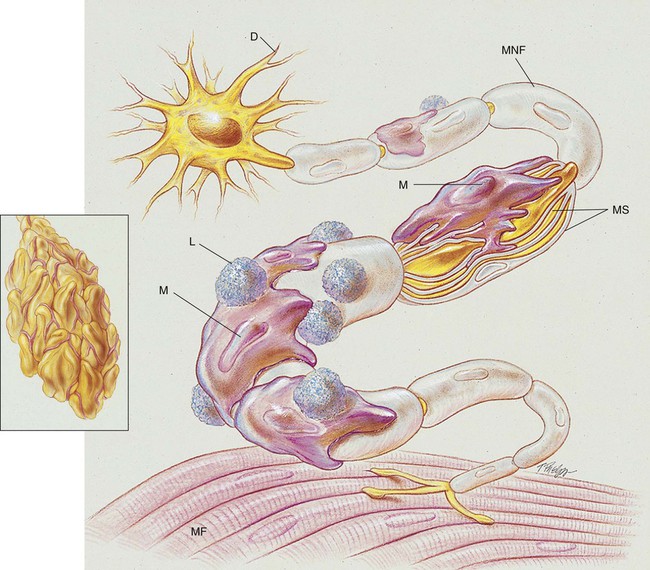
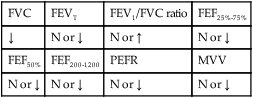
After reading this chapter, you will be able to: • List the anatomic alterations of the lungs associated with Guillain-Barré syndrome. • Describe the causes of Guillain-Barré syndrome. • List the cardiopulmonary clinical manifestations associated with Guillain-Barré syndrome. • Describe the general management of Guillain-Barré syndrome. • Describe the clinical strategies and rationales of the SOAPs presented in the case study. • Define key terms and complete self-assessment questions at the end of the chapter and on Evolve. Paralysis of the skeletal muscles develops in response to various pathologic changes in the peripheral nerves. Microscopically, the nerves show demyelination, inflammation, and edema. As the anatomic alterations of the peripheral nerves intensify, the ability of the neurons to transmit impulses to the muscles decreases, and eventually paralysis ensues (see Figure 28-1). Box 28-1 lists other names in the literature for Guillain-Barré syndrome. The precise cause of Guillain-Barré syndrome is not known. It is probably an immune disorder that causes inflammation and deterioration of the patient’s peripheral nervous system. Elevated levels of immunoglobulin M (IgM) antibodies against myelin glycolipid have been found in the serum of patients with Guillain-Barré syndrome. Antibodies that are cell-mediated are thought to be responsible for peripheral nerve demyelination and inflammation. Lymphocytes and macrophages appear to attack and strip off the myelin sheath of the peripheral nerves and leave swelling and fragmentation of the neural axon (see Figure 28-1). It is believed that the myelin sheath covering the peripheral nerves (or the myelin-producing Schwann cell) is the actual target of the immune attack.
Guillain-Barré Syndrome
Anatomic Alterations of the Lungs Associated with Guillain-Barré Syndrome
Etiology and Epidemiology