CHAPTER
7
Focal Atrial Tachyarrhythmia
UNDERSTANDING AND MANAGING FOCAL ATRIAL TACHYCARDIA
Epidemiology and Clinical Features
Focal atrial tachyarrhythmia (FAT) is observed in 0.3-0.4% of the asymptomatic population and 0.4-0.5% of the symptomatic population. It can present as:
○Paroxysmal tachycardia
○Persistent tachycardia with palpitations, chest pain, fatigue, dyspnea, or effort intolerance
▪ If rapid rates persist, then heart failure may result (tachycardia-induced cardiomyopathy).
○Syncope is rare, but it can occur with rapid tachycardia and 1:1 conduction.
○“Silent” atrial tachycardia is detected in asymptomatic patients on electrocardiogram (ECG), Holter, or implantable devices.
Anatomy and Pathophysiology (Mechanism)
○Basic mechanism is an impulse originating from a right (80%; crista terminalis; superior vena cava [SVC]; inferior vena cava [IVC]) or left (20%; pulmonary vein, atrial septum, mitral annulus) atrial focus.
○Sub-classified based on mechanism
▪ Abnormal automaticity (i.e., automatic ectopic atrial tachycardia [AEAT])
▪ Triggered activity (i.e., non-automatic focal atrial tachycardia [NAFAT])
▪ Localized (micro) reentry
Etiology
○Pulmonary disease: Chronic obstructive pulmonary disease (COPD), pulmonary hypertension, or chronic hypoxia
○Hyper-adrenergic states: Myocardial ischemia or infarction
○Metabolic or electrolyte: Hypokalemia/hypomagnesemia
○Drugs: Digoxin, theophylline
○Cardiothoracic surgery (especially for congenital heart disease)
Classification
○ Benign atrial tachyarrhythmia
▪ Paroxysmal, regular, narrow-complex tachyarrhythmia at 80–140 bpm
○ Incessant atrial tachyarrhythmia
▪ Persistent/permanent, regular, narrow-complex tachyarrhythmia at 100–160 bpm
○ Focal atrial tachycardia with an AV block
▪ Regular atrial tachyarrhythmia with variable ventricular rate
▪ Typically this is seen with digoxin toxicity, which has parasympathetic (inhibitory) effects on sinoatrial (SA node) and atrialventricular nodes (AVN) but sympathetic (stimulatory) effects on pacemaker cells (increased automaticity).
○ Multifocal atrial tachycardia
▪ Irregular tachyarrhythmia (100–250 bpm) because of simultaneous activation of multiple (>3) foci
• Most often enhanced automaticity is seen during an acute medical illness (typically pulmonary disease).
▪ A wandering atrial pacemaker is similar to multifocal atrial tachycardia except for the heart rate <100.
○ Junctional tachycardia (JT)
▪ Persistent/permanent tachyarrhythmia because of enhanced automaticity or triggered activity originating at the junction between AVN and His bundle
▪ Classification
• Focal junctional tachycardia: A heart rate of 110–250 bpm is usually due to trauma, infiltrative hemorrhage, inflammation, or pediatrics.
• Non-paroxysmal junctional tachycardia: The heart rate of 70–120 bpm is usually a marker for significant pathology (e.g., digitalis toxicity, ischemia, myocarditis).
12-Lead ECG
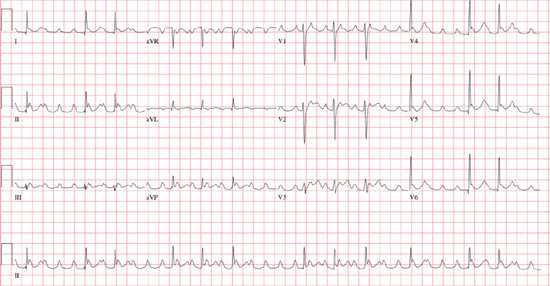
○ Rate: Atrial rate of 100–250 bpm
○ Rhythm: Ventricular conduction is variable:
▪ Regular (constant ventricular conduction): Usually 1:1, 2:1, or 4:1 AV association
• Odd conduction ratios (e.g., 3:1) are rare.
▪ Regularly irregular (dual-level AV block; i.e., 6:2)
▪ Irregularly irregular (variable AV conduction)
• Variable AV block may be confused with irregular ventricular rhythm for atrial fibrillation.
○ P wave: Ectopic, unifocal P′ waves differ from the sinus node P wave.
▪ FAT: Discrete P waves separated by isoelectric baseline in all leads
▪ MAT: Multiple (≥3) different discrete P-wave morphologies with no dominant pacemaker
Table 7.1 ECG Features to Localize the Site of Origin of an Atrial Tachycardia
| Right Atrium V1: Negative P wave (Spec 100%) aVL: Positive or biphasic (Spec 76%) | Left Atrium V1: Positive (Spec 90%) aVL: Negative P wave (usually) | |
High II, III, aVF – positive | SVC • Large P wave mimicking P pulmonale Crista Terminalis • P wave resembles sinus • P is negative in aVR (Spec. 93%) | Superior PVs • Amplitude in lead II is ≥0.1 mV (Sp. 74%) • P wave is larger in ectopy than sinus (lead II; Sp. 85%) Left-sided PVs • Notching in lead II (only during ectopy; Spec. 95%) • P-wave ratio in lead III:II ≥0.8 (Spec. 75%) • V1 positive phase ≥80 ms (Spec. 73%) Right-sided PVs • Positive P wave in aVL (Spec. 100%) • P-wave amplitude in lead I ≥50 mcV (Spec. 99%) |
Low II, III, aVF – negative | Inferolateral • Positive P wave in V5–V6 Inferomedial • Negative P wave in V5–V6 Apex of Triangle of Koch or Septal • P–wave duration is shorter than sinus |
○ PR interval: Isoelectric PR interval with long RP (period of absent atrial activation)
○ QRS: Narrow complex unless it is an aberrancy or bundle branch block (BBB)
○ Onset/termination: Paroxysmal or non-paroxysmal
▪ May exhibit a rate increase (“warm-up”) at onset or a decrease (“cool down”) at termination
○ Maneuvers: Carotid sinus massage or adenosine usually increases the degree of AV block and facilitates the identification of P waves. Adenosine may rarely terminate the tachycardia.
Other Investigations
○ Laboratory investigations
▪ Investigations into underlying cause (see Etiology)
○ 24-hour Holter monitor
▪ Useful for diagnosis with episodes occurring more frequent than weekly
○ Event recorder
▪ Useful for diagnosis with symptomatic episodes occurring weekly to monthly
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


