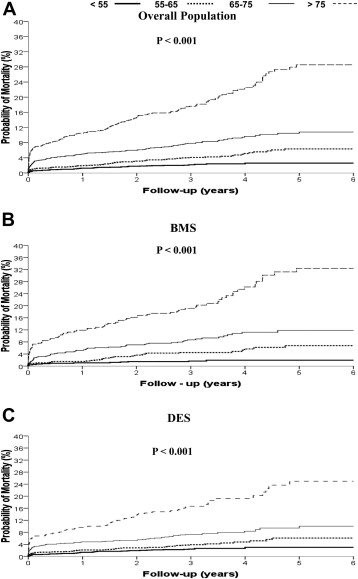
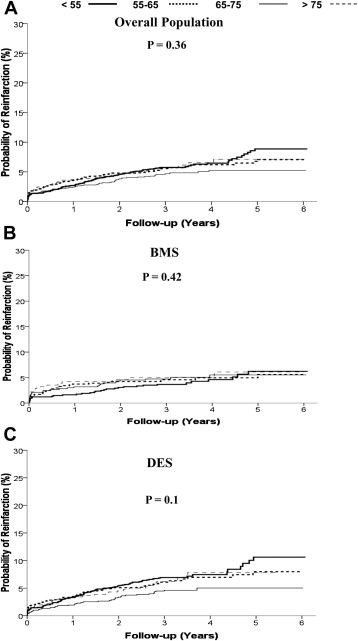
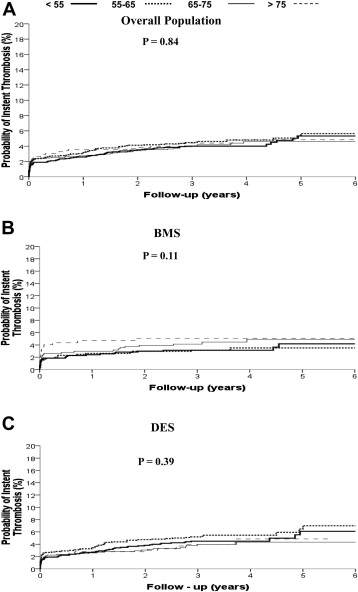
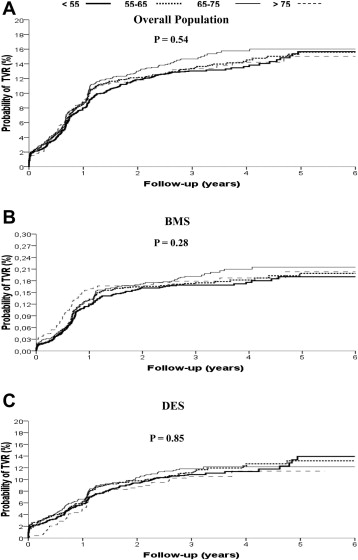
Despite mechanical reperfusion, elderly patients with ST-segment elevation myocardial infarction (STEMI) still experience unsatisfactory outcomes. Drug-eluting stents (DES) have significantly reduced target-vessel revascularization (TVR), but concerns have emerged about the higher risk of late stent thrombosis, which may be more pronounced in elderly patients. Therefore, the aim of this study was to evaluate the impact of age on outcome in patients with STEMI who underwent primary angioplasty with bare-metal stents (BMS) or DES. Our population comprised 6,298 patients who underwent primary angioplasty and stent implantation included in the Drug-Eluting Stent in Primary Angioplasty (DESERT) Cooperation database. Age was significantly associated with female gender (p <0.001), diabetes (p <0.001), hypertension (p <0.001), previous myocardial infarction (MI; p <0.001), ischemia time (p <0.001), and anterior MI (p <0.001) but inversely related to smoking (p <0.001). Elderly patients most often had infarct-related artery located in the descending artery (p = 0.014) and impaired postprocedural thrombolysis in myocardial infarction flow (p <0.001). Elderly patients were less often on clopidogrel at follow-up. At long-term follow-up, age was associated with a higher rate of death (hazard ratio [95% confidence interval] = 2.17 [1.97 to 2.39], p <0.0001), whereas no impact was observed on reinfarction (p = 0.36), stent thrombosis (p = 0.84), and TVR (p = 0.54). These results were confirmed in patients receiving both BMS and DES. The impact of age on mortality was confirmed after correction for baseline confounding factors (gender, diabetes hypertension, hypercholesterolemia, smoking, ischemia time, anterior MI, infarct-related artery location, and postprocedural thrombolysis in myocardial infarction 3 flow; adjusted hazard ratio [95% confidence interval] = 2.13 [1.78 to 2.56], p <0.001). In conclusion, this study shows that in patients with STEMI who underwent primary angioplasty, age is independently associated with higher mortality, observed with both BMS and DES, whereas no impact was observed on the rate of reinfarction, stent thrombosis, and TVR.
Primary angioplasty currently represents the best reperfusion therapy for the treatment of ST-segment elevation myocardial infarction (STEMI). Further improvement has been attained by optimization of antithrombotic therapies and adjunctive mechanical devices. Special attention has been paid to elderly patients in recent years, because older age is associated with increased mortality in patients with STEMI who have undergone primary angioplasty. Poor myocardial perfusion has recently been shown to contribute to poor outcome, in addition to several known factors, such as the presence of co-morbidities, more severe coronary artery disease, and impaired left ventricular function. In addition, elderly patients are at higher risk for major bleeding complications, which may potentially contribute to premature discontinuation of dual antiplatelet therapy and therefore increase the risk of stent thrombosis (ST), especially in the era of drug-eluting stents (DES). Therefore, the aim of the present study was to evaluate the impact of age on clinical outcome in patients with STEMI who underwent primary angioplasty with bare-metal stents (BMS) or DES.
Methods
Our population comprised patients with STEMI included in the Drug-Eluting Stent in Primary Angioplasty (DESERT) Cooperation. Detailed data have been previously described. Briefly, we collected data from 11 randomized trials on DES in STEMI, including baseline characteristics (age, gender, diabetes, hypertension, hypercholesterolemia, smoking, previous revascularization, infarct location, ischemia time), major angiographic variables (preprocedural thrombolysis in myocardial infarction [TIMI] flow, infarct-related artery, postprocedural TIMI flow, use of glycoprotein IIb-IIIa inhibitors), and complete follow-up data, such as mortality, reinfarction, target-vessel revascularization (TVR), and stent thrombosis (defined according to the Academic Research Consortium definite or probable definition). A temporal analysis was performed for stent thrombosis divided into acute (<24 hours), subacute (24 hours to 30 days), late (1 to 12 months), and very late (later than 12 months follow-up) events.
Statistical analysis was performed with the SPSS 15.0 statistical package (SPSS Inc., Chicago, Illinois). Continuous data were expressed as mean ± SD and categorical data as percentage. The analysis of variance was appropriately used for continuous variables. The chi-square test or the Fisher’s exact test was used for categorical variables. A trend analysis was performed as previously described. The difference in event rates between groups during the follow-up period was assessed by the Kaplan-Meier method using the log-rank test. Cox proportional hazard method analysis was used to calculate hazard ratios adjusted for differences in baseline clinical and angiographic characteristics, which were all entered in block. A p value <0.05 was considered statistically significant.
Results
Our population is represented by 6,298 patients with STEMI. Baseline characteristics according to age are reported in Table 1 . Age was significantly associated with female gender (p <0.001), diabetes (p <0.001), hypertension (p <0.001), previous myocardial infarction (p <0.001), ischemia time (p <0.001), and anterior myocardial infarction (p <0.001) but inversely related with smoking (p <0.001). Elderly patients most often had infarct-related artery located in the descending artery (p = 0.014) and impaired postprocedural TIMI flow (p <0.001). Glycoprotein IIb-IIIa inhibitors were administrated equally among different groups. As reported in Table 1 , elderly patients were less often on clopidogrel at follow-up.
| Clinical Characteristics | Age (yrs) | p Value | |||
|---|---|---|---|---|---|
| <55 (n = 2,073) | 55–65 (n = 1,869) | 65–75 (n = 1,489) | >75 (n = 891) | ||
| Age (mean ± SD) | 47.5 ± 5.4 | 59.6 ± 2.8 | 69.5 ± 2.8 | 79.8 ± 2.9 | <0.001 |
| Men | 85.4% | 80% | 72.9% | 55.6% | <0.001 |
| Diabetes mellitus | 11.7% | 14.6% | 19.9% | 18.7% | <0.001 |
| Hypercholesterolemia | 33.3% | 38.2% | 31.9% | 29.7% | <0.001 |
| Smoker | 69.1% | 51.7% | 37.1% | 19.7% | <0.001 |
| Arterial hypertension | 33.9% | 44.9% | 50.8% | 54% | <0.001 |
| Previous MI | 4.6% | 6.4% | 10.3% | 10% | <0.001 |
| Previous revascularization | 4.5% | 5.7% | 7.3% | 6.2% | 0.08 |
| Symptom onset to balloon time (min) mean ± SD | 244 ± 171 | 257 ± 225 | 277 ± 285 | 283 ± 225 | <0.001 |
| Anterior MI | 43.4% | 42% | 45.9% | 48.2% | <0.001 |
| Preprocedural TIMI flow | 0.27 | ||||
| 0–1 | 80% | 81.6% | 82.1% | 80.3% | |
| 2 | 20% | 18.4% | 17.9% | 19.7% | |
| Multivessel disease | 29.7% | 34.6% | 42.3% | 47.7% | <0.001 |
| Postprocedural TIMI flow 3 | 90.2% | 87.1% | 85.4% | 82.5% | <0.001 |
| DES | 63.6% | 65% | 61.3% | 61.7% | 0.12 |
| Type of DES | 0.06 | ||||
| Cypher | 28.4% | 25.3% | 26.9% | 25.3% | |
| Taxus | 70.5% | 74.0% | 72.4% | 72.3% | |
| Endeavor | 1.1% | 0.7% | 0.7% | 2.4% | |
| Glycoprotein IIb-IIIa inhibitors | 70.4% | 69.7% | 70.6% | 71.4% | 0.83 |
| Infarct-related artery | 0.014 | ||||
| LM | 0.1% | 0.1% | 0.3% | 0.1% | |
| LAD | 43% | 40.3% | 45.6% | 47.7% | |
| AL | 0.1% | 0.1% | 0.3% | 0.1% | |
| LCX | 14.3% | 12.7% | 12.2% | 13.2% | |
| RCA | 41.6% | 45.5% | 39.9% | 37.5% | |
| Graft | 0% | 0.1% | 0.1% | 0.1% | |
| DAT at follow-up (mo) | |||||
| 6 | 92.5% | 93.2% | 91.2% | 89.6% | 0.001 |
| 12 | 63.8% | 65.6% | 63% | 59% | 0.03 |
| 24 | 16.9% | 18.4% | 15.3% | 15.5% | 0.15 |
| 36 | 12.2% | 12.9% | 10.1% | 10.2% | 0.083 |
Follow-up data were available at a mean of 1,201 ± 441 days. At long-term follow-up, age was associated with a significantly higher rate of death (hazard ratio [HR; 95% confidence interval, CI] = 2.17 [1.97 to 2.39], p <0.0001; Figure 1 ), whereas no impact was observed in terms of reinfarction (HR [95% CI] = 0.95 [0.86 to 1.06], p = 0.36; Figure 2 ), stent thrombosis (HR [95% CI] = 1.01 [0.9 to 1.14], p = 0.84; Figure 3 ), and TVR (HR [95% CI] = 1.02 [0.96 to 1.09], p = 0.54; Figure 4 ). These results were confirmed in both patients receiving BMS or DES ( Table 2 , Figures 1 to 4 ). The impact of age on mortality was confirmed after correction for baseline confounding factors (gender, diabetes, hypertension, hypercholesterolemia, smoking, ischemia time, anterior myocardial infarction, infarct-related artery location, and postprocedural TIMI 3 flow; adjusted HR [95% CI] = 2.13 [1.78 to 2.56], p <0.001; Table 3 ).