Fig. 8.1
Depiction of auscultation findings for HCM
Test Results
Echo.
Echocardiogram (Fig. 8.2) shows an enlarged interventricular septum and LVOT obstruction during systole (arrow) in a patient with HCM. Asymmetrical LV hypertrophy is noted with septal thickening.

Fig. 8.2
Echocardiogram showing the increased septal thickness and systolic anterior motion of the mitral leaflet into the left ventricular outflow tract
Doppler.
Doppler ultrasound (Fig. 8.3) shows increased blood ejection velocity from the LV. There is a presence of late-peaking systolic velocity due to the LVOT obstruction.
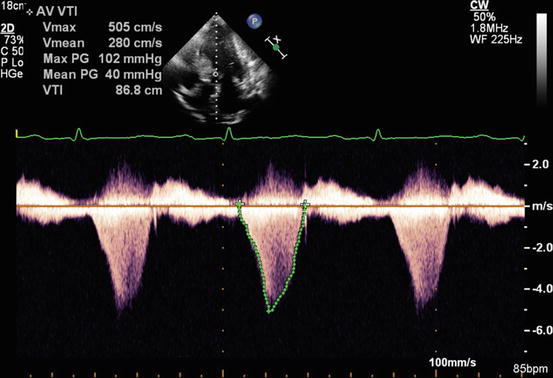
Fig. 8.3
Doppler ultrasound showing severely increased left ventricular outflow velocity due to dynamic obstruction of the outflow tract
Subaortic velocity acceleration is noted by turbulence of blood flow.
LVOT peak velocity of 4–6 m/s.
Systolic anterior motion of the anterior mitral valve leaflet.
Grade 2 aortic regurgitation.
Clinical Basics
Normal Anatomy
HCM pathophysiology arises from obstruction of aortic valve/outflow tract due to excessive cardiac muscle build up.
50–75 % have subaortic stenosis from ventricular septum obstruction.
left ventricular outflow tract plaque (scarring from anterior mitral valve leaflet rubbing against the outflow tract).
There is reduced left ventricular compliance in conjunction with left atrial dilation.
Myocardial abnormalities include cardiomegaly, enlarged asymmetric ventricular septum, and asymmetric LV thickness, with the interventricular septum being hypertrophied more so than the left ventricle free wall (Fig. 8.4).
Fig. 8.4
Illustration of the myocardial abnormalities in hypertrophic cardiomyopathy, including cardiomegaly with an asymmetrically thickened interventricular septum
On histology, there is cardiac myofiber disarray and thickened intramural coronary arteries.
Etiology
50 % hereditary.
Family member with exertional syncope or sudden death.
Most common familial heart disease.
Sarcomere protein abnormality (usually beta-myosin heavy chain).
Male predominance.
1 % of all congenital heart disease.
Often associated with other congenital heart diseases.
Potential hemodynamic cause.
(a)
Steeper aorto-ventricular angle with increased aortic override.
Four morphological variants.
Thin discrete membrane.
Fibromuscular ridge at base of intraventricular septum.
Ring of tissue attached to LV outflow tract and base of mitral valve.
Fibromuscular tunnel in LV outflow tract.
Types 1 and 2 account for 75 % of cases.
Signs and Symptoms
Often related to exertion.
Shortness of breath or dyspnea (most common symptom) especially in the setting of atrial fibrillation.
Dizziness or syncope.
Angina.
Arrhythmias common.
Sudden death (often exercise related) usually with very high LVOT gradients.
Rapid or quick-rise (“flip”) pulse.
Prevalence
The prevalence of HCM is 20/100,000.
Typical age of onset is 20–50 years old.
The disease occurs with a male predominance (1.5:1).
Key Auscultation Features
Systolic murmur.
Occurs in early to mid systole with a peak around mid systole.
Best heard at the apex and left sternal border (aortic area).
May not radiate.
Has a crescendo-decrescendo pattern (Fig. 8.1).
Low pitched, murmur intensity grade 2–4/6.
The murmur of HCM is highly dependent on the volume of blood in the LV.
With less blood, the LV outflow tract can be increasingly obstructed because the septum and the mitral valve become closer together, thus the murmur gets louder.
Conversely, increased venous return will increase volume in the LV and decrease the murmur intensity.
Normal S1.
S2- often single due to prolonged LV systole.
No ejection click.
Changes with maneuvers [1]:
In a majority of cases (90 % of the time), the murmur intensity will decrease on inspiration and increase on expiration.
Increase in intensity with Valsalva maneuver (65 % sensitivity, 96 % specificity).
Increase in intensity from squatting to standing (95 % sensitivity, 84 % specificity).
Decrease in intensity with passive leg elevation (85 % sensitivity, 91 % specificity).
Decrease in intensity with handgrip maneuver after 1 min of maximal contraction (85 % sensitivity, 75 % specificity).
Valsalva maneuver and standing increase murmur intensity; handgrip maneuver, passive elevation of the lower extremity, and squatting each decrease the murmur intensity (Fig. 8.5).
Fig. 8.5
Maneuvers to accentuate or diminish the intensity of the systolic murmur heard in patients with HCM< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


