There are limited data regarding the effect of age on the risk of ventricular tachyarrhythmias (VTAs). The present study was designed to compare the risk for VTAs in young and older patients with left bundle branch block (LBBB) and mildly symptomatic heart failure who receive device therapy. The risk of the first ventricular tachycardia (VT) or ventricular fibrillation (VF) event and the risk of first appropriate implantable cardioverter defibrillator (ICD) shock was compared between young (<75 years, n = 1,037) and older (≥75 years, n = 227) patients with LBBB enrolled in Multicenter Automatic Implantation Trial with Cardiac Resynchronization Therapy. The cumulative incidence of a first VTA through 2 years of follow-up was significantly lower in older patients than in younger patients. Multivariate analysis showed that older patients experienced a significantly lower risk of VT/VF (hazard ratio 0.38, 95% confidence interval 0.22 to 0.64, p <0.001) and a significantly lower risk of appropriate ICD shocks (hazard ratio 0.37, 95% confidence interval 0.17 to 0.82, p = 0.014) compared with younger patients. Each increasing decade of life was associated with a 19% (p = 0.002) and 22% (p = 0.018) reduction in the risk of VT/VF and appropriate ICD shocks, respectively. The lower risk of VT/VF and appropriate ICD shocks in older patients was evident in patients implanted with an ICD only and in those implanted with a cardiac resynchronization therapy with defibrillator. In conclusion, in patients with LBBB and mild symptoms of heart failure, aging is associated with a significant decrease in the incidence of VT/VF and ICD shocks.
Aging is associated with a variety of structural and functional changes in the cardiovascular system affecting cardiovascular reserves and lowering the threshold for clinical manifestation of heart failure (HF). The prevalence of HF and the mortality associated with HF increases directly with age. Cardiac resynchronization therapy (CRT) provides significant reductions in morbidity and mortality in patients with left ventricular (LV) systolic dysfunction and advanced HF symptoms. More recently, the Multicenter Automatic Implantation Trial with Cardiac Resynchronization Therapy (MADIT-CRT) demonstrated the efficacy of CRT in patients with LV systolic dysfunction and mild symptoms of HF, particularly in those with left bundle branch block (LBBB). In older patients, CRT has been shown to significantly reduce the risk of HF or death ; however, the risk of life-threatening ventricular tachycardia (VT) or ventricular fibrillation (VF) in young and older patients has not been well characterized. In the present study, we aimed to evaluate the risk of VT and VF as a function of age in patients with LBBB enrolled in MADIT-CRT.
Methods
The design and results from MADIT-CRT have previously been published. Briefly, 1,820 patients enrolled at 110 hospitals in the United States, Canada, and Europe were randomized in a 3:2 ratio to receive CRT with a defibrillator (CRT-D) or an implantable cardioverter defibrillator (ICD) therapy. Patients of either gender who were at least 21 years were enrolled if they had ischemic cardiomyopathy (New York Heart Association [NYHA] functional class I or II) or nonischemic cardiomyopathy (NYHA functional class II only), normal sinus rhythm, an LV ejection fraction ≤30%, and a QRS duration of ≥130 milliseconds (ms).
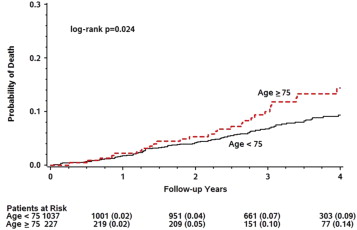
Age at enrollment in the trial was recorded for all patients. For this substudy, we restricted the analysis to include only patients with an LBBB pattern on the baseline electrocardiogram as this population has been identified as patients in whom CRT-D is most beneficial and for whom current guidelines for device-based therapy of cardiac rhythm abnormalities have recommended CRT-D therapy. The rate of death between young and older patients within 2 years of device implant was similar ( Figure 1 ). Therefore, to account for the competing risk of death associated with aging, we restricted our analysis to within 2 years of device implant.
Patients enrolled and randomized in the trial underwent implantation of either a CRT-D or ICD system. Devices were programmed to monitor + therapy, with a protocol recommendation to a setting of the VT zone at 180 beats/min and the VF zone at 210 beats/min. Sensitivity was programmed according to physician discretion. A detection delay of 2.5 seconds for the VT zone and 1.0 seconds for the VF zone was recommended. The protocol suggested programming the VT zone first therapy to burst-type antitachycardia pacing with 8 pulses at 88% of the measured cycle length with a 10-millisecond decrement between bursts and then shock therapy.
All devices were interrogated quarterly and after any ICD shock therapies. All device interrogations and arrhythmia episodes were adjudicated in a core laboratory. The definition of VT in this particular analysis was set to a rate from 180 beats/min (recommended programming) up to 250 beats/min using the stored electrograms of the episode, if the rate of the ventricular electrograms (V) was greater than the rate of the atrial electrograms (A) and if there was a 1:1 AV-conduction V-V changes were driving A-A changes. VF was defined as ventricular rate faster than 250 beats/min with disorganized ventricular electrograms. In this analysis, only appropriate therapy delivered for VT or VF was considered. The analysis was performed on an intention to treat basis.
“Younger patients” were defined as <75 years and older patients as ≥75 years. “Sudden cardiac death” (SCD) was defined using a modified Hinkle-Thaler system and categorized by an independent mortality review committee, as previously described. The “primary end point” in the present study was the first occurrence of appropriate device therapy for VT/VF, whichever occurred first. “Secondary end points” included the following events: VT/VF or death, VT/VF or SCD, appropriate therapy for VT alone, appropriate therapy for VF alone, and appropriate ICD shock therapy.
Baseline characteristics of study patients by age group were compared with the Wilcoxon rank-sum test for continuous variables and the chi-square test for categorical variables. Cumulative incidence rates were estimated for the end point of VT/VF separately for patients in the CRT-D arm and in the ICD-only arm. The test of Fine and Gray was used to test the differences in cumulative incidence between age groups. The method of Kaplan-Meier was used to estimate cumulative event probabilities for end points including death. Multivariate Cox proportional hazards regression modeling was performed to estimate the relative risk for VT/VF and for death between older and younger patients and with age assessed as a continuous variable (per 10-year increments).
The best subset regression procedure was used to identify significant variables to be included in the multivariate regression model. The variables that were included are treatment with CRT-D, gender, ischemic etiology, QRS ≥150 ms, and LV end-systolic volume index. Additionally, ischemic status was forced into the multivariate models. Otherwise, only variables that reached significance of <0.05 were included. Negative binomial regression was used to test the rates of recurrent VT/VF episodes in the age groups with all events censored at 2 years of follow-up or up to 10 recurrent events, whichever came first. All p values are 2 tailed. Interaction p-values were computed and reported between treatment with a CRT-D and the effect of age on end points. All analyses were on an intention-to-treat basis. Analyses were performed with version 4.0 of the MADIT-CRT database using SAS software (version 9.3; SAS Institute, Cary, NC).
Results
Baseline characteristics in young compared with older patients are listed in Table 1 . Young patients were more likely to have wider QRS intervals, whereas older patients were more likely to have hypertension, renal dysfunction, and ischemic cardiomyopathy. The use of angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and statins were similar between the 2 groups; however, older patients were less likely to be on β-blocker therapy. Echocardiographic parameters exhibited lower LV end-diastolic and end-systolic volumes in older patients compared with younger patients.
| Variable | Ages (Years) | p-value | |
|---|---|---|---|
| <75 (n=1037) | ≥ 75 (n=227) | ||
| Age (years) | 61 ± 9 | 79 ± 3 | |
| Women | 327 (32%) | 61 (27%) | 0.17 |
| CRT-D Therapy | 624 (60%) | 133 (59%) | 0.66 |
| Ischemic, NYHA class I | 107 (10%) | 35 (15%) | 0.03 |
| Ischemic, NYHA class II | 305 (29%) | 110 (48%) | <0.001 |
| Non-Ischemic cardiomyopathy, NYHA class II | 625 (60%) | 82 (36%) | <0.001 |
| QRS duration (ms) | 164 ± 19 | 160 ± 18 | 0.02 |
| Hypertension | 640 (62%) | 157 (69%) | 0.03 |
| Diabetes Mellitus | 310 (30%) | 72 (32%) | 0.57 |
| Glomerular filtration rate (ml/min/1.73 m 2 ) | 71 ± 20 | 60 ± 18 | <0.001 |
| Echocardiography | |||
| Left ventricular Ejection Fraction (%) | 23 ± 5 | 24 ± 5 | 0.16 |
| Left ventricular EDV Index (ml/m 2 ) | 127 ± 30 | 122 ± 26 | 0.05 |
| Left ventricular ESV Index (ml/m 2 ) | 91 ± 25 | 87 ± 21 | 0.04 |
| Left Atrial Volume Index (ml/BSA) | 47 ± 10 | 48 ± 10 | 0.30 |
| Medications | |||
| Beta-blockers | 983 (95%) | 204 (90%) | 0.005 |
| ACE Inhibitors/Angiotensin receptor blockers | 1001 (97%) | 214 (94%) | 0.11 |
| Statins | 649(63%) | 154 (68%) | 0.14 |
The cumulative probability of death in young versus older patients is shown in Figure 1 . The rate of death at 2 years in young versus older patients was 4% and 5%, respectively. A separation in the rate of mortality in young and older patients was observed only after 2 years after the device implantation.
In patients receiving an ICD only, the cumulative incidence of VT/VF at 2 years was 9% in older patients versus 22% in younger patients, with a p = 0.006 for the overall difference during follow-up ( Figure 2 ). In those receiving a CRT-D, the cumulative incidence of VT/VF at 2 years was 5% in older patients versus 14% in younger patients, p = 0.008 for the overall difference during follow-up ( Figure 3 ).
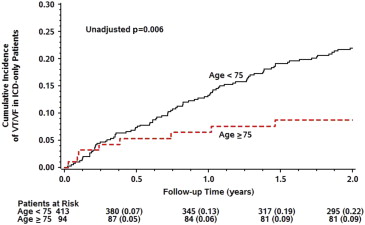
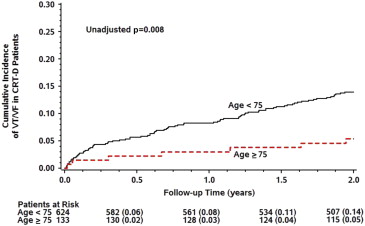
Figure 4 shows the rates of recurrent VTA and death events and the need for appropriate ICD shocks per 100 patient-years of follow-up in the young and older groups. Recurrent VT/VF rates were significantly lower in older compared with younger patients (8.1 events per 100 patient-years vs 22.8 events per 100 patient-years, p <0.001). Recurrent event rates for the end points of VT/VF or SCD, VT alone, VF alone, and the need for appropriate ICD shocks were consistently observed to be lower in older patients compared with younger patients.
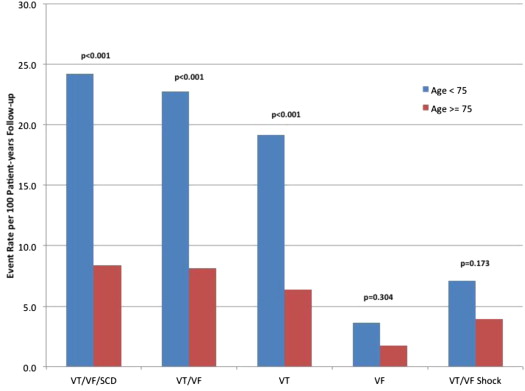
Consistent with these findings, multivariate analysis demonstrated that older patients had a significant 62% lower risk for VT/VF (p <0.001) and 44% lower risk for VT/VF or death, whichever occurred first (p = 0.005) compared with younger patients. Similar risk reductions for the separate end points of VT/VF or SCD, VT alone, and VF alone were seen for older patients compared with younger patients ( Table 2 ). Of note, compared with younger patients, older patients had a 63% lower risk of receiving an appropriate ICD shock, p = 0.014.
| End point | Hazard Ratio | 95 % Confidence Interval | p-value |
|---|---|---|---|
| VT/VF/Death (229 events) | 0.56 | 0.37 – 0.84 | 0.005 |
| VT/VF/Sudden Cardiac Death (193 events) | 0.40 | 0.24 – 0.67 | 0.001 |
| VT/VF (188 events) | 0.38 | 0.22 – 0.64 | <0.001 |
| VT (162 events) | 0.42 | 0.24 – 0.74 | 0.002 |
| VF (44 events) | 0.34 | 0.11 – 1.12 | 0.08 |
| Appropriate Implantable Cardioverter-Defibrillator Shock (88 events) | 0.37 | 0.17 – 0.82 | 0.014 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


