Atrial fibrillation (AF) is 1 of the most important healthcare issues and an important cause of healthcare expenditure. AF care requires specific arrhythmologic skills and complex treatment. Therefore, it is crucial to know its real affect on healthcare systems to allocate resources and detect areas for improving the standards of care. The present nationwide, retrospective, observational study involved 233 general practitioners. Each general practitioner completed an electronic questionnaire to provide information on the clinical profile, treatment strategies, and resources consumed to care for their patients with AF. Of the 295,906 patients screened, representative of the Italian population, 6,036 (2.04%) had AF: 20.2% paroxysmal, 24.3% persistent, and 55.5% permanent AF. AF occurred in 0.16% of patients aged 16 to 50 years, 9.0% of those aged 76 to 85 years, and 10.7% of those aged ≥85 years. AF was symptomatic despite therapy in 74.6% of patients and was associated with heart disease in 75%. Among the patients with AF, 24.8% had heart failure, 26.8% renal failure, 18% stroke/transient ischemic attack, and 29.3% had ≥3 co-morbidities. The rate control treatment strategy was pursued in 55%. Of the 6,036 patients with AF, 46% received anticoagulants. The success rate of catheter ablation of the AF substrate was 50%. In conclusion, in our study, the frequency of AF was 2 times greater than previously reported (approximately 0.90%), rate control was the most pursued treatment strategy, anticoagulants were still underused, and the success rate of AF ablation was lower than reported by referral centers.
Atrial fibrillation (AF) is 1 of the most important public health issues, occurring in approximately 1% of the general population, and 1 of the most important causes of healthcare expenditure in western countries. In the past, several randomized controlled studies were performed to assess the most appropriate treatment of AF. The results of these studies have provided the framework for guidelines on AF management, which are based primarily on the firm recommendation of thromboprophylaxis in patients with a high risk of stroke and on 2 well-defined treatment strategies (rhythm control and rate control). Recently, several observational studies have assessed the overall adherence of in-hospital cardiologists and internists and out-hospital cardiologists to the guideline recommendations. However, only a few studies have been performed to obtain comparable information in the much more complex setting of the community in which many patients have only occasional or no contact at all with hospitals or specialists, and, thus, it is more difficult to accurately apply the guideline recommendations. Therefore, the Italian Association of Hospital Cardiologists and the Italian College of General Practitioners promoted a nationwide, retrospective, observational study to assess, in a large sample of the Italian population, the frequency of diagnosed AF and the current care of AF, and to detect potential areas of improvement in the standards of AF care.
Methods
In Italy, every resident is registered with a general practitioner (GP) who cares for their patients and keeps track of their clinical history. In the past few years, the Italian College of General Practitioners has developed a research network consisting of 800 GPs interested in research in primary care and trained for high-quality data entry; all use the same office software (Millewin, Millenium srl, Florence, Italy). The 600 best GPs (measured by the quality of the data records) were invited to participate in the present survey, and 233 GPs confirmed their participation in the study. From May 17 to June 22, 2011, all subjects aged ≥15 years cared for by the 233 GPs were screened, and those with AF diagnosed (supported by electrocardiographic findings or the diagnosis recorded on a hospital discharge summary) were included in the present study. For each patient with AF, the GPs were required to complete an electronic questionnaire to provide the following data: the demographic and clinical characteristics of the patients with AF and the number of some of the selected diagnostic and therapeutic procedures performed in the previous 5 years, the treatment strategies pursued and the current medical therapy, and the catheter ablation results. Most data were automatically extracted by the GPs from their own databases. The remaining data, which could not be extracted automatically by the computerized procedure, were collected manually. The automatic extraction included: AF (with a codified diagnosis of International Classification of Diseases, 9th revision, code IX 427.31), relevant cardiovascular and noncardiovascular diseases, patient baseline characteristics, therapy, test prescription (echocardiography, Holter electrocardiographic monitoring, exercise testing), and hospitalizations. The CHADS 2 score (congestive heart failure, hypertension [blood pressure consistently >140/90 mm Hg or treated medically], age ≥75 years, diabetes mellitus, and previous stroke, transient ischemic attack, or thromboembolism; the presence of each gives a score of 1, but the last, which has a score of 2) was automatically calculated. The manual data collection included AF classification, AF-related symptoms, management strategy (rhythm vs rate control, medications), level of engagement of the GP in the diagnosis and management of AF, number of attempts and methods used to restore sinus rhythm, use of electrophysiologic testing, and use of AF substrate catheter ablation. Paroxysmal AF was defined as an episode, usually self-terminating within 48 hours, in particular within 7 days, but always terminating spontaneously. Persistent AF was defined as an episode either lasting >7 days or requiring termination by cardioversion. Permanent AF was considered present when interventions to restore sinus rhythm were no longer considered appropriate (regardless of the reason). AF was classified as “lone AF” when occurring in the absence of heart disease, hypertension, heart failure, chronic obstructive pulmonary disease, diabetes, renal failure, dementia, cerebrovascular disease, obesity, smoking, abuse of alcohol consumption, hyperthyroidism, and hypothyroidism. Patients were assigned to the rhythm control strategy when a willingness to maintain sinus rhythm (previous electrical or pharmacologic cardioversion, chronic use of antiarrhythmic drugs, catheter ablation of the substrate) was present and to a rate control strategy when no attempt to maintain sinus rhythm or no use of drugs or intervention specifically directed to maintain sinus rhythm was pursued. AF ablation was considered effective in the absence of AF recurrence, as determined by referred symptoms or electrocardiographic recordings, and an optimum quality of life was present. It was considered moderately effective in the presence of both >50% reduction in AF recurrence and significant improvement in quality of life. It was considered ineffective in the absence of a significant reduction of AF recurrence, with no improvement in the patient’s quality of life.
Data were collected as aggregate and analyzed using standard descriptive statistics. To assess the presence of possible differences with regard to the distribution by age and gender of the Italian Survey of Atrial Fibrillation Management (ISAF) population and the Italian population (Italian Institute of Statistics Life Tables), the Kolmogorov-Smirnov test was used. To assess the prevalence of AF in Italy, the crude frequencies of AF observed in the subgroups of the ISAF population were adjusted to similar subgroups of the Italian population (Italian Institute of Statistics Demographic Tables) using the direct standardization rates method.
Results
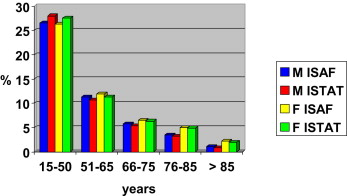
We studied a population of 295,906 subjects aged ≥15 years (51.9% female) cared for by 233 GPs. The GPs and ISAF population were homogeneously distributed across Italy, with 31% and 32% in the northern regions, 24% and 23% in the central regions, 28% and 29% in the southern regions, and 17% and 16% in the islands, respectively. The Kolmogorov-Smirnov test results showed that the ISAF and Italian populations were similar with regard to gender and age distribution ( Figure 1 ). The distribution of the entire ISAF population and of the patient subgroups according to age and gender is listed in Table 1 . The diagnosis of AF was recorded and confirmed in 6,036 patients (51% female). The frequency of AF was 2.04% (95% confidence interval 1.99 to 2.09) in the global ISAF population: 2.4% in Northern Italy, 2.1% in Central Italy, 1.7% in Southern Italy and 1.8% in the Islands. The frequency of AF increased with age, with patient subgroups aged 66 to 75 years and 76 to 85 years contributing most (26.8% and 37.5%, respectively). The AF frequency ratio between males and females was ≥1.2 in each age subgroup. When the frequency of AF observed in the subgroups of the ISAF population was extrapolated to the Italian population of the same age and gender, it appeared that in Italy, the prevalence of AF is 1.85%.
| Age (yrs) | Study Population (n = 295,906) | AF Population (n = 6,036) | AF Frequency | ||||
|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Total | Male | Female | |
| 15–50 | 78,415 (26.5%) | 77,823 (26.3%) | 183 (3%) | 65 (1.1%) | 0.16% | 0.23% | 0.08% |
| 51–65 | 33,437 (11.3%) | 35,213 (11.9%) | 527 (8.7%) | 340 (5.6%) | 1.3% | 1.6% | 0.97% |
| 66–75 | 16,867 (5.7%) | 19,235 (6.5%) | 821 (13.6%) | 795 (13.2%) | 4.5% | 4.9% | 4.1% |
| 76–85 | 10,357 (3.5%) | 14,794 (5%) | 1,028 (17%) | 1,237 (20.5%) | 9.0% | 9.9% | 8.4% |
| ≥86 | 3,255 (1.1%) | 6,510 (2.2%) | 397 (12.2%) | 643 (9.9%) | 10.7% | 12.2% | 9.9% |
At the time of the survey, 19.4% of patients had had only 1 episode of AF in the previous 5 years; 20.2% had paroxysmal, 24.3% persistent, and 55.5% permanent AF. Lone AF was diagnosed in 1.2% of patients. The clinical characteristics of the patients with AF are listed in Table 2 . Approximately 2/3 of our patients had cardiac disease, almost all (91.5%) had ≥1 co-morbidity, 1/3 had ≥3 co-morbidities, and ¼ had heart failure. The AF history was >5 years in ½ of the patients (48.2%). Among those with >1 episode of AF (commonly treated with medical therapy), 25.4% did not report any symptoms related to the arrhythmia.
| Characteristic | Total (n = 6,036) |
|---|---|
| Female gender | 3,080 (51%) |
| Atrial fibrillation type | |
| Paroxysmal | 1,218 (20.2%) |
| Persistent | 1,465 (24.3%) |
| Permanent | 3,353 (55.5%) |
| Lone atrial fibrillation | 73 (1.2%) |
| Duration of atrial fibrillation history ∗ (yrs) | |
| <1 | 760 (12.7%) |
| 1–5 | 2,339 (39.1%) |
| 6–10 | 1,811 (30.3%) |
| >10 | 1,074 (17.9%) |
| Current atrial fibrillation symptoms | |
| None | 1,522 (25.4%) |
| Palpitations | 2,457 (39.4%) |
| Asthenia | 1,471 (24.6%) |
| Dyspnea | 1,417 (23.7%) |
| Other | 281 (4.7%) |
| No heart disease | 1,433 (23.7%) |
| Coronary artery disease | 1,145 (19%) |
| Hypertension and left ventricular hypertrophy | 2,203 (36.5%) |
| Ischemic dilated cardiomyopathy | 237 (3.9%) |
| Nonischemic dilated cardiomyopathy | 122 (2%) |
| Valvular disease | 735 (12.2%) |
| Other heart disease | 153 (2.5%) |
| Hypertension | 4,023 (66.7%) |
| Diabetes | 1,343 (22.2%) |
| Diabetes plus vascular complications | 420 (7%) |
| Cerebrovascular disease † | |
| Ischemic stroke | 448 (7.5%) |
| Hemorrhagic stroke | 70 (1.2%) |
| Transient ischemic attack | 560 (9.3%) |
| Psychological disturbance | 1,129 (18.9%) |
| Dementia | 891 (14.9%) |
| Renal failure † | |
| Glomerular filtration rate 30–60 ml/min/1.73 m 2 | 1,350 (22.6%) |
| Glomerular filtration rate <30 ml/min/1.73 m 2 | 218 (3.6%) |
| Dialysis | 36 (0.6%) |
| Hyperthyroidism | 267 (4.5%) |
| Hypothyroidism | 456 (7.6%) |
| Chronic obstructive pulmonary disease | 1,114 (18.7%) |
| Obstructive sleep apnea | 268 (4.5%) |
| Other pulmonary disease | 226 (3.8%) |
| ≥3 Co-morbidities | 1,770 (29.3%) |
| Obesity (body mass index ≥30 kg/m 2 ) | 1,198 (20%) |
| Heart failure hospitalizations (n) † | 1,486 (24.8%) |
| None | 613 (10.2%) |
| 1–3 | 726 (12.1%) |
| >3 | 147 (2.5%) |
| No co-morbidity | 512 (8.5%) |
| Smoke | 542 (9%) |
| Alcohol abuse | 143 (2.4%) |
| Implantable defibrillator | 179 (3%) |
The clinical characteristics, antiarrhythmic therapy, and antithrombotic therapy of the patients with AF, according to the treatment strategy assignment, are summarized in Table 3 . The rhythm control strategy was pursued in 43.8% of the patients and the rate control strategy in 54.8%; in the remaining 1.4%, the strategy was not defined. Among the rhythm control patients, 43.1% were aged ≥75 years, most had cardiac disease, 45.5% had paroxysmal AF, 54.5% had persistent AF, and 54.5% had received ≥1 electrical or pharmacologic cardioversions (11% >3 attempts). In the 5 years preceding the present study, 54.5% of the patients had experienced ≥1 AF recurrences. β Blockers were the drugs prescribed most, followed by class 1C antiarrhythmic drugs (21.5%) and amiodarone. Ablation of the AF substrate or pacemaker/defibrillator implantation was performed in few patients. In addition, in the rhythm control group, 50.8% had a CHADS 2 score of ≥2, 26.6% did not receive any antithrombotic therapy, and 28.4% were treated with oral anticoagulation (OAC) therapy. In particular, only <1/2 (45.4%) of the 1,308 patients with a CHADS 2 score of ≥2 received OAC therapy and only <1/2 (44.4%) of the 714 patients who did not receive warfarin presented with valid reasons not to be treated (side effects, refusal, no compliance, risk of bleeding). Of the rate control patients, 64.3% were ≥75 years old, the proportion of patients with cardiac disease was similar to that in the rate control group. β Blockers were prescribed most, followed by digitalis, verapamil-diltiazem, and combinations of drugs. Atrioventricular junction ablation and pacemaker implantation (ablate and pace) were performed in a few patients. A CHADS 2 score of ≥2 was present in 71.8% of patients, and OAC was prescribed in 59.6%. In particular, of the 2,378 patients with a CHADS 2 score of ≥2, approximately ¾ (73.2%) received OAC therapy. Of the 664 patients who did not receive OAC, 69.1% presented with valid reasons not to be treated.
| Characteristic | Rhythm Control (n = 2,643; 43.8%) | Rate Control (n = 3,310; 54.8%) |
|---|---|---|
| Age (yrs) | ||
| 15–50 | ||
| Male | 141 (5.3) | 36 (1.1) |
| Female | 44 (1.7) | 15 (0.5) |
| 51–65 | ||
| Male | 323 (12.2) | 196 (5.9) |
| Female | 204 (7.7) | 134 (4.0) |
| 66–75 | ||
| Male | 406 (15.4) | 408 (12.3) |
| Female | 386 (14.6) | 393 (11.9) |
| 76–85 | ||
| Male | 395 (15) | 618 (18.7) |
| Female | 469 (17.7) | 758 (22.9) |
| >85 | ||
| Male | 103 (3.9) | 289 (8.7) |
| Female | 172 (6.5) | 463 (14) |
| Heart disease | 1,906 (72.1) ∗ | 2,623 (79.2) |
| CHADS 2 score † | ||
| 0 | 486 (18.4) ‡ | 226 (6.8) |
| 1 | 784 (29.7) ‡ | 706 (21.3) |
| 2 | 791 (30.7) ‡ | 1,156 (34.9) |
| >2 | 517 (20.1) ‡ | 1,222 (36.9) |
| Antiarrhythmic therapy | ||
| No | 425 (16.5) ‡ | 532 (16.1) |
| β Blockers | 730 (28.3) ‡ | 1,227 (37.1) |
| Propafenone | 269 (10.4) ‡ | — |
| Flecainide | 285 (11.1) ‡ | — |
| Amiodarone | 447 (17.3) ‡ | — |
| Dronedarone | 37 (1.4) ‡ | — |
| Digitalis | — | 798 (24.1) |
| Verapamil/diltiazem | 134 (5.2) ‡ | 295 (8.9) |
| Combination of drugs | 140 (5.4) ‡ | 402 (12.1) |
| Pacemaker | 110 (4.3) ‡ | 56 (ablate and pace; 1.7) |
| Ablation of atrial fibrillation | 174 (6.7) ‡ | 0 |
| Antithrombotic therapy | ||
| No | 686 (26.6) ‡ | 273 (8.2) |
| Antiplatelet agents | 1,164 (45.1) ‡ | 1,054 (31.8) |
| Oral anticoagulation | 728 (28.2) ‡ | 1,974 (59.6) |
| Antiplatelet and oral anticoagulation | 4 (0.16) ‡ | 9 (0.27) |
| CHADS 2 ≥2 and oral anticoagulation | 594/1,308 (45.4) | 1,741/2,378 (73.2) |
† Congestive heart failure, hypertension (blood pressure consistently >140/90 mm Hg or treated medically), age ≥75 years, diabetes mellitus, and previous stroke, transient ischemic attack, or thromboembolism; the presence of each gives a score of 1, but the last, which has a score of 2.
Of the whole study population, the CHADS 2 score was 0 in 12.1%, 1 in 25.3%, and ≥2 in 62.6%; 46% of the patients received OAC, 37.5% ≥1 antiplatelet agent, and 16.5% received no antithrombotic therapy.
In the 5 years preceding the ISAF study, catheter ablation of the AF substrate was performed in 174 patients (2.9% of all patients with AF). Of these patients, 69% were 51 to 75 years old, 55.7% had heart disease, and most had persistent AF (80.5%). Palpitation was the most frequent indication for ablation, followed by asthenia and dyspnea. In 26.4% of the patients, the ablation was repeated ≥2 times. After ablation, 67.8% of patients continued to take antiarrhythmic drugs; 55.2% were treated with OAC ( Table 4 ). The GPs considered the results of the ablation procedure effective in 50.6% of cases, moderately effective in 30.4%, and ineffective in 19%.
| Characteristic | n (%) |
|---|---|
| Gender | |
| Male | 112 (64.4) |
| Female | 62 (35.6) |
| Age (yrs) | |
| 16–50 | |
| Male | 15 (8.6) |
| Female | 4 (2.3) |
| 51–65 | |
| Male | 46 (26.4) |
| Female | 15 (8.6) |
| 66–75 | |
| Male | 34 (19.5) |
| Female | 25 (8.6) |
| >75 | |
| Male | 17 (9.8) |
| Female | 18 (10.3) |
| Atrial fibrillation type | |
| Paroxysmal | 34 (19.5) |
| Persistent | 140 (80.5) |
| Heart disease | 97 (55.7) |
| Previous cardioversion | |
| 0 | 24 (13.8) |
| 1–3 | 90 (51.7) |
| >3 | 52 (29.9) |
| Unknown | 8 (4.6) |
| Symptoms leading to ablation | |
| Palpitations | 144 (82.8) |
| Dyspnea | 83 (47.7) |
| Asthenia | 90 (51.7) |
| Other | 3 (9.8) |
| Catheter ablation | |
| 1 | 117 (67.2) |
| 2 | 40 (23) |
| ≥3 | 6 (3.4) |
| Unknown | 11 (6.3) |
| Postablation antiarrhythmic drugs | |
| Propafenone | 20 (11.5) |
| Flecainide | 41 (23.6) |
| Amiodarone-dronedarone | 46 (24.4) |
| Combinations | 11 (6.3) |
| None | 56 (32.2) |
| Postablation antithrombotic therapy | |
| No | 40 (23) |
| Antiplatelet agents | 38 (21.8) |
| Oral anticoagulation | 96 (55.2) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


