Hydatid Disease of the Lung
Nickolaos N. Harlaftis
Homeros A. Aletras
Panagiotis N. Symbas
Hydatid disease has been known since ancient times. Hippocrates referred to it and Rudolphi40 first used the term hydatid cyst to describe echinococcosis in humans.
Echinococcosis remains a significant health problem in endemic areas, including the Middle East and Mediterranean countries, South America, Australia, New Zealand, Central Asia, China, Alaska, and East Africa as well as among Indian tribes of Canada. Although the disease has been rare in North America and western Europe, a greater frequency of this clinical entity can be expected with increases in travel and migration. Therefore the possibility of hydatid disease should be considered in a patient who has lived or traveled in an endemic area and presents with a well-defined spherical density of the lung.
Pathophysiology
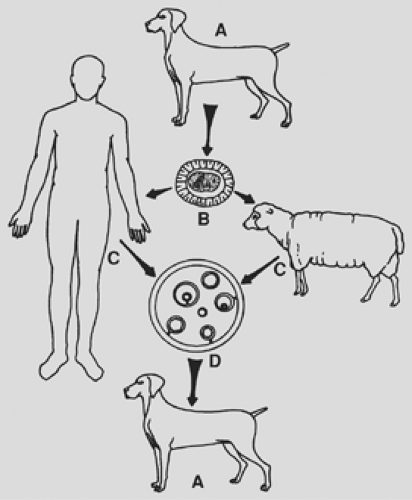
Hydatid disease is caused by Echinococcus granulosus. Its primary hosts are the members of the Canidae family, usually dogs, wolves, and coyotes. They contract echinococcosis by ingesting mature, productive echinococcal cysts in the viscera of an intermediate host (e.g., sheep, goats, cattle, hogs, moose, reindeer, deer, elk, etc.).
In the intestines of the primary host, the hydatid cyst develops into a parasitic worm containing 400 to 800 ova. These are released in the feces of the primary host and then introduced into intermediate hosts by ingestion of contaminated grass, water, vegetables, and such. The larval stage begins in the intermediate host and leads to the development of hepatic and pulmonary hydatid cysts.
In the gastrointestinal tract of the intermediate host, including humans, the ovum develops into an embryo, which, with the aid of its hooklets, attaches to and penetrates the mucosa of the duodenum and jejunum, enters the mesenteric venules, and proceeds to the portal vein and the liver, where it becomes embedded.48 Those embryos whose diameter does not exceed 0.3 mm may pass through the sinus capillaries of the liver and, by way of the hepatic veins and vena cava, proceed to the right side of the heart and the pulmonary capillaries, where they may become embedded.
One alternative pathway of the parasites’ entrance into the lung is the lymphatic circulation. The embryo enters the lymphatics of the small intestine, proceeds to the thoracic duct, to the central venous system, to the right side of the heart, and then to the lungs. Another possible route is a venovenous anastomosis in the liver and the space of Retzius. The infected liver and the lungs are then ingested by the primary host, and thus the cycle continues (Fig. 94-1).
The liver is most commonly infected with hydatid disease (60% to 80% of all cases), followed by the lung in 10% to 30% of the patients Morar and Feldman (2003). Pulmonary echinococcosis most frequently occurs in the right and both lower lobes, as has been noted in the series of Aletras,1 Dogan,19 Burgos,11 and Dakak14 and their associates. The studies of Dogan19 and Solak49 and their colleagues have demonstrated that 75% to 90% of these cysts are solitary, whereas involvement of both lungs occurs in 2% to 30%.
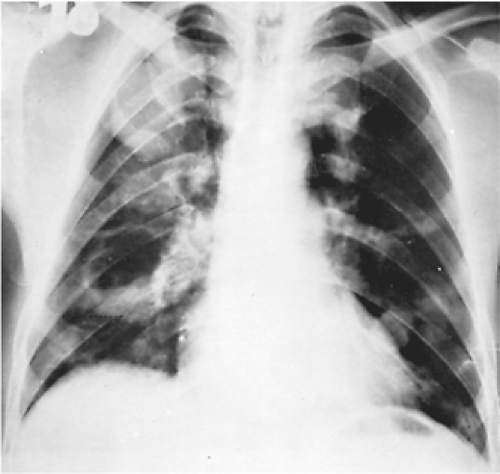
Each cyst grows and matures independently of any coexisting cyst (Fig. 94-2). Balci and associates6 emphasized that children are more likely to develop pulmonary rather than hepatic echinococcal cysts.
Some evidence suggests that echinococcal cysts develop more rapidly in the lungs of children than those of adults, which may explain the more common appearance of pulmonary cysts in children. Younger patients have larger cysts owing to their greater tissue elasticity. Large pulmonary hydatid cysts are critical because they pose a higher risk of rupture. Sometimes the entire hemithorax of a young child is occupied by parasitic cysts (Fig. 94-3).
Two types of pulmonary hydatid cysts occur in humans: the unilocular and the alveolar. This discussion is limited to the unilocular variety, because these are the cysts of clinical importance. A hydatid cyst is composed of the wall and the hydatid fluid. There are three layers in the wall of the cyst. Two of these, the outer laminated membrane and the inner germinal layer or germinative membrane, derive from the parasite, and one layer, the pericyst or adventitia, is produced by the host. The adventitia, also known as the ectocyst, is rarely thicker than a few millimeters—it is a capsule composed entirely of the host cell’s fibrous matter, connective tissue, and compressed parenchymal cells resulting from the inflammatory response of the organ. Functionally, this layer provides mechanical protection and nutrition to the parasite. Therefore, whenever degenerative changes of the membrane develop, such as calcification, an amorphous degeneration automatic absorption of the hydatid cyst occurs. The laminated membrane, 1 to 3 mm thick, is composed of hyaline and elastic tissue with no host blood vessels; it is easily discernible from the pericystic layer, which is vitally important to the surgeon. Schwabe44 and Larbaoui29
noted that it is permeable to calcium, potassium, chlorides, water, and colloids. Larbaoui29 emphasized that when this layer is intact, it constitutes a perfect filter for microorganisms while allowing the entrance of colloids and crystalloids. Nutritional and other substances useful to the parasite traverse the membrane by diffusion, but active transport may also play a role.
noted that it is permeable to calcium, potassium, chlorides, water, and colloids. Larbaoui29 emphasized that when this layer is intact, it constitutes a perfect filter for microorganisms while allowing the entrance of colloids and crystalloids. Nutritional and other substances useful to the parasite traverse the membrane by diffusion, but active transport may also play a role.
The germinal layer (germinative membrane, or endocyst) is the inner layer of the cyst wall. It is a thin, transparent, granular membrane lined with small papillae, which are brood capsules at different stages of development. These capsules, which are formed by the proliferation of the cells of the germinal layer, develop buds of scolices, which have suckers and hooks and represent the mature parasite larvae. The germinative membrane is the living part of the parasite; it produces the laminated membrane and reproduces the parasite. Some cysts cannot regenerate, but every undamaged cyst regardless of size must be considered capable of reproduction.
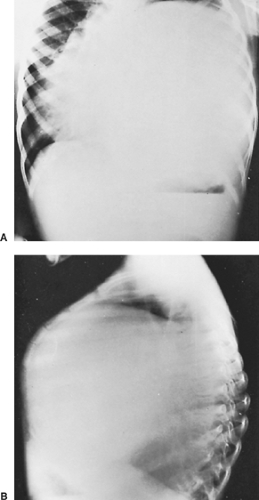 Figure 94-3. Frontal (A) and lateral (B) preoperative and postoperative chest radiographs of a 5-year-old boy with a giant left-lower-lobe hydatid cyst producing chest deformity. |
The hydatid cyst is filled with hydatid fluid, which is colorless, odorless, and sterile, resembling crystal-clear water. Yuksel and colleagues55 contend that the pressure of the fluid ranges from 21 to 61 cm H2O. It contains antigenic elements that may cause anaphylactic phenomena when the cyst ruptures.
The cysts grow more rapidly in the lungs than in other organs, mainly because of the negative pressure and the great elasticity of the pulmonary tissue. In the course of their natural evolution,
many cysts gradually cease growing and degenerate. During the growth period of the cyst, it may rupture spontaneously or during coughing, sneezing, or any other cause of increased intrathoracic pressure, or after injury during diagnostic thoracentesis. Large cysts are especially vulnerable to rupture because of the increased pressure exerted by the fluid. The rupture may occur within the boundaries of the pericystic layer, into the pleural space, or into a neighboring organ, bronchus, or blood vessel. Rupture of the germinal membrane toward the interior of the cyst may result in the formation of daughter cysts. Such formation after a rupture of the laminated membrane is rare. Rupture of the cyst toward the surrounding tissues may be followed by secondary echinococcosis, and rupture into a blood vessel may lead to embolization of a portion of the cyst. Rupture of the cyst and evacuation of the cystic content into a main bronchus rarely results in spontaneous cure. This complication exposes the patient to asphyxia, anaphylactic shock, secondary hydatid spread as well as hemoptysis, according to Ramos and colleagues.39 Suppuration of the cyst can occur after rupture and secondary infection. Intrapleural rupture is limited by the development of pleural adhesions. The consequences of intrapleural rupture are triggering of an anaphylactic reaction, infection of the cyst, or secondary pleural hydatidosis. However, according to Ramos and colleagues,39 the frequency of secondary pleural hydatidosis is low. Calcification of the cyst in the lung is rare. It resembles an eggshell, is limited in the adventitia of complicated cysts, and does not always indicate that the hydatid is dead. A calcified lung cyst is almost always in communication with the bronchial tree and is probably infected.
many cysts gradually cease growing and degenerate. During the growth period of the cyst, it may rupture spontaneously or during coughing, sneezing, or any other cause of increased intrathoracic pressure, or after injury during diagnostic thoracentesis. Large cysts are especially vulnerable to rupture because of the increased pressure exerted by the fluid. The rupture may occur within the boundaries of the pericystic layer, into the pleural space, or into a neighboring organ, bronchus, or blood vessel. Rupture of the germinal membrane toward the interior of the cyst may result in the formation of daughter cysts. Such formation after a rupture of the laminated membrane is rare. Rupture of the cyst toward the surrounding tissues may be followed by secondary echinococcosis, and rupture into a blood vessel may lead to embolization of a portion of the cyst. Rupture of the cyst and evacuation of the cystic content into a main bronchus rarely results in spontaneous cure. This complication exposes the patient to asphyxia, anaphylactic shock, secondary hydatid spread as well as hemoptysis, according to Ramos and colleagues.39 Suppuration of the cyst can occur after rupture and secondary infection. Intrapleural rupture is limited by the development of pleural adhesions. The consequences of intrapleural rupture are triggering of an anaphylactic reaction, infection of the cyst, or secondary pleural hydatidosis. However, according to Ramos and colleagues,39 the frequency of secondary pleural hydatidosis is low. Calcification of the cyst in the lung is rare. It resembles an eggshell, is limited in the adventitia of complicated cysts, and does not always indicate that the hydatid is dead. A calcified lung cyst is almost always in communication with the bronchial tree and is probably infected.
Clinical Manifestations
The clinical presentation of hydatid cysts of the lung depends on whether the cysts are intact or ruptured. Intact or simple cysts of the lung produce no characteristic symptoms. Their clinical manifestations depend on their site and size. Small, peripherally located cysts may manifest with symptoms of compression of adjacent organs. If the patient is symptomatic, the first complaint is often a nonproductive cough; some patients, particularly those with centrally located cysts, may have blood-streaked sputum, although massive hemoptysis does not occur. Some patients complain of a dull or acute chest pain or present with a sensation of pressure in the chest with no aggravating or relieving features. During infancy, the hydatid cyst may disturb growth. In children who have a supple chest wall, a bulge in the ipsilateral chest may also be observed (see Fig. 94-3).
Rupture of the cyst may occur spontaneously or as a result of trauma or anthelminthic therapy. In the case of a contained rupture, only the endocyst is torn and the contents of the cyst are contained by the pericyst.
Rupture of the cyst into an adjacent bronchus may be manifested by vigorous coughing and expectoration of salty sputum consisting of mucous hydatid fluid and occasionally fragments of the laminated membrane, generally described as “grape skin” or frothy blood. In addition, the patient may develop a severe hypersensitivity reaction, manifested by generalized rash, high fever, pulmonary congestion, and severe bronchospasm. Occasionally the intrabronchial rupture of the cyst manifests with sudden and severe dyspnea, which may lead to suffocation and death from complete tracheal obstruction by fragments from the hydatid membrane. The diagnosis of rupture of the hydatid cyst is unequivocally made when the hooklets or the parasites are found during microscopic examination of the sputum. Complete intrabronchial evacuation of the hydatid contents may result in cure of the disease in few patients. More often the parasitic membrane and a significant quantity of parasitic fluid remain in the pericystic cavity and the patient experiences complications from local infection. In this case the most usual manifestations are fever, chronic cough, mucopurulent or dark bloody sputum, anorexia, and weight loss.
Rupture of the cyst into the pleural cavity is a severe but infrequent complication. It occurred in 5% of the patients of Ramos and colleagues.39 The symptoms are usually insidious and moderate; they consist of dry cough, chest pain, moderate dyspnea, generalized malaise, and fever. These relatively mild clinical manifestations result from preexisting pleural adhesions, which prevent the dissemination of the cyst’s contents into the whole pleural space. In some patients, particularly those without preexisting pleural adhesions, intrapleural rupture of the cyst produces an acute and dramatic clinical picture consisting of intense chest pain, persistent cough, severe dyspnea, and even cyanosis, shock, and suffocation. Frequently symptoms of generalized urticaria, intense pruritus, and severe anaphylactic shock can occur, even leading to death.
The symptoms of intrapleural rupture of a hydatid cyst are accompanied by the physical findings of localized or generalized hydropneumothorax.
Diagnosis
Diagnosis of an intact echinococcal cyst is usually based on suspicion resulting from an unexpected finding on routine chest radiographs. Radiographically, the cyst appears as a homogeneous spherical opacity with definite edges (Fig. 94-4). Sharma and Eggleston47 emphasized that a change from a spherical to an oval shape may be observed only during deep inhalation
(Escudero–Nemerow sign). The radiologic picture depends mainly on the size and location of the cyst. A small cyst may appear as a small vesicle and is difficult to recognize until it grows large enough to present a clear image on the chest radiograph. A cyst may cause distal bronchial obstruction, manifested as atelectasis and pneumonitis beyond the cyst. Centrally located cysts may compress the bronchovascular structures, presenting radiographically as a depression or indentation at the site of pressure, the so-called notch sign. The cyst may also have a clear crescentic shadow on the top or on one side, referred to as a pneumocyst by Dévé,17 perivesicular pneuma by Arce,3 perivesicular meniscus by Peschiera,36 moon sign or crescent sign by Barret and Thomas,8 and pulmonary meniscus sign by Saidi.41 This sign has been attributed to the air that enters the perivesicular space, becoming trapped between the adventitia and the unruptured vesicle after vigorous coughing, straining, or direct trauma to the cyst, and is the first radiographic sign of impending rupture. A double-domed arch sign may appear when a small additional amount of air enters the hydatid vesicle. The entrance of free air into the cyst and the perivesicular space after complete rupture of the laminated membrane displaces the fluid. This finding has been termed a camalote sign by Arce3 and a water lily sign by Lagos-Garcia and Segers.28 It is produced by the floating membrane of the cyst (Fig. 94-5). However, these three diagnostic signs are radiographic rarities.9 Most cysts present as a solid mass in the right lower lobe. They are solitary lesions in approximately 60% of cases and multiple unilateral or bilateral lesions in 20% to 50% of cases as described by Martinez31 and Kuzucu26 and their colleagues and are indistinguishable from other pulmonary lesions.
(Escudero–Nemerow sign). The radiologic picture depends mainly on the size and location of the cyst. A small cyst may appear as a small vesicle and is difficult to recognize until it grows large enough to present a clear image on the chest radiograph. A cyst may cause distal bronchial obstruction, manifested as atelectasis and pneumonitis beyond the cyst. Centrally located cysts may compress the bronchovascular structures, presenting radiographically as a depression or indentation at the site of pressure, the so-called notch sign. The cyst may also have a clear crescentic shadow on the top or on one side, referred to as a pneumocyst by Dévé,17 perivesicular pneuma by Arce,3 perivesicular meniscus by Peschiera,36 moon sign or crescent sign by Barret and Thomas,8 and pulmonary meniscus sign by Saidi.41 This sign has been attributed to the air that enters the perivesicular space, becoming trapped between the adventitia and the unruptured vesicle after vigorous coughing, straining, or direct trauma to the cyst, and is the first radiographic sign of impending rupture. A double-domed arch sign may appear when a small additional amount of air enters the hydatid vesicle. The entrance of free air into the cyst and the perivesicular space after complete rupture of the laminated membrane displaces the fluid. This finding has been termed a camalote sign by Arce3 and a water lily sign by Lagos-Garcia and Segers.28 It is produced by the floating membrane of the cyst (Fig. 94-5). However, these three diagnostic signs are radiographic rarities.9 Most cysts present as a solid mass in the right lower lobe. They are solitary lesions in approximately 60% of cases and multiple unilateral or bilateral lesions in 20% to 50% of cases as described by Martinez31 and Kuzucu26 and their colleagues and are indistinguishable from other pulmonary lesions.
 Figure 94-4. Routine frontal chest radiograph showing a small peripheral hydatid cyst in the left upper lung field. |
Therefore every discrete radiologic lesion observed in any patient over 3 years of age in an endemic area should be considered a hydatid cyst. Also, a patient with lung hydatidosis should be investigated for associated liver cysts. The radiographic pleural manifestations in the acute stage of rupture of a cyst vary from loculated hydropneumothorax to nonloculated partial, complete, or tension hydropneumothorax. The water lily sign can also be observed in instances of rupture of the cyst into the pleura (Fig. 94-6). A nodular extrapulmonary appearance suggests secondary hydatidosis of the pleura. As Dogan and colleagues19 have noted, the usual radiographic signs after rupture of a cyst into the bronchi are an air meniscus, the water lily sign, and incarcerated membrane.
 Figure 94-5. Frontal chest radiograph of a ruptured echinococcal cyst in the right lower lung field, with the cystic membrane floating on the hydatid fluid (arrow)—the water lily sign. |
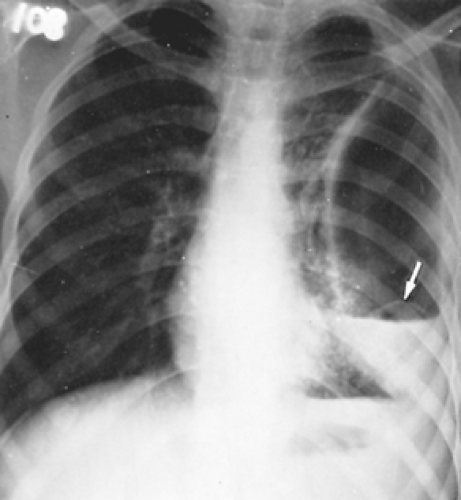 Figure 94-6. Frontal chest radiograph showing a collapsed echinococcal membrane lying above the air–fluid level (arrow)—the water lily sign—in a 15-year-old boy admitted with a pyothorax. |
Computed tomography (CT), as Saksouk and associates43 have reported, has added to the diagnosis of hydatid disease of the lung, particularly to the early discovery of coexistent small cysts in the lung and of pending or existing rupture of the cyst.
CT scanning with contrast may demonstrate a thin enhancing rim if the cyst is intact. The contents of these cysts are homogeneous, with a density similar to that of water.
Also, as Kalovidouris and colleagues22 have noted, CT scanning appears to be valuable in the follow-up of patients who have had resection or evacuation of a hydatid cyst of the lung.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree