A 62-year-old man with a history of 2 previous cardiac catheterizations presented with an itchy, nontender skin lesion over his right scapula. The skin lesion had been present for >5 years. Review of the medical records found evidence of a prolonged and complicated cardiac catheterization 8 years previously. Physical examination revealed an 8 × 6 cm, well-demarcated, erythematous reticulated atrophic plaque with telangiectasias and ulceration. Biopsy confirmed histologic changes consistent with radiation dermatitis. In conclusion, the characteristic histologic findings of radiation dermatitis, along with the location over the right scapula and the history of prolonged fluoroscopic exposure during cardiac catheterization, led to the clinical diagnosis of fluoroscopy-induced chronic radiation dermatitis.
The advent of therapeutic interventions such as atrial fibrillation ablation, biventricular pacing, and even complex coronary intervention has resulted in increased radiation exposure in the catheterization laboratory. Skin exposed to fluoroscopy can be injured by the radiation and is often the tissue most at risk because it receives the highest dose. We present a case of a patient found to have fluoroscopy-induced chronic radiation dermatitis and review the current research surrounding the diagnosis and management of these patients.
Case Description
A 62-year-old man presented with a history of an itchy, nontender skin lesion over his right scapula, which he reported had been present for >5 years. His medical history included hypertension, hyperlipidemia, heart failure, coronary artery disease, and extensive smoking. He reported no history of excessive sun exposure or radiation therapy. The patient had 2 cardiac catheterizations with stent placement 8 and 9 years before presentation. Later review of his medical records revealed that the patient’s second cardiac catheterization involved stent breakage in the ostial right coronary artery requiring prolonged fluoroscopic exposure to retrieve the broken stent. The total fluoroscopy time and total dose of radiation delivered during the catheterization are unknown; there were no reporting requirements for total grays at that time.
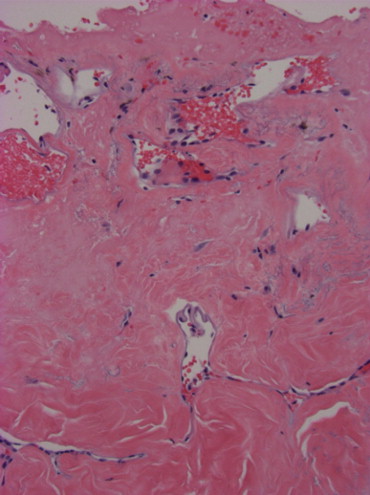
On physical examination, the lesion was an 8 × 6 cm, well-demarcated, erythematous reticulated atrophic plaque with telangiectasias and ulceration located over the right scapula ( Figure 1 ). Histopathology of the lesion demonstrated dilated superficial vessels; thickened, sclerotic collagen bundles with loss of adnexal structures; and sparsely scattered atypical fibroblasts ( Figure 2 ). These findings were consistent with radiation dermatitis. The patient’s history of prolonged fluoroscopic exposure during cardiac catheterization combined with the location of the lesion and the characteristic histologic findings of radiation dermatitis led to the clinical diagnosis of fluoroscopy-induced chronic radiation dermatitis. Since presentation to clinic, the patient has been followed regularly for skin cancer screening and symptomatic management of his lesion.

Comments
Radiation dermatitis is well documented and common, occurring in about 90% of patients receiving radiotherapy for cancer. Fluoroscopy-induced radiation dermatitis is uncommon, because radiation doses delivered during fluoroscopic procedures are typically low and do not reach the threshold needed for skin injury. Radiation dermatitis can develop after fluoroscopy-guided interventional procedures such as coronary angiography, percutaneous transluminal coronary angioplasty, and radiofrequency cardiac catheter ablation. The location of skin injury correlates with the site of radiation beam entry and varies depending on the procedure. Radiation dermatitis from coronary procedures is commonly found on the midback, scapular areas, right anterolateral chest, and below the right axilla.
Clinical presentation of fluoroscopy-induced radiation dermatitis can vary from early reactions of erythema, epilation, and dermal atrophy to chronic changes such as telangiectasia, ulceration, and necrosis. Signs of acute radiation dermatitis are usually present but are not necessary for the development of chronic radiation dermatitis. Histologic features characteristic of radiation dermatitis include epidermal atrophy, dermal sclerosis, dilated superficial blood vessels, and atypical stellate fibroblasts. Fluoroscopy-induced radiation dermatitis is diagnosed by correlating the patient’s history of a fluoroscopy-guided procedure with the location of the skin lesion and the characteristic histologic findings. A biopsy is generally not recommended for chronic radiation dermatitis if the history and clinical presentation are classic given poor wound healing of skin damaged by radiation.
Treatment options for radiation dermatitis consist mostly of symptomatic management and monitoring for progression of the lesion. There is currently no definitive treatment for radiation dermatitis. Review of the existing therapies demonstrates that topical corticosteroids, such as mometasone furoate and beclomethasone dipropionate, reduce skin reactions after radiation. Evidence for the use of topical nonsteroidal creams is conflicting and does not show a clear benefit. Surgical excision and skin grafting may be required for severe injuries, such as nonhealing ulcers.
Malignant transformation of the skin into squamous cell carcinoma in the area exposed to ionizing radiation has been documented. There have been reports of superficial basal cell carcinomas developing 20 to 30 years after multiple diagnostic fluoroscopic procedures in patients exposed to large cumulative doses of ionizing radiation. Cancer is an example of a stochastic effect of radiation. Stochastic effects lack a threshold dose required for injury, whereas deterministic effects of radiation are injuries to the skin and subcutaneous tissues that occur once a threshold dose is exceeded.
Patients who undergo fluoroscopy-guided procedures should be made aware of the possibility of radiation dermatitis, especially if they will be exposed to >4 Gy. In most patients, the threshold dose for clinically significant skin and hair changes is 5 Gy. If a patient received an estimated total radiation dose >10 Gy, medical follow-up is appropriate. After fluoroscopic procedures, patients should be advised to monitor for any skin changes in the area exposed under fluoroscopy and should receive direct skin evaluation if exposed to higher doses.
Fluoroscopic procedures are increasing in younger patients, particularly radiofrequency cardiac catheter ablation as a treatment for atrial fibrillation, many of whom require ≥2 procedures. Physicians must know thresholds of exposure mandating follow-up and published guidelines for reducing exposure. As outlined in a recent publication by the American College of Cardiology Foundation and the Society for Cardiovascular Angiography and Interventions, cardiac catheterization reports must include fluoroscopy time and radiation dose as minimum requirements, and patients should be informed if they received significant exposure. Because there is no definitive treatment for fluoroscopy-induced radiation dermatitis, prevention is critical to reducing injuries. Radiation dermatitis should be considered in any patient at late follow-up presenting with a well-demarcated, atrophic, telangiectatic ulcerated lesion arising in an area exposed to substantial fluoroscopy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


