Echocardiography is essential as it plays a crucial role in identifying patients suitable for the procedure, provides intraprocedural guidance, and remains the primary modality for postprocedure followup. The demands on the echocardiographer to interpret and guide catheter-based interventions for SHD are much more complex than interpreting a routine echocardiogram. Consequently, interventional cardiologists—if not well trained—will require the assistance of a skilled echocardiographer as part of the interventional SHD team.
The major advantage of echocardiography over other imaging modalities such as computed tomography (CT) and magnetic resonance imaging (MRI) is its mobility and ease of use. In addition, it does not require any contrast agent, and does not emit ionizing radiations. It can produce real-time 2-D and 3-D images, and has the ability to detect and diagnose complications in real time during the procedure, which helps for early correction and treatment. Transthoracic echocardiography (TTE), transesophageal echocardiography (TEE), and intracardiac echocardiography (ICE) are the three modalities widely used for SHD interventions. The advantages and limitations of each are listed in
Table 38-1.
Transthoracic Echocardiography
TTE is noninvasive and widely available. It does not require patient sedation or general anesthesia. Newer systems are small and portable and provide adequate 2-D imaging and Doppler capabilities to assist in a number of procedures, including mitral balloon valvuloplasty, alcohol septal ablation, atrial septostomy, and others (
2). TTE images may be challenging to acquire with the patient supine on the catheterization table, and usually the probe and the operators’ arm may be in the fluoroscopic field, and thus simultaneous images may not be obtainable (
3).
Transesophageal Echocardiography
Currently TEE is the standard imaging technique in many centers that perform catheter-based interventions (
3). TEE offers superior imaging quality when compared with TTE. It provides direct assessment of intraprocedural anatomy and physiology, shows the relationship between catheters/devices and cardiac structures, and helps guide interventions and diagnose complications. TEE imaging does not interfere with the operative field and rarely interferes with the fluoroscopic field. One of the most important limitations of TEE includes the need for deep sedation or general anesthesia with endotracheal intubation. In addition, long cases may predispose the TEE probe to overheat, causing burns in the esophagus (
2).
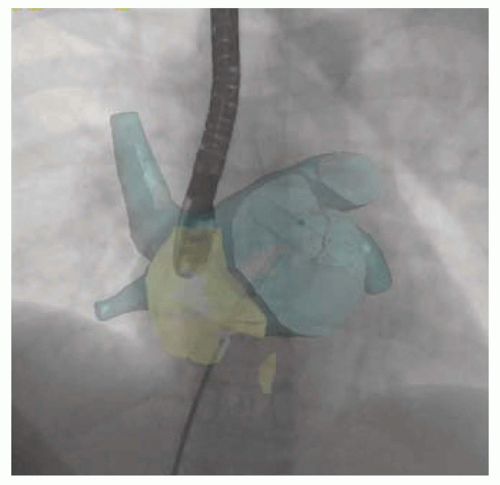
On the other hand, TEE has the capability to provide
real-time 3-D imaging. This capability has overcome the limitations of other 3-D imaging modalities such as CT and MRI that have to acquire images prior to the procedure and process them offline to obtain 3-D reconstructions. Real-time 3-D TEE (RT 3D TEE) can provide immediate and online images of cardiac structures, including mobile structures; superior spatial relationship; and alignment of catheters and devices to the cardiac defects. These defects often have a complex morphology that is suboptimally visualized by 2-D imaging, including TEE (
4). In addition, 3-D TEE provides
en face views of cardiac structures, valves, and surrounding tissues,
which has proved to be of great value in some procedures such as repair of paravalvular leaks (
5). RT 3D TEE has a steep learning curve and requires effective communication between the echocardiographer and the interventionalist (
1).
Intracardiac Echocardiography
ICE has demonstrated an excellent potential to guide and monitor catheter-based interventions. The image quality of ICE is comparable or at times superior to TEE. This technology is widely used for a broad variety of SHD and electrophysiological procedures. Even though ICE is an invasive procedure, one of its major advantages is the elimination of the need for general anesthesia and endotracheal intubation as in TEE (
2).
The most commonly used ICE catheters come in 8- and 10-F shafts with a transducer frequency that ranges from about 5 to 10 MHz and has Doppler and color flow capabilities. The catheter is attached to a control handle that helps steer it in four different directions (anterior-posterior and left-right) using two different knobs. The third knob locks the position of the catheter in place once the desired image is displayed (
6). The probe is advanced through a separate sheath in the ipsilateral or contralateral femoral vein into the right atrium. Generally, a long sheath from the femoral vein is advanced into the inferior vena cava, and then the ICE catheter is advanced under fluoroscopic guidance because of its rigidity and its blunt tip that may get wedged in venous branches, causing potential injury to vital organs and bleeding (
7). When the catheter reaches the right atrium, the standard starting view, called the “home view,” shows the right atrium, right ventricle, tricuspid valve, anterior part of the anterior septum, and the right ventricular inflow and outflow tracks. Depending on the procedure being performed, the ICE catheter can be navigated and its position adjusted to give standardized views that help guide interventions on the atrial septum, ventricular septum, mitral valve, pulmonic valve, LAA, and even the descending aorta.
There is a substantial learning curve associated with the use of ICE. This is mainly related to the understanding of the unique images obtained by ICE compared with the standard echocardiographic images. However, studies have shown that with the repeated use of ICE, the operator becomes significantly less dependent on fluoroscopy to identify cardiac structures, guide interventions, and diagnose complications (
4). This reduction in fluoroscopy time is a potential benefit for both patients and high-volume operator. Other advantages of ICE include minimal additional staff requirement and no additional space for the echocardiography and anesthesia teams, and the fact that the patient can be awake for interaction during the procedure. Some of the disadvantages of this imaging modality include the additional cost of the single-use catheter, invasive nature of the procedure, and unavailability of commercial 3-D imaging capability yet. Complications associated with ICE use are mainly caused by its invasive nature and the need for maneuvering and manipulation of the stiff catheter in vascular and cardiac structures, and they can occur in 1% to 3% of cases (
Table 38-2). Reported complications include, but are not limited to, vascular access site complications, venous and cardiac perforation, arrhythmias, thromboembolism, and cutaneous nerve palsy (
8).