Advantages
Disadvantages
Not influenced by weather
Shorter maximum distance coverage
Available night and day
Safety of transportation negatively affected by street roughness, other vehicles, traffic
Airports/heliport and secondary transportation not required
Slower
No need for a flight-trained medical emergency team
More units available at the same time
Table 39.2
ECMO transportation ambulance technical requirements
Requirement | Reason |
|---|---|
Adequate space (enlarged) | |
Reinforced ambulance stretcher and stretcher holders | To support increased weight (ECMO pump, ECMO heater, ICU ventilator) |
Reinforced shock adsorbers | To mitigate the effect of street roughness on the devices employed (especially ECMO pump) |
Increased compressed oxygen storage | To support both ventilator MV and ECMO oxygenator sweep gas at iFO2 100 % |
Increased battery capacity | To support air heater/cooler, ICU ventilator, ICU monitor, infusional pumps, ECMO pump, ECMO heater |
Increased fuel tanks | To avoid the need for fuel supplying during transportation |
39.3 Equipment
Custom-made mobile steel carts or cradles have been developed by each ECMO centre to easily load all the equipment on the patient and to allow safe loading/unloading on the ambulance. Our custom-made steel cart (Fig. 39.1) extends in height (100 cm) and provides two supports on two levels. It mounts on the spinal board over the patient’s feet and allows transportation of the ECMO unit (driving pump, heater and console), an ICU ventilator and an ICU monitor. Moreover, a especially designed iron post allows holding of infusional pumps, pressure bags and fluids. A power strip is fixed on a post to organize electrical cables. Patient-cart unit is then secured and loaded on ambulance stretcher (maximum tolerance 250 kg). When loaded on the ambulance (Fig. 39.2), it may be secured with additional ropes to avoid rolling of the patient-cart unit and displacement of the equipment.
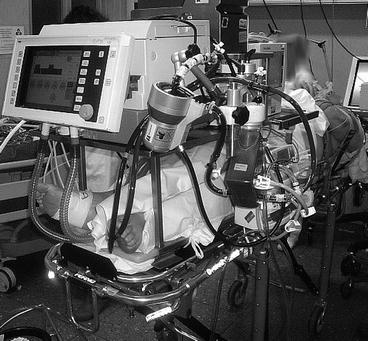

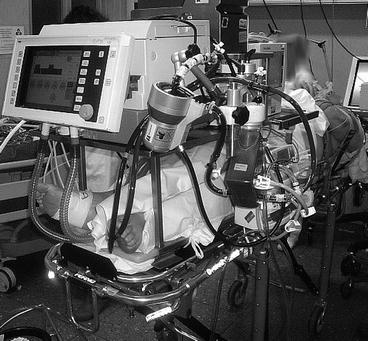
Fig. 39.1
ECMO transportation custom-made steel cart at the end of patient preparation. Special attention should be paid to weight distribution on the stretcher

Fig. 39.2
Patient-cart unit loaded on the special ICU unit and secured. Of note, up to three ECMO team members can sit on the right of the patient during transport (ECMO pump, ventilator and monitoring), while other two members can sit at the head of the patient (drug infusions and artificial airway management)
All the equipment needed for cannulation, priming of ECMO circuit and emergency procedures are listed in checklists and organized into backpacks. Backpacks and electrical equipment must be checked before departure, and materials must be replaced immediately after use.
39.4 Pre-transport Preparation
On arrival the ECMO team gets clinical informations from the referring medical staff and takes charge of the patient. It’s important to avoid unnecessary delays of referral; the ECMO team will attempt to get the most stable clinical condition after ECMO is started and the patient is positioned supine on the stretcher. The cart will be placed on the stretcher and carefully loaded with special attention to weight-balance the cart. All the equipment will be checked again while on battery energy supply and tightly secured. Only after these procedures the patient will be moved to the ambulance. Moving the patient to the ambulance, oxygen to both the ECMO membrane lung and the ventilator will be provided by at least two small oxygen tanks. Power and gas supplies will be replaced by ambulance power inverter and gas tanks once loaded.
39.5 Team
The ECMO team is multidisciplinary and should be staffed by experienced and trained personnel. The team must be able to apply and run ECMO via peripheral venous-venous or venous-arterial cannulation and to front serious adverse events (see below). The number and composition of the group may vary from a minimum of three [5, 17] up to 15 [7, 10, 18], depending on the distance of the referring hospital (i.e. need for two drivers, support vehicles) and the presence of trainees, logistics and local practices. More frequently, the team includes at least a perfusionist to provide ECMO circuit set-up and management, two ECMO skilled physicians (surgeons and/or critical care physicians or both), one or two critical care nurses and drivers. Although Seldinger cannulation technique is preferable, many groups include a cardiac surgeon in order to provide, when needed, direct vascular cutdown or rescue thoracotomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


