Recurrent presyncope is occasionally reported by patients with hypertrophic cardiomyopathy (HC). However, it is difficult to identify on 24-hour Holter recordings the mechanisms responsible for these infrequent symptoms. We report the case of a patient with HC with recurrent presyncope and without major sudden death risk factors, in whom electrocardiographic loop recording identified life-threatening arrhythmias as the mechanism responsible for these symptoms. Documentation of these arrhythmias justified implantation of a cardioverter-defibrillator in the absence of other risk factors.
Some patients with hypertrophic cardiomyopathy (HC) report sporadic episodes of dizziness and lightheadedness, occasionally associated with palpitations. However, the mechanisms responsible for these potentially worrisome symptoms are difficult to document on 24-hour Holter electrocardiographic (ECG) monitoring. In the case we report, ECG loop recording identified life-threatening arrhythmias as the cause of recurrent episodes of dizziness associated with lightheadedness in a patient with HC without major risk factors. Documentation of these arrhythmias justified aggressive management and the implantation of an implantable cardioverter-defibrillator (ICD) for primary prevention of sudden death.
Case Description
In February 2010, a 68-year-old man with HC presented with recent episodes of dizziness associated with lightheadedness and occasional palpitations, the latter being described as a sensation of “skipped beats.” During the 2 previous weeks, such symptoms had occurred 4 times at rest. The patient had no history of premature sudden death in the family. He had mild symptoms of heart failure (New York Heart Association class II) and no history of syncope or angina. Electrocardiography showed sinus rhythm and left ventricular (LV) hypertrophy with deep negative T waves in leads V 3 to V 6 . Echocardiography demonstrated asymmetric LV hypertrophy, with a maximal LV wall thickness of 18 mm at the level of the anterior interventricular septum, a mildly enlarged left atrium (diameter 43 mm, area 22 cm 2 ), and a 12 mm Hg LV outflow peak gradient under basal conditions. Cardiac magnetic resonance confirmed the magnitude of LV hypertrophy and showed a small and poorly demarcated area of late gadolinium enhancement at the level of the anterior interventricular septum. A 24-hour Holter ECG recording identified a single run of 4 beats of nonsustained ventricular tachycardia with a rate of 140 beats/min. During Holter monitoring, the patient remained free of symptoms.
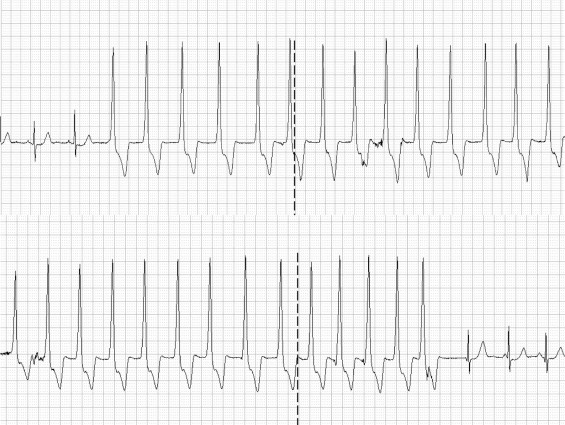
In an attempt to identify the mechanisms responsible for these recent episodes of dizziness and lightheadedness, an external ECG loop recorder was used, which could be activated by the patient at the time of symptoms. The memory of this device stores the ECG tracings recorded during the 5 minutes before and after its activation. During the subsequent 13 days, the patient activated the event recorder 4 times, immediately after the occurrence of dizziness and palpitations, and the ECG tracings documented 4 alarming episodes of nonsustained ventricular tachycardia ( Figures 1 to 3 ). The potential prognostic implications of these tachyarrhythmias, as well as the limitations of risk stratification for sudden death in HC, were discussed with the patient, and the mutual decision was reached to implant an ICD. Shortly thereafter, while awaiting hospital admission for ICD implantation, the patient experienced an episode of prolonged palpitations associated with a loss of postural tone.