Studies have found that non–high-density lipoprotein cholesterol (non-HDL-C) is a superior marker for coronary heart disease compared to low-density lipoprotein cholesterol (LDL-C). Little is known about achievement of non-HDL-C goals outside clinical trials. Within a population of 146,064 patients with dyslipidemia in the PINNACLE Registry and a subgroup of 36,188 patients with diabetes mellitus (DM), we examined the proportion of patients and patient characteristics associated with having LDL-C, non-HDL-C, and both LDL-C and non-HDL-C levels at National Cholesterol Education Program goals. LDL-C, non-HDL-C, and both LDL-C and non-HDL-C goals in the overall cohort were achieved by 73%, 73.4%, and 68.9% patients, respectively. Significant predictors of meeting all 3 goals were age, male gender, statin, nonstatin, and combined statin plus nonstatin use. Patients with co-morbidities of hypertension, previous stroke or transient ischemic attack, peripheral arterial disease, myocardial infarction, and smoking were less likely to have LDL-C, non-HDL-C, and both LDL-C and non-HDL-C levels at National Cholesterol Education Program goal. In the overall cohort, patients with DM were less likely to meet non-HDL-C and both LDL-C and non-HDL-C goals. In the subgroup of patients with DM, predictors of meeting lipid goals were similar to the overall cohort. In conclusion, these data suggest contemporary treatment patterns by cardiologists successfully achieve lipid goals in most patients. Younger, female patients and those with atherosclerotic cardiovascular disease and risk factors, such as hypertension and DM, are less likely to achieve goals and may require more careful follow-up after statin initiation. Both LDL-C and non-HDL-C goals are achieved in <70% of patients, suggesting room for improvement if a goal-targeted individualized strategy is adopted.
Patients with diabetes mellitus (DM) and insulin resistance often have metabolic syndrome and elevated low-density lipoprotein cholesterol (LDL-C), non–high-density lipoprotein cholesterol (non-HDL-C), apolipoprotein B, and triglycerides. The 2013 American College of Cardiology (ACC)/American Heart Association (AHA) guidelines recommended statin therapy for patients of any age having LDL-C ≥190 mg/dl and those with DM 40 to 75 years of age and LDL-C 70 to 189 mg/dl, regardless of calculated atherosclerotic cardiovascular disease (ASCVD) risk. In their 2014 document, the National Lipid Association considers patients with DM at either high or very high risk for ASCVD and recommend primary LDL-C goals of <100 mg/dl or <70 mg/dl depending on risk with analogous non-HDL-C goals of <130 mg/dl and <100 mg/dL. In addition, the American Diabetes Association 2015 Standards of Medical Care in Diabetes recommend high-intensity statin therapy regardless of baseline lipid levels for patients with DM who have overt cardiovascular disease (CVD). For patients with one or more CVD risk factors (including the risk factor of LDL-C ≥100 mg/dl), the American Diabetes Association recommends moderate- or high-intensity statin therapy for patients aged <40 years, high-intensity statin therapy for patients aged 40 to 75 years, and moderate-intensity statin therapy for patients aged >75 years. For patients with DM and no additional CVD risk factors, no drug therapy is recommended for ages <40 years and a moderate-intensity statin is recommended for ages ≥40 years. No LDL-C treatment targets are recommended in the 2015 guidelines. The 2013 International Atherosclerosis Society guidelines do not address DM specifically but promote non-HDL-C targets corresponding to level of risk estimated by a risk calculators that incorporate DM.
Little is known about LDL-C and non-HDL-C levels achieved in real-world practice in patients within the National Cardiovascular Data Registry (NCDR), Practice INNovation And Clinical Excellence (PINNACLE) Registry. Because there is current controversy in approach to management, the purpose of this analysis was to determine the rates and predictors of LDL-C and non-HDL-C lipid goal attainment as a function of National Cholesterol Education Program (NCEP) Expert Panel risk categories in a population and the subgroup of patient with DM from the PINNACLE Registry, which is the largest outpatient CVD registry in the United States. Targets recommended were those defined by the 2002 Third Report of the NCEP on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults and the 2004 Adult Treatment Panel III update which were applicable during the reference period of our analysis.
Methods
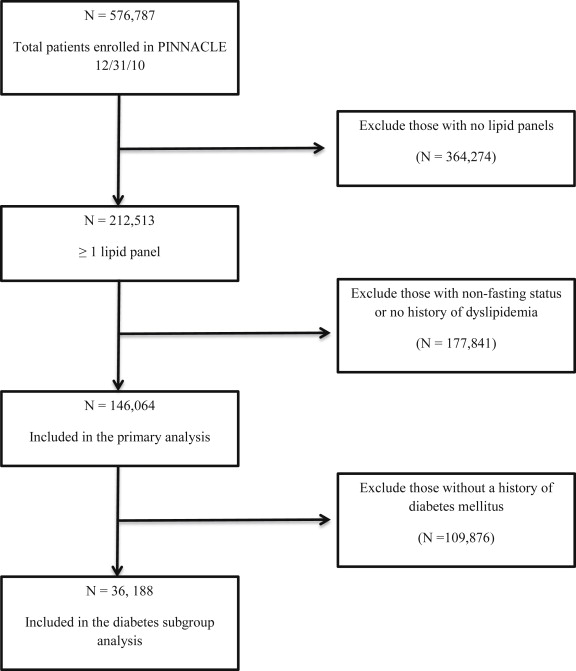
Patients entered into the PINNACLE Registry from July 1, 2008, to December 31, 2010, with at least a history of dyslipidemia and at least 1 lipid panel (or because of low sample size, patients where the fasting status of the lipid panel was missing) were identified ( Figure 1 ). PINNACLE Registry data are collected prospectively from 44 cardiology office practices representing all 5 regions of the United States. Data collected includes patients’ symptoms, vital signs, co-morbidities, selected laboratory tests, medication classes, and health insurance. Data collection is achieved largely through a system capable of directly extracting relevant PINANCLE Registry data from practices’ electronic medical records or through paper forms completed at the time of clinic visits. If there was more than one lipid panel per patient, the first one was used for data analysis.
LDL-C and non-HDL-C goals were determined by standard NCEP definitions using Framingham risk score for 10-year coronary heart disease (CHD) risk. Two separate analyses were performed. One for the overall cohort and one restricted to patients with DM. Three separate hierarchical modified Poisson regression models (SAS version 9.3; SAS Institute, Cary, North Carolina) were subsequently created to identify patient-level factors that were associated with having an LDL-C (≤100 mg/dl), non-HDL-C (≤130 mg/dl), or both levels at NCEP goal in the overall cohort and in those with DM. Patient characteristics included in the model are listed in Table 1 with the exception of race as it had a high frequency of missing data in the PINNACLE Registry. Finally, we analyzed the likelihood of achieving LDL-C, non-HDL-C, and both LDL-C and non-HDL-C levels below NCEP goals using combined statin and nonstatin lipid-lowering therapy versus statin alone.
| Variable | PINNACLE ® Population (study Eligible n=146,064) | PINNACLE ® Population (diabetes subgroup n= 36,188) |
|---|---|---|
| Age (mean ± SD) (Years) | 66.6 ± 12.4 | 67.5 ± 11.0 |
| Men | 58.1 % | 58.5 % |
| Race | ||
| White race | 89.2% | 82.8% |
| Black race | 9.8% | 15.9% |
| Other race | 1.0% | 1.3% |
| Smoker | ||
| Current | 11.2% | 10.1% |
| Never | 47.3% | 45.9% |
| Body mass index ≥ 25 kg/m 2 | 79.1% | 88.1% |
| Hypertension | 81.7% | 91.4% |
| Diabetes mellitus | 24.8% | 100% |
| Coronary artery disease | 65.7% | 73.6% |
| Myocardial infarction | 21.5% | 23.2% |
| Percutaneous coronary intervention within 12 months | 11.4% | 13.0% |
| Prior stroke/transient ischemic attack | 5.1% | 5.8% |
| Peripheral arterial disease | 12.6% | 16.1% |
| LDL-C (mg/dL) | 93.2 ± 38.5 | 84.6 ± 37.1 |
| HDL-C (mg/dL) | 47.4 ± 15.7 | 43.5 ± 14.0 |
| Triglycerides (mg/dL) | 137.2 ± 83.6 | 150.5 ± 92.9 |
| Non-HDL-C (mg/dL) | 120.6 ± 43.6 | 114.7 ± 43.3 |
| Lipid-Lowering Medications | ||
| Any lipid-lowering medication | 80.4% | 86.2% |
| Regimen contains a statin | 75.0% | 80.6% |
| Regimen contains a non-statin | 20.9% | 24.1% |
| Regimen contains both statin and non-statin | 15.5% | 18.5% |
| None | 19.6% | 13.8% |
| ACE inhibitor | 36.7% | 45.9% |
| Angiotensin receptor blocker | 16.6% | 20.9% |
| Clopidogrel or prasugrel | 19.1% | 23.7% |
| Aspirin or aspirin/dipyridamole | 63.6% | 66.2% |
| Beta-blocker | 58.9% | 66.8% |
| Calcium channel blocker | 16.0% | 19.4% |
| Diuretic | 34.6% | 46.0% |
Results
Of 576,787 patients enrolled in the PINNACLE Registry, 146,064 patients (25.3%) had a history of dyslipidemia with at least 1 lipid panel ( Figure 1 ). Of these 146,604 patients, there were 36,188 patients with a history of DM (included in the subgroup analysis). The baseline characteristics of patients in the overall cohort and in the subgroup of patients with DM are described in Table 1 .
In the overall cohort (n = 1,46,604), the mean patient age was 66.6 ± 12.4 years, 58.1% were men and 89.3% were white ( Table 1 ). The prevalence of co-morbidities were DM 24.8%, coronary artery disease (CAD) 65.7%, myocardial infarction (MI) 21.5%, and stroke or transient ischemic attack (TIA) 5.1%. Eighty percent of patients (80.4%) were currently being treated with pharmacotherapy for dyslipidemia and 19.6% of patients with a history of dyslipidemia were prescribed no lipid-lowering pharmacotherapy. In patients taking pharmacotherapy, 75% of regimens contained a statin (59.5% statin monotherapy), 20.9% contained a nonstatin (5.4% nonstatin monotherapy), and 15.5% contained both a statin and nonstatin. In the overall cohort, the mean LDL-C was 93.2 ± 38.5 mg/dl and non-HDL-C 120.6 ± 43.6 mg/dl. Using NCEP goal definitions, LDL-C, non-HDL-C, and both LDL-C and non-HDL-C goals in the overall cohort were achieved by 102,245 (73%), 107,211 (73.4%), and 100,638 (68.9%) patients, respectively.
Table 2 describes variables associated with LDL-C, non-HDL-C, and both non-HDL-C levels at NCEP goals. Older patients were more likely to have LDL-C and non-HDL-C levels at NCEP goals compared to younger patients. Men were more likely than women to have levels at NCEP goals. (Risk ratios and 95% confidence interval [CI] are provided in Table 2 .) Patients with MI and most NCEP CHD risk equivalents (previous stroke or TIA or PAD) were less likely to have LDL-C and non-HDL-C levels at NCEP goals. Although a history of DM was not associated with an LDL-C level at NCEP goal in the overall cohort, it was a significant predictor of having non-HDL-C and of having both an LDL-C and non-HDL C levels at NCEP goals ( Table 2 ). Use of angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, β blockers, and aspirin/aspirin-dypiridamole was each independently associated with a higher likelihood of having LDL-C, HDL-C, and both LDL-C and HDL-C levels at NCEP goals, whereas the use of clopidogrel or prasugrel was associated with a lower likelihood ( Table 2 ). Use of both statin and the use of nonstatins were the best predictors of having LDL-C, non-HDL-C, or both LDL-C and non-HDL-C levels at NCEP goal ( Table 2 ). Patient characteristics in the subgroups of patients with LDL-C, non-HDL-C, and both LDL-C and non-HDL-C levels at NCEP goals versus those with levels higher than NCEP goals are available in Supplementary Table 1 .
| Variable | Risk Ratio LDL-C at NCEP Goal (95% CI) | Risk Ratio Non-HDL-C at NCEP Goal (95% CI) | Risk Ratio Both LDL-C and Non-HDL-C at NCEP Goals (95% CI) |
|---|---|---|---|
| Age (per 5-yr increment) | 1.02 (1.02-1.02 ) a | 1.03 (1.03-1.03) a | 1.03 (1.02-1.03) a |
| Men | 1.08 (1.06-1.09) a | 1.07 (1.05-1.09) a | 1.08 (1.06-1.10 ) a |
| Diabetes mellitus | 0.99 (0.97-1.01) | 0.96 (0.93-0.98) a | 0.96 (0.94-0.99) a |
| Smoker (current) | 0.94 (0.91-0.96) a | 0.96 (0.92-0.94) a | 0.92 (0.90-0.94) b |
| Hypertension | 0.97 (0.95-0.99) b | 0.96 (0.95-0.97) a | 0.96 (0.94-0.98) a |
| Prior stroke/transient ischemic attack | 0.91 (0.87-0.95) a | 0.92 (0.88-0.96) b | 0.90 (0.85-0.95) a |
| Peripheral arterial disease | 0.96 (0.94-0.99) c | 0.97 (0.94-0.99) c | 0.96 (0.94-0.98) a |
| Myocardial infarction | 0.99 (0.97-0.99) d | 0.99 (0.98-0.99) c | 0.98 (0.97-0.99) b |
| Percutaneous coronary intervention (within 12 months) | 0.97 (0.93-1.01) | 0.96 (0.93-0.99) d | 0.96 (0.92-0.99) d |
| Statin | 1.35 (1.26-1.44) a | 1.30 (1.22-1.38) a | 1.40 (1.30-1.51) a |
| Non-statin | 1.24 (1.13-1.36) a | 1.15 (1.04-1.27) b | 1.24 (1.12-1.39) a |
| Both statin and non-statin | 1.44 (1.36-1.53) a | 1.33 (1.26-1.41) a | 1.46 (1.36-1.57) a |
| ACE inhibitor | 1.01 (1.00-1.02) c | 1.01 (1.01-1.02) a | 1.01 (1.01-1.02) c |
| Angiotensin receptor blocker | 1.03 (1.02-1.04) b | 1.03 (1.02-1.04) a | 1.03 (1.02-1.05) a |
| Clopidogrel or prasugrel | 0.99 (0.98-0.99) d | 0.98 (0.98-0.99) c | 0.98 (0.97-0.99) c |
| Aspirin or aspirin/dipyridamole | 1.01 (0.99-1.02) | 1.02 (1.01-1.03) a | 1.02 (1.01-1.03) b |
| Beta-blocker | 1.03 (1.02-1.04) a | 1.01 (1.01-1.02) a | 1.03 (1.02-1.04) a |
| Calcium channel blocker | 1.01 (0.99-1.02) | 1.01 (1.01-1.02) b | 1.01 (1.00-1.03) d |
| Diuretic | 1.02 (1.01-1.03) a | 1.00 (0.99-1.01) | 1.01 (1.00-1.01) |
We also compared LDL-C, non-HDL-C, and combined LDL-C and non-HDL-C levels in our cohort in patients prescribed statin therapy versus those on combination lipid-lowering therapy. Compared to the use of statin alone, combination therapy was associated with a greater likelihood of having an LDL-C level at NCEP goal (risk ratio 1.07, 95% CI 1.04 to 1.09) and both LDL-C and non-HDL-C levels at NCEP goals (risk ratio 1.04, 95% CI 1.01 to 1.08) but was not associated with a greater likelihood of having a non-HDL-C level at NCEP goal (risk ratio 1.03, 95% CI 0.99 to 1.06; data not shown.)
In the subgroup of patients with DM, the mean patient age was 67.5 ± 11.0 years, 58.5% were men and 82.8% were white ( Table 1 ). The prevalence rates of co-morbidities were CAD 73.6%, MI 23.2%, PAD 16.1%, and stroke/TIA 5.8%. More than 3/4 of the patients (80.6%) were being treated with a statin (62.1% statin monotherapy, 5.6% nonstatin monotherapy, and 18.5% statin and nonstatin), whereas 13.8% had no pharmacotherapy for dyslipidemia documented. The mean LDL-C was 84.6 ± 37.1 mg/dl, HDL-C 43.5 ± 14.0 mg/dl, triglycerides 150.5 ± 92.9 mg/dl, and non-HDL-C 114.7 ± 43.3 mg/dl. Using NCEP goal definitions, LDL-C, non-HDL-C, and both goals were achieved by 26,743 (73.9%), 26,055 (72.0%), and 24,717 (68.3%) patients with DM, respectively.
As described in Table 3 , older patients were more likely (risk ratio per 5 years 1.04, 95% CI 1.04 to 1.05), and men more likely (risk ratio 1.13, 95% CI 1.12 to 1.15) to achieve non-HDL-C goals. With the exception of MI as a predictor of non-HDL-C levels, the presence of ASCVD did not impact likelihood of achieving either LDL-C, non-HDL-C, or both goals. (Risk ratios and 95% CIs are provided in Table 3 .) The use of statins, nonstatin lipid-lowering agents, and their combination were the best independent predictors of achieving goals ( Table 3 ). As found in the main analysis, the use of angiotensin-converting enzyme inhibitors, β blockers, and aspirin/aspirin-dypiridamole was each independently associated with a higher likelihood of having LDL-C, HDL-C, and both LDL-C and HDL-C levels at NCEP goals, whereas the use of clopidogrel or prasugrel was associated with a lower likelihood ( Table 3 ). Patient characteristics in the subgroups of patients with LDL-C, non-HDL-C, and both LDL-C and non-HDL-C levels at NCEP goals compared to those with levels higher than NCEP goals are available in Supplementary Table 2 .



