This study was undertaken to assess the impact of acute hyperglycemia (acute-HG) and chronic hyperglycemia (chronic-HG) on short-term outcomes in patients with acute myocardial infarction (AMI). This study consisted of 696 patients with AMI. Acute-HG was defined as admission plasma glucose ≥200 mg/dl and chronic-HG as hemoglobin A1c ≥6.5%. Acute-HG was associated with higher peak serum creatine kinase (4,094 ± 4,594 vs 2,526 ± 2,227 IU/L, p <0.001) and in-hospital mortality (9.8% vs 1.6%, p <0.001). On the contrary, there was no significant difference in peak creatine kinase (2,803 ± 2,661 vs 2,940 ± 3,181 IU/L, p = 0.59) and mortality (3.3 vs 3.7%, p = 0.79) between patients with chronic-HG and those without. Multivariate analysis showed that admission plasma glucose was an independent predictor of in-hospital mortality (odds ratio 1.15, 95% confidence interval 1.05 to 1.27, p <0.001), but hemoglobin A1c was not. When only patients with acute-HG were analyzed, chronic-HG was associated with a significantly smaller infarct size (3,221 ± 3,001 vs 5,904 ± 6,473 IU/L, p <0.001) and lower in-hospital mortality (5.5 vs 18.9%, p = 0.01). In conclusion, these results suggested that acute-HG, but not chronic-HG, was associated with adverse short-term outcomes after AMI. Paradoxically, in patients with acute-HG, chronic-HG might abate the adverse effects of acute-HG.
Highlights
- •
Acute hyperglycemia is associated with large infarct size and high in-hospital mortality in patients with acute myocardial infarction.
- •
Infarct size and in-hospital mortality are not different between patients with chronic hyperglycemia and those without.
- •
Paradoxically, chronic hyperglycemia may abate the adverse effects of acute hyperglycemia.
It has been reported that hyperglycemia (HG) causes oxidative stress, enhances inflammation, induces apoptosis, and activates coagulation, which deteriorate myocardial damage in the setting of ischemia. In the clinical practice, admission plasma glucose is used as a measure of acute-HG and hemoglobin A1c (HbA1c) for chronic-HG. However, it remains unclear how acute-HG and chronic-HG affect short-term outcomes in patients with acute myocardial infarction (AMI). The purpose of the present study was to investigate impact of acute-HG and chronic-HG on short-term outcomes after AMI.
Methods
From January 2007 to June 2012, 760 consecutive patients who were admitted to National Cerebral and Cardiovascular Center of Japan within 48 hours after the onset of AMI were prospectively enrolled to the observational single-center registry and were retrospectively analyzed. In this registry, AMI was defined by a combination of 2 of the following 3: chest pain longer than 30 minutes, electrocardiographic signs, and elevation of serum creatine kinase more than twice the upper normal limit. Patients for whom laboratory data were lacking (n = 64) were excluded from the present study. Finally, this study consisted of the remaining 696 patients who constituted the study population with short-term clinical follow-up. The allocation of emergency coronary angiography and coronary intervention was determined by the physician’s decision. The study protocol was approved by the Institutional Review Board of National Cerebral and Cardiovascular Center and was conducted in accordance with regulations governing epidemiological studies issued by the Ministry of Health, Labor, and Welfare of Japan.
On admission, age, gender, body mass index, and co-morbidities such as hypertension, diabetes, dyslipidemia, smoker, and previous myocardial infarction were recorded. Plasma glucose was obtained at the time of admission, and HbA1c, during hospitalization. Serum creatine kinase was measured every 3 hours until it reached the peak value. Acute-HG was defined as admission plasma glucose ≥200 mg/dl. Chronic-HG was defined as HbA1c ≥6.5%. Chronic kidney disease is defined as estimated glomerular filtration rate ≤30 ml/min/1.73 m 2 in this study.
Continuous data were shown as mean ± SD. Continuous variables were compared by use of the t test and categorical variables with chi-square statistics or Fisher’s exact test. Logistic regression analysis was used to obtain odds ratio (OR) and 95% confidence interval (CI) for in-hospital mortality. In multivariate analysis, the association between acute-HG and chronic-HG were adjusted for baseline variables, including age, gender, smoker, previous myocardial infarction, elapsed time, ST-elevation myocardial infarction, Killip classification ≥2, and primary coronary intervention. Multivariate analysis was also performed when plasma glucose and HbA1c were analyzed as a continuous variable. Values of p <0.05 were considered statistically significant. All statistical analyses were performed using JMP (version 11.0, SAS Inc., Tokyo, Japan).
Results
This study consisted of 696 patients. A total of 652 patients (94%) underwent emergency coronary angiography. Primary coronary intervention was performed in 606 patients (87%), mostly with stents (92%). Final Thrombolysis In Myocardial Infarction grade 3 flow was obtained in 553 patients (91%).
Acute-HG was found in 163 patients (23%). Table 1 lists the baseline characteristics of patients with and without acute-HG. Patients with acute-HG had significantly higher plasma glucose on admission (276 ± 75 vs 139 ± 28 mg/dl, p <0.001) and HbA1c (7.2 ± 1.9 vs 5.6 ± 0.8%, p <0.001) than those without acute-HG. Acute-HG was associated with more diabetes, more chronic kidney disease, more Killip classification ≥2, and higher body mass index.
| Variables | Acute Hyperglycemia | p Value | |
|---|---|---|---|
| Yes (n=163) | No (n=533) | ||
| Age (yrs) | 68.7 ± 11.9 | 67.4 ± 12.8 | 0.268 |
| Men | 72% | 72% | 0.921 |
| Body mass index (kg/m 2 ) | 24.4 ± 3.8 | 23.3 ± 3.7 | 0.002 |
| Diabetes Mellitus | 69% | 24% | <0.001 |
| Hypertension | 72% | 66% | 0.214 |
| Dyslipidemia | 61% | 54% | 0.105 |
| Smoker | 32% | 33% | 0.964 |
| Chronic kidney disease | 48% | 29% | <0.001 |
| Previous myocardial infarction | 9% | 10% | 0.881 |
| ST elevation myocardial infarction | 80% | 84% | 0.342 |
| Anterior location | 39% | 39% | 1.000 |
| Killip class 2 to 4 | 35% | 14% | <0.001 |
| Elapsed time (hour) | 7.1 ± 10.2 | 7.5 ± 9.7 | 0.701 |
| Primary percutaneous coronary intervention | 90% | 86% | 0.349 |
| Medication before infarction | |||
| Antiplatelet agent | 21% | 18% | 0.494 |
| Angiotensin-converting enzyme inhibitors and/or angiotensin receptor blockers | 31% | 22% | 0.021 |
| Calcium-channel blocker | 27% | 26% | 0.919 |
| Beta-blocker | 12% | 10% | 0.562 |
| Statin | 23% | 17% | 0.066 |
| Oral hypoglycemic agent | 29% | 8% | <0.001 |
| Insulin | 9% | 2% | <0.001 |
There were 212 (30%) patients with chronic-HG. The baseline characteristics of patients with chronic-HG and without chronic-HG were listed in Table 2 . Both admission plasma glucose and HbA1c were higher in patients with chronic-HG than without chronic-HG (223 ± 86 vs 148 ± 52 mg/dl, p <0.001 and 7.5 ± 1.5 vs 5.4 ± 0.3%, p <0.001, respectively). Chronic-HG was associated with more diabetes and more dyslipidemia.
| Variables | Chronic Hyperglycemia | p Value | |
|---|---|---|---|
| Yes (n=212) | No (n=484) | ||
| Age (yrs) | 68.6 ± 12.4 | 67.3 ± 12.7 | 0.192 |
| Men | 74% | 71% | 0.583 |
| Body mass index (kg/m 2 ) | 24.4 ± 3.9 | 23.2 ± 3.7 | <0.001 |
| Diabetes Mellitus | 83% | 13% | <0.001 |
| Hypertension | 73% | 65% | 0.065 |
| Dyslipidemia | 62% | 53% | 0.031 |
| Smoker | 34% | 32% | 0.736 |
| Chronic kidney disease | 36% | 32% | 0.296 |
| Previous myocardial infarction | 8% | 10% | 0.491 |
| ST elevation myocardial infarction | 80% | 84% | 0.229 |
| Anterior location | 36% | 41% | 0.238 |
| Killip class 2 to 4 | 20% | 19% | 0.754 |
| Elapsed time (hour) | 8.1 ± 10.3 | 7.1 ± 9.6 | 0.206 |
| Primary percutaneous coronary intervention | 88% | 87% | 0.711 |
| Medication before infarction | |||
| Antiplatelet agent | 20% | 18% | 0.600 |
| Angiotensin-converting enzyme inhibitors and/or angiotensin receptor blockers | 31% | 21% | 0.007 |
| Calcium-channel blocker | 27% | 26% | 0.926 |
| Beta-blocker | 10% | 11% | 1.000 |
| Statin | 22% | 18% | 0.090 |
| Oral hypoglycemic agent | 35% | 4% | <0.001 |
| Insulin | 9% | 1% | <0.001 |
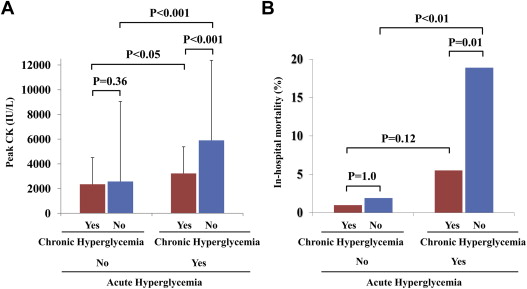
Peak creatine kinase was obtained in 691 patients (99%). Patients with acute-HG had a significantly higher peak creatine kinase than those without (p <0.001; Figure 1 ). There was no significant difference in peak creatine kinase between patients with chronic-HG and those without (p = 0.59; Figure 1 ). In-hospital mortality rate was significantly higher in patients with acute-HG than in those without (p <0.001; Figure 1 ), but chronic-HG was not associated with in-hospital mortality (p = 0.79; Figure 1 ).
In univariate analysis, acute-HG was associated with a sixfold increase in in-hospital mortality risk (OR 6.34, 95% CI 2.8 to 15.3, p <0.001). When plasma glucose was analyzed as a continuous variable, an increase of 1 mmol/L (18 mg/dl) in plasma glucose was associated with an increase in mortality risk of 18% (OR 1.18, 95% CI 1.10 to 1.26, p <0.001). On the contrary, chronic-HG (OR 0.88, 95% CI 0.34 to 2.06, p = 0.79) and HbA1c (OR 1.14, 95% CI 0.85 to 1.43, p = 0.31) were not predictive factors of in-hospital mortality.
In multivariate analysis, acute-HG was independently associated with in-hospital mortality (OR 6.35, 95% CI 2.29 to 18.9, p <0.001), but chronic-HG was not (OR 0.47, 95% CI 0.15 to 1.37, p = 0.16). Analyzed as a continuous variable, plasma glucose was an independent predictor for in-hospital mortality (OR 1.21, 95% CI 1.09 to 1.35, p <0.001), but HbA1c was not (OR 0.85, 95% CI 0.57 to 1.20, p = 0.36).
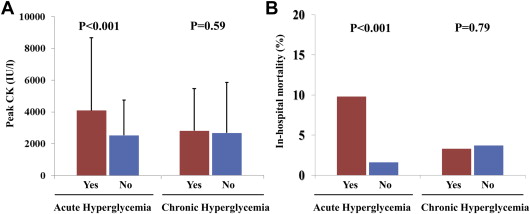
Peak creatine kinase and in-hospital mortality are shown in Figure 2 , stratified according to acute-HG and chronic-HG. Acute-HG was associated with large infarct size and high in-hospital mortality in both patients with and without chronic-HG. In 528 patients without acute-HG, there was no significant difference in peak creatine kinase and in-hospital mortality between patients with and without chronic-HG. On the contrary, in 163 patients with acute-HG, chronic-HG was associated with smaller peak creatine kinase and lower in-hospital mortality.