Our objective was to investigate the course of depression and anxiety symptoms in patients treated with continuous flow (CF) left ventricular assist devices (LVADs). Depression and anxiety are associated with poor outcomes in patients with heart failure, yet few studies have examined such symptoms in patients with CF-LVADs. Depression and anxiety were measured as part of routine clinical care in patients who received a CF-LVAD at our institution from October 2009 to April 2012. Sixty-six patients completed the Patient Health Questionnaire-9, and 48 of 66 patients also completed the Generalized Anxiety Disorder Questionnaire-7. Nineteen of 66 patients completed measures before implantation. Patients who completed measures before and after implantation demonstrated significant improvements in depression and anxiety scores. All patients showed significant improvements in depression and anxiety scores from implantation to the first time point after implantation. Pairwise mean comparisons between time intervals after implantation were not significant. In conclusion, depression and anxiety scores improve after CF-LVAD implantation and remain stable up to 1 year. The improvement does not depend on baseline psychotropic medication use and may be related to improved physical health.
Patients treated with continuous flow (CF) left ventricular assist devices (LVADs) demonstrate improvements in functional capacity and quality of life. However, there is a paucity of studies examining depression and anxiety symptoms in patients treated with CF-LVADs. Only 1 study to date has examined psychological morbidity in the CF-LVAD population, and this has been limited to anxiety related to post–traumatic stress disorder symptoms. Given that depression and anxiety symptoms were significantly correlated with issues specific to pulsatile devices, the extent to which these symptoms would still be present in patients who have CF-LVADs is unclear. Thus, the purpose of this study was to investigate the course of depression and anxiety symptoms in a real-world cohort of ambulatory patients with CF-LVADs.
Methods
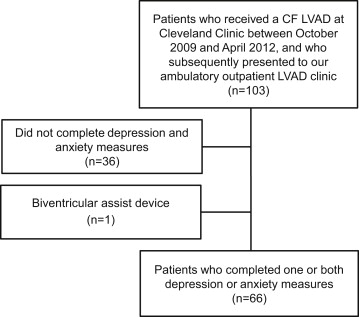
The study protocol was approved by our institutional review board. Patients with heart failure (HF) were included if they received a CF-LVAD at our institution from October 20, 2009 to April 3, 2012 and subsequently presented to our LVAD outpatient clinic ( Figure 1 ) and completed validated questionnaires. These questionnaires were administered electronically using digital tablets at each follow-up visit with no less than 30 days between completion of the same measure. Patients completed the Patient Health Questionnaire-9 (PHQ-9; n = 66), the Generalized Anxiety Disorder Questionnaire-7 (GAD-7; n = 48), or the Kansas City Cardiomyopathy Questionnaire (KCCQ; n = 48) at least once during the study time period. Data for these questionnaires were different because the PHQ-9 was used at our institution before the GAD-7 and KCCQ (November 2010 vs June 2011). More than 75% of patients answered questionnaires ≥2 times after implantation, and 19 patients completed at least 1 of these 3 measures before implantation. These preimplantation data were also used for the present study.
We extracted the following variables from the electronic medical record:
- •
Demographic information: age, gender, race, education, and marital status.
- •
Clinical status: type of cardiomyopathy (ischemic vs nonischemic), history of cardiac surgery (i.e., valve replacement or repair and coronary artery bypass graft surgery), delivery of defibrillator shock within 1 year preoperatively, LVAD device type (HeartMate II (Thoratec; Pleasanton, California) or HVAD (HeartWare; Framingham, Massachusetts)), LVAD strategy (bridge to transplant [BTT] vs destination therapy [DT]), preoperative New York Heart Association class, preoperative left ventricular ejection fraction, date of heart transplantation, and date of death (if applicable).
- •
Clinical variables related to mental health: mood or anxiety disorder diagnosis at implantation, and pre- and post-operative use of psychotropics.
PHQ-9 is a standardized screening tool to assess depression. It has been shown to have acceptable sensitivity and specificity for patients with coronary heart disease and is recommended as a method to screen for depressive symptoms in the HF population. Patients respond to 9 items by answering “not at all,” “several days,” “more than half the days,” and “nearly every day.” A total score can be derived from assigning values of 0, 1, 2, and 3 and adding values for the 9 items. The PHQ-9 uses a categorical algorithm to assess the possibility of a current episode of major or minor depression. Cut-off points of 5, 10, and 15 are used to define mild, moderate, and severe depression (score range 0 to 27). Scores ≥10 are clinically meaningful.
GAD-7 is a 7-item anxiety scale used to screen for anxiety disorders. Psychometric properties for the HF population have not been conducted. However, the GAD-7 has been shown to have high sensitivity and good specificity for diagnosing anxiety in primary care clinics and can be recommended for screening and repeated assessments in these settings. Patients respond to 7 items by indicating “not at all,” “several days,” “more than half the days,” and “nearly every day,” and each response is assigned values of 0, 1, 2, and 3. A total score is calculated with cut-off points of 5, 10, and 15, which define mild, moderate, and severe anxiety symptoms (score range 0 to 21). Scores ≥10 are clinically meaningful.
KCCQ was included to quantify health improvement because it is strongly associated with improved functional capacity (e.g., peak VO 2 and 6-minute walk distance). This 23-item measure has well-documented psychometric properties and assesses the impact of HF on physical functioning, social functioning, self-efficacy, and quality of life. An overall summary score is derived from these domains and was used as the KCCQ outcome variable in our analyses. Scores range from 0 to 100; higher scores reflect fewer symptoms and better quality of life. A 5-point change is clinically meaningful and strongly associated with improved functional capacity.
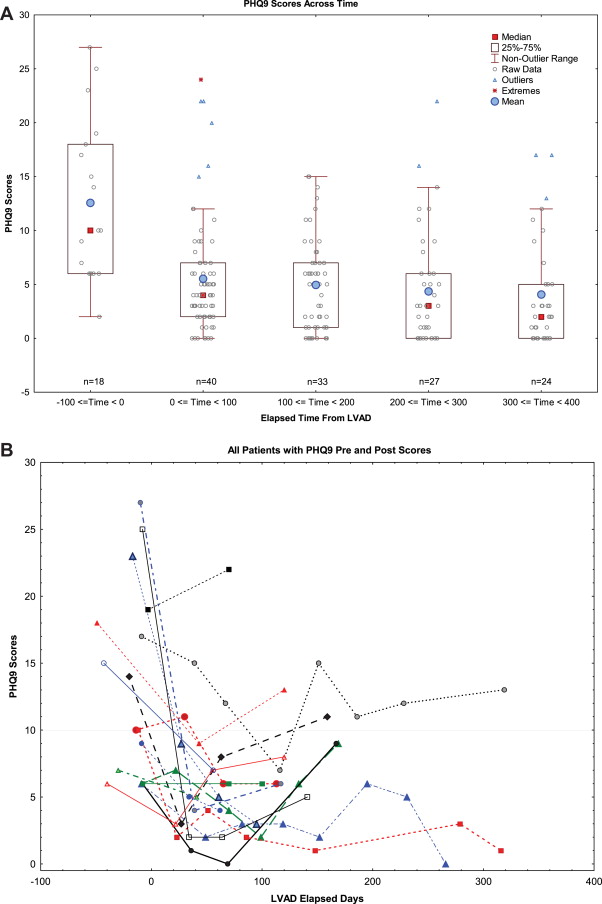
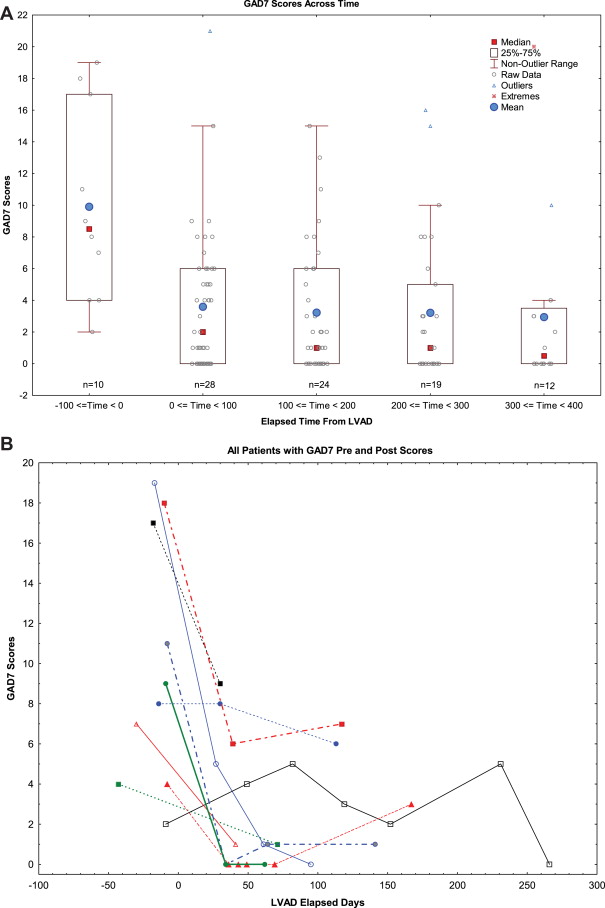
The trending in depression and anxiety scores over time with adjustments for the covariates of patient age, race, gender, defibrillator shock, and LVAD strategy (BTT vs DT) was assessed using backward elimination repeated measure mixed models with an autocorrelation covariance structure for measures within subjects across time. To ensure that the effect of time was not being driven by patients who only had postimplantation measures, the data were analyzed with and without these patients. Time was a significant variable (p <0.05) in the final models for each of the measures regardless of patient sample. Uneven distribution of measurement times within a given patient, as well as across patients, required temporal binning of the data into intervals of 100 days to permit repeated measures analysis and allow pairwise comparisons between time groups. Figures 2 and 3 illustrate this condition for patients with pre- and post-implantation measures. A bin width of 100 days was driven by the distribution of the preimplantation time measurements. All pairwise comparisons were made with Tukey-Kramer adjustments for multiple comparisons.
We performed 2 secondary analyses to examine the relation between the first postimplantation depression and anxiety scores and (1) diagnoses of mood or anxiety at baseline and (2) use of psychotropic medication at baseline. Using mixed models repeated measures regression, we also examined whether depression and anxiety scores correlated with physical functioning or health status (i.e., KCCQ scores).
Results
Patient characteristics are listed in Table 1 . Median follow-up time between CF-LVAD implantation and first postimplantation questionnaire of any type was 54 days (mean 126 ± 126). Depression and anxiety scores over time are shown in Figures 2 and 3 . As noted previously, trending over time was significant with/without patients who did not complete measures before implantation. All patients showed significant improvements in mean depression and anxiety scores after implantation (PHQ-9: 12.1 ± 7.5 to 5.7 ± 5.4, p <0.0001 and GAD-7: 10.4 ± 6.2 to 3.4 ± 4.3, p <0.0001) that remained stable through 1 year. Pairwise mean comparisons between time intervals after implantation were not significant (p ≥0.53). Figures 2 and 3 show patient-level data for the subset of patients (n = 19) who completed measures before and after implantation. Significant improvements in mean depression and anxiety scores (PHQ-9: 12.1 ± 7.5 to 5.6 ± 4.5, p = 0.0002 and GAD-7: 10.4 ± 6.2 to 2.3 ± 3.0, p <0.05) were observed for these patients.
| Characteristics | N = 66 |
|---|---|
| Age (yrs) | 55 (21–79) |
| Men | 57 (86%) |
| White | 50 (78%) |
| Married | 41 (62%) |
| College graduate or graduate school | 11 (17%) |
| High school graduate or some college | 44 (67%) |
| Less than high school | 11 (17%) |
| Ischemic cardiomyopathy | 27 (41%) |
| Prior cardiac surgery | 12 (18%) |
| Charlson Comorbidity Index score | 2.6 ± 1.5 |
| Defibrillator | 62 (94%) |
| History of defibrillator shock within 1 year | 16 (26%) |
| Left ventricular ejection fraction | 17 (5%) |
| Index hospitalization length of stay | 38.4 (9–133) |
| Left ventricular assist device | |
| HeartMate II left ventricular assist device | 59 (89%) |
| HVAD left ventricular assist device | 7 (11%) |
| Destination therapy | 30 (46%) |
| Mental health | |
| Documented depression diagnosis | 12 (18%) |
| Documented anxiety diagnosis | 10 (15%) |
| Antidepressant medication use | 19 (29%) |
| Anxiolytic medication use | 13 (20%) |
| Stimulant medication use | 1 (2%) |
| Sedative or hypnotic medication use | 8 (12%) |
| Atypical antipsychotic medication use | 1 (2%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


