General Features of Pulmonary Resections
Gaetano Rocco
Thomas W. Shields
Resections of the lungs may vary from a minimal incision of the visceral pleura and enucleation of a hamartoma to a pneumonectomy. Most resections are unilateral, but synchronous bilateral excisions may be carried out. The standard procedures (Table 26-1) may be extended to include excision of a part of the chest wall; one of the thoracic parietes (pleura, pericardium, or diaphragm); an adjacent vascular structure (portion of the atrium or vena cava); and rarely part of the esophagus. Some pulmonary resections may be accomplished using local anesthesia (open lung biopsy), but most are performed with general endotracheal anesthetic management (see Chapter 22). In spite of the above similarities, a fundamental variation in practice can be found as to the approach to the chest cavity given the customary introduction of video-assisted thoracic surgery (VATS) or hybrid VATS/muscle-sparing limited thoracotomy in the surgical armamentarium in order to reduce incision-related morbidity. Indeed, after decades of consolidated practice, the general features of pulmonary resections are changing, being currently focused on the evaluation of performance by refining preoperative risk evaluation and adopting both minimally invasive surgery techniques and innovative protocols of postoperative care aimed at fast-tracking thoracic surgical patients.
Operative Positions and Thoracic Incisions
Although each operative procedure has its own unique features, the standard operations are performed with the patient in the lateral decubitus, supine, or prone position. The selection of patient position is determined by the operation planned and in part by the patient’s physiologic condition. The supine position is associated with fewer physiologic changes in the patient’s cardiopulmonary function than are noted with the other positions. While the lateral position permits the best access to the hilum of the lung and is the preferred position for VATS and hybrid procedures, the prone position can be used only in selected circumstances, mainly when the main bronchus needs to be dissected first to avoid spillage of secretions toward the contralateral lung. However, the routine use of double-lumen tubes and bronchial blockers has obviated the need of surgical bronchial isolation. The supine position is still utilized to perform anterior thoracotomies, either unilateral or bilateral, with or without transverse sternotomy to perform pulmonary resections and lung transplantation. Access to the hilum seems to be somewhat impaired with the anterior approach compared to the lateral. In addition, median sternotomy can also be used to perform pulmonary resections, even though access to the left inferior pulmonary vein is hindered by its retrocardiac position. The various incisions and modifications for conduct of open thoracic pulmonary resections are discussed elsewhere. The advent of minimally invasive techniques—VATS—has resulted in the employment of multiple small (1 to 4 cm in length) ports located at selected sites in the chest wall through which the necessary instruments for the selected VATS procedures may be inserted (see Chapter 33).
A compromise solution between rigorously performed VATS and traditional open approaches consists of adding a small incision to the improved visualization attainable through video assistance to provide the ability to safely control the vascular hilum for centrally located lesions. Therefore a rib-spreading, muscle-sparing lateral minithoracotomy associated with two port incisions for video assistance and the insertion of endoscopic instrumentation can be used for all kinds of pulmonary resections, including lung transplantation.75
Even with “traditional” open procedures, the standard thoracotomies are reserved for special circumstances, while the trend is to use shorter posterolateral or fully lateral incisions and to spare the division of the major thoracic muscles as much as is compatible with appropriate operative exposure. As a consequence, the subperiosteal resection of a rib is done infrequently, whereas the division or excision of a small posterior portion of a rib or ribs adjacent to the intercostal incision to improve exposure and prevent a possible fracture of the rib as the intercostal space is retracted is practiced on an individual basis. If a fracture of one or more ribs occurs, control of any bleeding is mandatory, and fixation of the fracture site by sutures is indicated to prevent overriding of the fractured ends and further vascular injury or the occurrence of severe postoperative pain on chest wall movement. As a general rule, the rib cage is closed with pericostal sutures; however, Cerfolio and associates19 have suggested the use of intracostal sutures to decrease postoperative
incisional pain. In this closure, the sutures are placed through the tissues and periosteum on top of the fifth rib and through small holes drilled in the sixth rib. These investigators found that patients experienced less pain 2 weeks and 1, 2, and 3 months after thoracotomy when compared with that of patients with a standard closure. These results, of course, need to be confirmed.
incisional pain. In this closure, the sutures are placed through the tissues and periosteum on top of the fifth rib and through small holes drilled in the sixth rib. These investigators found that patients experienced less pain 2 weeks and 1, 2, and 3 months after thoracotomy when compared with that of patients with a standard closure. These results, of course, need to be confirmed.
Table 26-1 Pulmonary Resections | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
General Techniques
The specific techniques of the various standard pulmonary resections are discussed in their respective chapters. The technique of VATS resection is discussed in detail in Chapters 33 and 35. As an introduction, however, a discussion of the general features of the dissection and management of the bronchi, large vessels, and lung surfaces is appropriate.
Dissection and Control of the Major Arteries
Dissection of a major pulmonary artery is carried out with care. The vessel is thin-walled and is easily injured. Simultaneous traction and countertraction on the vessel wall before the proper plane has been established is to be avoided. The fascial envelope can be retracted as the vessel wall is dissected away from it (Fig. 26-1). Pulling on a branch of the artery is also best avoided because the branch may easily be partially or completely avulsed from the main vessel wall, especially at the level of the left upper lobe branches. In this setting, it must be remembered that additional distal length for vessel ligation can be obtained by careful dissection of the branches as they enter the lung parenchyma. Both sharp and blunt dissection should be used, and finger mobilization of the posterior aspect of the larger vessels is helpful. In dissecting the main pulmonary artery on the right side, the truncus anterior of the artery may be isolated and divided to obtain greater length of the mainstem vessel. On the left side, the pulmonary artery may be isolated up to or even proximal to the ligamentum arteriosum, although one must guard against injury to the recurrent laryngeal nerve as it passes underneath the aortic arch from the front to the back of the aorta at this point. The concept of achieving subadventitial control of the pulmonary artery becomes the mainstay of a correct surgical conduct while performing major pulmonary resections, both by VATS or through the traditional approach. The ligation of a major artery is accomplished in several ways. If it is long enough, the vessel may be doubly ligated with No. 2-0 or 3-0 nonabsorbable suture. The proximal end is then suture ligated between the two ligatures before division of the vessel. A simple transfixation suture is not sufficient, but a figure-eight suture through the center of the vessel and tied around it is satisfactory. The vessel is then divided. If the vessel is too short to ligate safely in this manner, the artery may be held with two vascular clamps and divided and the proximal cut end closed with a continuous No. 4-0 or 5-0 nonabsorbable monofilament suture. Some surgeons prefer to treat the pulmonary artery in this manner as a routine procedure. After proximal clamping and division to leave a sufficient arterial cuff, Blalock’s technique may be used to close the main pulmonary artery in such a way as to create two rows of nonabsorbable sutures. This technique consists of an in-and-out deep row and a running more superficial one of No. 4-0 or 5-0 nonabsorbable monofilament sutures. The concept of having two or three proximal suture lines to ensure safe closure of the pulmonary vessels is similar to the one adopted in the development of mechanical vascular closure. Indeed, a third method of controlling the vessel is the use of a mechanical stapling device such as a TA-30 instrument using 3.5-mm or V staples. Deslauriers25 suggests the use of the roticulator vascular stapler for the control of short stumps. Recently, several authors have reported on the use of endostapler, with and
without roticulating ability, to proceed to major pulmonary resection for centrally located tumors during so-called hybrid (open and VATS) techniques.75 The resort to endostaplers is a routine practice for major pulmonary resections performed through an integral VATS approach (Chapters 33 and 35), for which these instruments were originally designed. Endostapler cartridges are usually selected according to the thickness of the tissue to be divided, from green (suitable for the bronchial structures) to blue (lung parenchyma), white (main vein and pulmonary artery trunks), and gray (for smaller vessels).
without roticulating ability, to proceed to major pulmonary resection for centrally located tumors during so-called hybrid (open and VATS) techniques.75 The resort to endostaplers is a routine practice for major pulmonary resections performed through an integral VATS approach (Chapters 33 and 35), for which these instruments were originally designed. Endostapler cartridges are usually selected according to the thickness of the tissue to be divided, from green (suitable for the bronchial structures) to blue (lung parenchyma), white (main vein and pulmonary artery trunks), and gray (for smaller vessels).
The smaller branches of the artery may be satisfactorily controlled by triple ligation and division between the two most distal ligatures or with vascular endostaplers. Delicate handing of these ligatures is of paramount importance to avoid back-bleeding from the lung side. Simple proximal clipping of the arterial branches is generally contraindicated, since clips tend to slip off the vessel, as demonstrated in the VATS lobectomy experience (Chapter 35). Surgeons in training should be made familiar with both hand-sewn and stapling techniques so as to be prepared for unexpected difficulties inside the chest.
If injury to the vessel occurs, as a general principle the bleeding should be controlled initially by pressure with a gauze sponge, guarding against any maneuver that might further tear the vessel. Next, adequate exposure is ensured and both proximal and distal control beyond the injury obtained; or, when possible, a fine vascular clamp is applied directly to control the injured site. Repair is accomplished with an over-and-over fine vascular suture material. Reinforcing sutures with pledgets can also be an option to avoid further tearing of the fragile vessel wall.
Dissection and Control of the Major Veins
The major pulmonary veins and their branches are managed in a manner not dissimilar to that described for the pulmonary artery. The walls of the veins are stronger than those of the arteries, and injuries to them are less likely to occur. Occasionally it is necessary to enter the pericardium to obtain sufficient length of the superior or inferior pulmonary vein. After the vessel is free of the pericardial reflections (see Chapter 5), the vein is usually divided between vascular clamps and closed with a fine continuous vascular suture. Nowadays a vascular stapler is also commonly used. Even a portion of the left atrial wall may be included in the excision, and the atrial incision is closed in the standard manner. The pericardial defect, if small, is closed. If the opening is too large to close without compromise of the pericardial space, one must prevent postoperative herniation of the heart through the pericardial defect, especially on the right side. Piccione and Faber65 suggest closing all large defects, either right- or left-sided, routinely with a soft tissue patch. Harvey44 and Sugarbaker74 and their colleagues suggest that fenestration of the soft tissue patch be made to permit egress of fluid out of the pericardial sac to avoid the possibility of a pericardial tamponade.
Ligation of the veins as the initial step in a pneumonectomy for carcinoma has been advocated so as to lessen the possibility of spilling tumor cells into the circulation. Yael and coworkers88 have suggested that the routine use of this maneuver may not be oncologically beneficial. In addition, investigators have demonstrated that, irrespective of the sequence of vessel ligation, the amount of blood accumulating in the resected lobe is minimal.90
Fissure Dissection
An incomplete or fused fissure presents a bridge of parenchymal tissue of different thickness connecting two lobes. Three main layers are encountered while deepening the dissection, with the most superficial one occasionally presenting communicating venous branches that are sometimes erroneously interpreted as arterial vessels, since their injury can cause significant bleeding. In the second layer, perivascular lymph nodes usually overlie the pulmonary artery, which rests on the corresponding bronchus, forming the third deepest layer (see Chapter 5).
There are two methods to approach incomplete or fused fissures. The most commonly used is represented by the identification of the fissural artery by blunt and sharp dissection (see also Chapter 28). The second avoids this dissection and the attendant risk for prolonged air leaks; it relies on known anatomic boundaries to divide fissures prior to addressing hilar vessels. An example of the former is the development of the posterior part of a fused major fissure on the right side. The “floor” of the confluence of the major and minor fissures usually hides the artery accompanying the bronchus intermedius, which lies deep to the artery. From the medial aspect of this segment of the vessel depart the branches to the middle lobe, whereas, often at this same level but from the lateral aspect of artery, the takeoff of the artery to the apical segment of the lower lobe (S6) is found. In a more cranial position, aiming at the right-upper-lobe bronchus, one can easily identify the posterior ascending artery to the upper lobe. The dissection onto the subadventitial plane enables the surgeon not only to recognize possible anatomic variations but also, having identified the S6 arterial branch (A6), to conduct the dissection posteriorly toward the bronchial bifurcation between upper-lobe bronchus and the intermedius until the subcarinal area in the posterior mediastinum is reached. The incomplete fissure can then be divided in a safe, usually avascular plane running from flush of A6 to the subcarinal area, just caudal to the loop of the azygos vein.
The fissureless technique is based on the identification of anatomic corridors running from the anterior to the posterior aspects of the lobes and defined by vascular landmarks (i.e., on the right side, the posterior ascending artery to the upper lobe and the upper venous trunk) as the gates of these corridors. Once the gates are eluded or removed (i.e., the corresponding vessels divided), these passageways can accommodate the anvil of a stapler. Largely fused fissures and anthracotic adenopathies are the main reasons to attempt at performing lobectomy without developing the interlobar fissural plane in the traditional fashion via the fissureless technique.81 Reportedly, this approach reduces the incidence of persistent air leaks and length of hospitalization.39 In these circumstances, “fissureless” techniques have been proposed that obviate the need of intrafissural dissection of the artery by dividing known anatomic passageways. On the left side, the division starts from the posterior aspect of the main pulmonary artery, remaining flush to the superficial aspect of the artery and thereby respecting the upper lobe branches, and proceeds anteriorly to end just caudal to the upper vein. On the right side, the ideal dissection line starts at the level of the posterior ascending artery to the upper lobe and aims towards the caudal border of the superior pulmonary vein;
caution should be taken at identifying supernumerary anterior arterial branches to the upper lobe, which may get in the way of such dissection.
caution should be taken at identifying supernumerary anterior arterial branches to the upper lobe, which may get in the way of such dissection.
Dissection and Closure of the Bronchus
Main Bronchus
The main bronchus is usually the last hilar structure isolated in a pulmonary resection, although some surgeons still endorse the bronchus-first technique, especially for right-sided resections.42 Regardless, whether the bronchus is the first or last structure mobilized, the technique of handling the bronchus remains essentially the same. On the right side, the dissection can be carried up to the tracheal carina without difficulty, but care is taken, even during lymph node dissection, not to completely denude the bronchus of its investing adventitial tissue and the contained blood supply. On the left side, the main bronchus should likewise be freed to the tracheal bifurcation, but this effort is more tedious because of its position within the aortic window. The proximal site of division of a main bronchus should be close to the bifurcation, and the line of division should be placed across the bronchus to avoid a blind pocket on its lateral side. Moreover, the residual stump should be as short as possible. As a general rule, a clamp need not be placed proximal to the proposed line of division when a manual suture closure of the stump is to be done. Similarly, it is unnecessary if a stapling device is to be used to secure closure. Takaro77 and Asamura8 summarized the use and advantages of different mechanical staplers in bronchial closure. There appears to be consensus on the need for a staple size of 4.8 mm if a mechanical stapler is used on the main bronchus in order to reduce the incidence of breakdown of the bronchial closure. There are controversial reports in the literature as to which suturing technique is endowed with a better tolerance of inflation pressure.29,51 Interestingly, after 2 weeks from the operation, Ludwig and coworkers52 were not able to demonstrate experimentally any difference between hand-sewn and mechanically stapled bronchial stumps with regard to pressure resistance.
With hand-sewn techniques, a 1.4% to 2.4% rate of bronchopleural fistula has been reported.5,47 It appears that the recently noted decrease in incidence of a bronchial stump breakdown is more likely the result of a different selection of patients undergoing operations. With the use of the standard stapler, however, Vester and associates86 reported only a 1.6% incidence of bronchial leak. In reviewing the experience with over 700 pneumonectomy patients, the Mayo Clinic group found mechanical stapling as having a protective effect against bronchopleural fistula formation, an event occurring in 4.5% of the entire series.24
In the manual closure of the bronchus, an occluding clamp is placed distal to the line of division to prevent soilage of the operative field from any contained material within the distal bronchial tree. A suture is placed in each lateral side of the bronchus just proximal to the line of excision, and the bronchus is divided, either completely before closure or in sequence to avoid a completely open stump. With either method, the posterior membranous wall is approximated to the anterior cartilaginous wall with interrupted single or mattress No. 00-0 or No. 000-0 sutures of the operator’s choice. Nonabsorbable suture, such as fine monofilament stainless steel wire suture, and synthetic monofilament suture, such as Vicryl or Prolene, are the presently acceptable suture materials. Before complete closure, the proximal stump and trachea should be aspirated by means of a sterile catheter. After the closure is complete, the stump is tested for any persistent air leaks by covering the stump with a sterile solution and having the anesthesiologist apply or increase inspiratory pressure to that side of the tracheobronchial tree. Areas of leakage are controlled by additional sutures as necessary. Occasionally, a small tear in the membranous wall of the closed stump is identified. A buttress of adjacent tissue or a pledget of synthetic material should then be incorporated into a mattress suture closure of the area.
Frequently, one or two bronchial arteries need to be ligated after the bronchus has been divided. If bleeding is not controlled, these vessels may serve as a significant source of postoperative blood loss; the bronchial arterial system carries about 1% of the cardiac output.
After closure of the proximal end, the bronchial stump is covered with adjacent tissue, such as a pleural flap, the azygos vein, a pedicle graft of pericardial fat, or adjacent pericardium to provide the stump with a viable tissue cover to help prevent the possible development of a leak from the stump, which normally heals by secondary intention. This cover is particularly important on the right side because no natural coverage for the stump is available. On the left side, the short proximal stump recedes into the depth of the aortic window and is surrounded by the adjacent tissues.
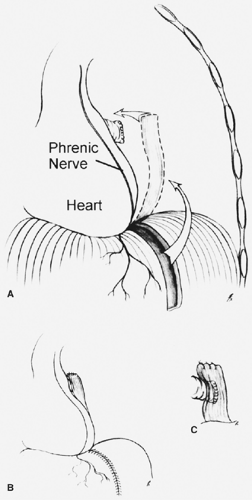
Further precautions to protect the stump and ensure healing are indicated in the patient who has received preoperative neoadjuvant chemotherapy and irradiation89; who has a positive sputum containing multidrug-resistant Mycobacterium tuberculosis, or, even more so, with the presence of environmental mycobacteria such as Mycobacterium avian complex organisms; who is undergoing a completion pneumonectomy for a recurrent or continuing severe inflammatory process after a previous lesser resection; or in whom a bronchopleural fistula is being closed. In all these situations, the risk for bronchial dehiscence is increased. McGovern and associates56 have stressed the increased morbidity and problems associated with the bronchial stump in patients undergoing a completion pneumonectomy for an inflammatory disease. As prophylaxis against bronchial dehiscence, coverage of the stump is recommended using a transplanted muscle flap, as described by Pairolero and Payne64 and Fujimoto and colleagues.35 The muscle flap may be obtained from the latissimus dorsi, the pectoralis major, or the serratus anterior muscles. An intercostal muscle flap may also be used, but one must make sure that all periosteum has been removed, because ossification may occur from this tissue at a later date. The rationale behind covering the bronchial stump with viable tissue, such as the intercostal muscle, lies in the reconstitution of an adequate blood supply to the denuded bronchus rather than a mere mechanical reinforcement.37 Indeed, the use of an intercostal muscle flap is effective and devoid of major complications.53 Sayeed-Shah and associates69 have suggested the use of a muscle flap from the hemidiaphragm to cover this stump (Fig. 26-2). Brown and Pomerantz12 have used muscle flaps extensively in patients with multidrug-resistant M. tuberculosis infection who undergo major pulmonary resections. The use of an omental flap is also satisfactory in these situations. In addition, the resort to a pericardial fat pad, as originally described by Brewer and
colleagues in 1953, to achieve protection of a potentially compromised bronchial stump has been proposed by Taghavi and associates.76
colleagues in 1953, to achieve protection of a potentially compromised bronchial stump has been proposed by Taghavi and associates.76
Lobar and Segmental Bronchi
The surgical closure of the divided lobar or segmental bronchi entails the same principles and techniques of management as for the mainstem bronchi. At present, bronchial closure with a 3.5- or 4.8-mm stapling device is generally preferred, depending on the compliance of the bronchus.
Suture material includes silk, monofilament, polyglactin, or polypropylene. Fell and Kirby32 suggest that the sutures be placed about 3 mm apart and 3 mm from the cut edge. As a general rule, it is unnecessary to cover these bronchial stumps with additional tissue when sufficient pulmonary parenchymal tissue is present, which, on inflation, surrounds the bronchial stump. If one is unsure that this will occur, simple coverage with a freed pleural flap is sufficient. When multidrug-resistant mycobacterial organisms are present in the sputum or preoperative neoadjuvant therapy including irradiation has been used, a more secure coverage of a lobar bronchial stump is indicated.41 A transposed muscular flap, a vascularized pericardial flap, or even an omental flap should be added to support the closure. When a residual pleural space or a major air leak is anticipated, one of several maneuvers can be carried out. If an apical space is anticipated (after an upper lobectomy), an apical pleural tent to reduce the pleural space may be constructed. Conlan20 discussed the technique of constructing the tent and its fate. More recently, Brunelli and associates13 have used this procedure to lessen and shorten the period of air leaks. In 2002, the same authors14 reported a randomized study of the efficacy and duration of effect in 200 upper lobectomy patients; 100 patients underwent construction of a pleural tent and 100 did not. The patients with the tent had significant reduction of the mean duration of air leaks (2.5 versus 7.2 days), number of days a chest tube was required (7.0 versus 11.2 days), and length of hospital stay (8.2 versus 11.6 days). Costs were also reduced. In the absence of sufficient or useful apical parietal pleura, a muscle transposition (latissimus dorsi, pectoralis major flap) or other chest wall muscle flap may be used to reduce the size of the pleural space.68 The method is described in Chapter 50.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree