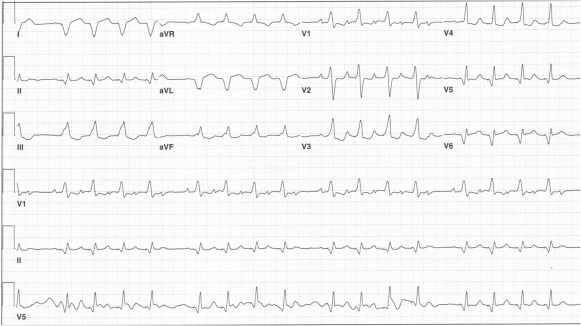
A 79-year-old woman with severe aortic stenosis, a history of atrial fibrillation and sick sinus syndrome, and implantation of a biventricular DDD pacemaker 3 years earlier presented to the hospital with congestive heart failure. Her electrocardiogram on admission showed what looked like sinus tachycardia at a rate of 127 beats per minute ( Figure 1 ). No atrial pacemaker spikes were seen. Groups of 4 QRSs, with each complex initiated by a pacemaker spike, were separated by pauses. The cause of this group beating was the intrinsic atrial rate’s having exceeded the maximum tracking rate of the pacemaker, which was set at 120 beats/min. The normal pacemaker response to this was progressive lengthening of the PR intervals to keep the conducted QRS complexes at the upper tracking rate of 120. The PR lengthening and the consequent shortening of the RP intervals eventually resulted in a P wave falling into the postventricular atrial refractory period, not being sensed, and therefore not followed by a ventricular stimulus, that is, pacemaker Wenckebach mimicking intrinsic second degree atrioventricular block, type I. Like most DDD pacemakers, the patient’s device had an automatic mode switching algorithm, but it would only have been activated if the patient’s atrial rate had reached 180 beats/min.