) after 90 days and 12 months. CMR was performed in 795 patients in the predefined AIDA CMR substudy. The design, rationale, and final results including the CMR substudy of AIDA STEMI have previously been published. The study was approved by national regulatory authorities and ethics committees of the participating centers. All patients provided written informed consent. Coronary angiography of the target vessel was performed before and after PCI with the same projections. Visual assessments were performed offline in the angiographic core laboratory by 2 blinded observers. Impaired coronary flow was defined by an initial TIMI flow ≤1 and preserved coronary flow was defined by an initial TIMI flow ≥2. CMR was performed between days 1 and 10 after infarction on a 1.5 or a 3.0 T scanner ( Figure 1 ). A standardized protocol was used to assess IS, MSI, MVO, and left ventricular (LV) ejection fraction and volumes as described before. In brief, cardiac edema imaging was conducted using T2-weighted imaging and cine sequences were used for analysis of function and volume and contrast-enhanced T1-weighted imaging for visualization of myocardial necrosis (15 minutes after contrast injection). Image analysis was performed by blinded observers in a CMR core laboratory. Certified CMR evaluation software (Circle CVI42; Calgary, Alberta, Canada) was used for the quantitative analyses. Semi-automated computer-aided threshold detection was used to identify regions of edema, hypointense core, infarcted myocardium, and MVO, as previously described. MSI was calculated as the area of myocardial edema minus IS divided by the area of myocardial edema multiplied by 100. The primary clinical end point of the study was the time to MACE defined as death, reinfarction, or new onset of congestive heart failure within 12 months after infarction, as previously described.
Continuous data are presented in medians with interquartile range and were compared using the nonparametric Mann-Whitney U test. Categorical and ordinal variables are presented as counts and percentages. Differences between groups with categorical or ordinal variables were evaluated using Pearson’s chi-square test. Univariable and stepwise multivariable linear regression analyses were performed to identify predictors of IS, MVO, and MSI. Multivariable regression was performed using only variables with a p value <0.05 in univariate regression analyses. For univariate analyses, all variables listed in Table 1 were tested. The Kaplan-Meier estimator was used for survival and MACE calculation, and differences between groups were compared using the log-rank test. Univariable and stepwise multivariable Cox regression analyses were performed to identify predictors of MACE. Multivariate regression was again performed using only variables with a p value <0.05 in univariable regression analyses. A 2-tailed p value <0.05 was defined as statistically significant. IBM SPSS, version 23, was used for all statistical analyses.
| Variable | Total study (n=738) | TIMI-flow grade | p-value | |
|---|---|---|---|---|
| 0-1 (n=507) | 2-3 (n=231) | |||
| Age (years) | 62 (51-71) | 61 (50-71) | 63 (52-71) | 0.57 |
| Women | 179/738 (24%) | 129/507 (25%) | 50/231 (22%) | 0.26 |
| Current smoker | 317/674 (47%) | 211/465 (45%) | 106/209 (51%) | 0.20 |
| Hypertension | 492/735 (67%) | 336/505 (66%) | 156/230 (68%) | 0.69 |
| Hypercholesterolemia | 264/730 (36%) | 167/500 (33%) | 97/230 (42%) | 0.02 |
| Diabetes mellitus | ||||
| Any | 142/735 (19%) | 91/504 (18%) | 51/231 (22%) | 0.20 |
| Insulin requiring | 68/735 (10%) | 46/504 (9%) | 23/231 (10%) | 0.66 |
| Family history of CAD | 251/572 (44%) | 176/399 (44%) | 75/173 (43%) | 0.87 |
| Body mass index (kg/m 2 ) | 27.3 (24.8-30.2) | 27.4 (24.9-30.6) | 27.1 (24.8-30.0) | 0.14 |
| Anterior wall infarct | 339/704 (48%) | 229/485 (47%) | 110/219 (50%) | 0.46 |
| Systolic blood pressure (mmHg) | 130 (117-147) | 130 (114-145) | 135 (120-150) | 0.005 |
| Diastolic blood pressure (mmHg) | 80 (70-87) | 80 (70-87) | 80 (70-87) | 0.41 |
| Heart rate (beats per minute) | 76 (67-86) | 77 (68-89) | 75 (66-84) | 0.54 |
| Times (minutes) | ||||
| Symptom onset to PCI hospital admission | 180 (109-317) | 185 (109-335) | 165 (108-285) | 0.10 |
| Door-to-balloon-time | 30 (22-42) | 30 (21-43) | 29 (23-42) | 0.91 |
| Pain-to-balloon-time | 216 (143-354) | 220 (143-368) | 199 (140-317) | 0.07 |
| Killip-class on admission | 0.23 | |||
| 1 | 653/738 (88%) | 441/507 (87%) | 212/231 (92%) | |
| 2 | 52/738 (7%) | 39/507 (8%) | 13/231 (6%) | |
| 3 | 18/738 (2%) | 14/507 (3%) | 4/231 (2%) | |
| 4 | 15/738 (2%) | 13/507 (3%) | 2/231 (1%) | |
| Number of narrowed coronary arteries | 0.58 | |||
| 1 | 397/738 (54%) | 276/507 (54%) | 120/231 (52%) | |
| 2 | 208/738 (28%) | 136/507 (27%) | 72/231 (31%) | |
| 3 | 133/738 (18%) | 95/507 (19%) | 39/231 (17%) | |
| Infarct related artery | 0.69 | |||
| Left anterior descending | 324/738 (44%) | 224/507 (44%) | 100/231 (43%) | |
| Left circumflex | 85/738 (12%) | 58/507 (11%) | 27/231 (12%) | |
| Right | 326/738 (44%) | 223/507 (44%) | 102/231 (44%) | |
| Left main | 3/738 (0%) | 1/507 (0%) | 2/231 (1%) | |
| TIMI-flow before PCI | <0.001 | |||
| 0 | 408/738 (55%) | 408/507 (80%) | 0/231 (0%) | |
| I | 99/738 (13%) | 99/507 (20%) | 0/231 (0%) | |
| II | 121/738 (16%) | 0/507 (0%) | 121/231 (52%) | |
| III | 110/738 (15%) | 0/507 (0%) | 110/231 (48%) | |
| Stent implanted | ||||
| Drug eluting stent | 318/737 (43%) | 208/507 (41%) | 110/230 (48%) | 0.08 |
| Bare metal stent | 433/737 (59%) | 304/507 (60%) | 129/230 (56%) | 0.32 |
| Thrombectomy | 179/738 (24%) | 149/507 (29%) | 30/231 (13%) | <0.001 |
| TIMI-flow post PCI | 0.001 | |||
| 0 | 9/737 (1%) | 9/506 (2%) | 0/231 (0%) | |
| I | 19/737 (3%) | 16/506 (3%) | 3/231 (1%) | |
| II | 54/737 (7%) | 47/506 (9%) | 7/231 (3%) | |
| III | 656/737 (89%) | 434/506 (86%) | 221/231 (96%) | |
| Intraaortic balloon pump | 31/738 (4%) | 26/507 (5%) | 5/231 (2%) | 0.06 |
| Peak creatine kinase 48 h (μmol/l/s) | 26.0 (11.8-45.8) | 32.6 (17.4-53.1) | 12.9 (6.3-24.9) | <0.001 |
| ST-segment resolution at 90 min (%) | 55 (22-78) | 52 (19-77) | 61 (29-80) | 0.18 |
| Concomitant medications | ||||
| ß-blockers (on discharge) | 707/736 (96%) | 485/507 (96%) | 220/229 (96%) | 0.80 |
| ACE-I/ARB | 701/736 (95%) | 482/507 (95%) | 219/229 (96%) | 0.74 |
| Aspirin | 738/738 (100%) | 507/507 (100%) | 231/231 (100%) | -/- |
| Clopidogrel | 627/713 (88%) | 426/490 (87%) | 201/223 (90%) | 0.22 |
| Prasugrel | 167/564 (30%) | 123/389 (32%) | 44/175 (25%) | 0.12 |
| Ticagrelor | 0/0 (0%) | 0/0 (0%) | 0/0 (0%) | -/- |
| Statins (on discharge) | 703/736 (96%) | 476/507 (94%) | 227/229 (99%) | 0.001 |
| Aldosterone antagonists (on discharge) | 89/736 (12%) | 67/507 (13%) | 22/229 (10%) | 0.17 |
Results
From July 2008 to April 2011, 795 patients were enrolled in the AIDA STEMI CMR substudy. Patients with previous infarction and incomplete or insufficient CMR data were excluded. The final study group comprised 738 patients ( Figure 2 ). The baseline characteristics are listed in Table 1 according to impaired or preserved TIMI flow before PCI. Most cardiovascular risk factors (smoking, hypertension, and diabetes mellitus) and reperfusion times did not differ significantly between the groups. In the impaired TIMI flow group, less patients had hypercholesterolemia and a higher peak CK value within 48 hours was observed ( Table 1 ). No significant differences could be found between groups regarding the number of diseased vessels and/or the infarct-related artery. Thrombectomy devices and intra-aortic balloon pumps were used more frequently in patients with impaired TIMI flow pre-PCI ( Table 1 ). The median time between the index event and CMR was 3 days (interquartile range 2 to 4 days) for both groups (p = 0.70). Most patients underwent CMR on a 1.5-T scanner (97%). The main findings from CMR analyses are presented in Table 2 . Almost all CMR parameters of myocardial injury showed significant differences between both groups. Patients with impaired TIMI flow had significantly larger IS, a higher extent of MVO, and less MSI. Impaired TIMI flow before PCI was an independent predictor of IS, MVO, and myocardial salvage ( Tables 3 to 5 ). Furthermore, there was a clear evidence for a graded inverse relation between TIMI flow pre-PCI and IS ( Figure 3 ) or MVO ( Figure 4 ) and a graded relation between TIMI flow pre-PCI and MSI ( Figure 5 ). The follow-up after 12 months was completed in all patients. The combined primary clinical end point and the individual clinical end points did not differ between both groups ( Table 6 ). Kaplan-Meier curves demonstrated also no significant differences according to the initial TIMI-flow pre-PCI ( Figure 6 ). Using Cox regression analysis, impaired TIMI-flow before PCI was not an independent predictor for MACE (data not shown).
| Variable | Total Study (n=738) | TIMI-flow grade | p-value | |
|---|---|---|---|---|
| 0-1 (n=507) | 2-3 (n=231) | |||
| Left ventricular ejection fraction (%) | 51 (44-58) | 49 (42-56) | 55 (47-61) | <0.001 |
| End-diastolic volume (ml) | 146 (121-172) | 149 (124-176) | 138 (113-162) | <0.001 |
| End-systolic volume (ml) | 72 (54-91) | 76 (58-96) | 62 (48-82) | <0.001 |
| Infarct size (%LV) | 17 (8-25) | 19 (12-27) | 9 (3-18) | <0.001 |
| Microvascular obstruction (%LV) | 0.0 (0.0-1.7) | 0.6 (0.0-2.7) | 0.0 (0.0-0.2) | <0.001 |
| Myocardial salvage (%) | 17 (9-27) | 17 (9-25) | 18 (10-30) | 0.01 |
| Myocardial salvage index | 51 (33-69) | 46 (29-62) | 65 (46-89) | <0.001 |
| Hypointense core of infarcted myocardium | 224/654 (34%) | 189/447 (42%) | 35/207 (17%) | <0.001 |
| Hypointense core (%LV) | 0.0 (0.0-1.6) | 0.0 (0.0-2.7) | 0.0 (0.0-0.0) | <0.001 |
| Edema (%LV) | 35 (25-48) | 35 (25-47) | 38 (27-49) | 0.08 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


