Although transcatheter aortic valve implantation (TAVI) for severe aortic stenosis is becoming an established technique, the impact of gender-related differences remains unclear. Two hundred twenty-four consecutive patients undergoing TAVI were prospectively followed up in a tertiary medical center. The primary end point of the present study was all-cause mortality at 2 years of follow-up. Interaction-term analysis was used to identify gender-specific predictors of mortality after TAVI. Fifty-seven percent of the study patients were women. Age was similar (82 ± 7 years). Compared with men, women had a lower frequency of coronary artery disease (CAD) and a higher baseline left ventricular ejection fraction (LVEF). The cumulative probability of all-cause mortality was significantly lower among women (8.6%) compared with men (26.8%; log-rank p value <0.001). A lower baseline LVEF (<45%) was associated with a significant, more than fourfold (p = 0.0019 and 0.048, respectively), increase in mortality risk among both men and women (p value for gender-by-LVEF interaction = 0.87). In contrast, the risk associated with the presence of previous CAD was shown to be gender related. Thus, in women, CAD was associated with a pronounced >14-fold increase in mortality risk, whereas in men, CAD was not associated with a significant mortality risk (p value for gender-by-LVEF interaction = 0.01). In conclusion, our findings suggest that risk assessment before TAVI should consider gender-specific differences in survival and risk factors.
The aim of the present study was to perform a gender-based comparison of survival in high-risk patients with severe aortic stenosis (AS) undergoing transcatheter aortic valve implantation (TAVI) in a tertiary referral center in Israel with either the balloon-expandable Edwards SAPIEN or SAPIEN XT (Edwards Lifesciences) or the self-expandable CoreValve (Medtronic) prosthesis, and to identify predictors of mortality in men and women undergoing TAVI.
Methods
From September 2008 to January 2013, a total of 224 consecutive patients with severe AS were treated by TAVI either with CoreValve or Edwards valves at our institution. These patients were included prospectively in a dedicated database that included data regarding baseline clinical factors and medications, procedural characteristics and complications, and mortality at 2 years of follow-up.
The primary end point of the present study was all-cause mortality at 2 years of follow-up. Mortality events were collected from hospital records and ascertained from the Israeli National Register.
The presence of coronary artery disease (CAD) before the TAVI procedure was defined as ≥1 of the following: previous myocardial infarction, previous revascularization (coronary artery bypass graft or percutaneous coronary intervention), or presence of significant obstructive CAD before the procedure requiring intervention.
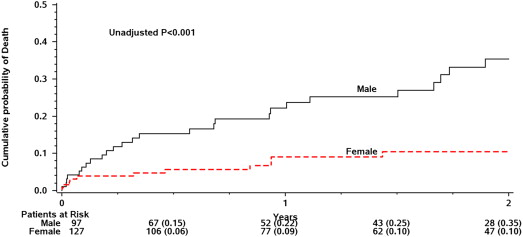
Continuous variables are reported as the mean ± SD or median and interquartile range, and comparisons between groups were performed with Student t or Mann-Whitney U tests, as appropriate. Categorical variables are reported as counts and percentages and were compared by chi-square test or Fisher’s exact test, as appropriate. The cumulative probability of all-cause mortality during follow-up was estimated with the Kaplan-Meier method, and comparisons by gender and risk factors were assessed using the log-rank test.
Multivariate analysis for the primary end point of all-cause mortality was carried out using Cox proportional hazards regression modeling. Covariates independently associated with mortality were identified using a best subset analysis, with candidate covariates listed in Table 1 . The effect of clinical factors on mortality in men and women was evaluated by adding a gender-by-covariate interaction term to the multivariate model. To avoid a possible confounding effect of age on mortality, age was forced in to all multivariate models.
| Variable | All (n = 224) | Men (n = 97) | Women (n = 127) | p Value |
|---|---|---|---|---|
| Age (yrs) | 82 ± 7 | 81 ± 8 | 82 ± 6 | 0.82 |
| Age >80 yrs | 65 | 64 | 66 | 0.73 |
| EuroSCORE | 28 ± 15 | 31 ± 16 | 27 ± 14 | 0.09 |
| High EuroSCORE (>20) | 64 | 67 | 63 | 0.65 |
| Previous coronary artery bypass graft | 27 | 41 | 17 | <0.001 |
| CAD | 51 | 69 | 38 | <0.001 |
| Chronic obstructive pulmonary disease | 37 | 39 | 35 | 0.50 |
| Diabetes mellitus | 34 | 36 | 32 | 0.6 |
| Peripheral vascular disease | 11 | 15 | 8 | 0.14 |
| Chronic kidney disease | 79 | 76 | 81 | 0.47 |
| Body mass index (kg/m 2 ) | 27 ± 4 | 27 ± 4 | 27 ± 5 | 0.65 |
| Body mass index >30 kg/m 2 | 27 | 22 | 31 | 0.19 |
| Glomerular filtration rate (ml/min) | 46 ± 19 | 47 ± 20 | 46 ± 18 | 0.43 |
| High New York Heart Association class (>II) | 99 | 100 | 99 | 1 |
| LVEF (%) | 54 ± 13 | 49 ± 14 | 58 ± 10 | <0.001 |
| LVEF <45% | 23 | 40 | 12 | <0.001 |
| Aortic valve area (cm 2 ) | 0.7 ± 0.2 | 0.7 ± 0.2 | 0.7 ± 0.2 | 0.29 |
| Aortic valve pressure gradient max (mm Hg) | 77 ± 24 | 71 ± 22 | 81 ± 25 | 0.02 |
| Aortic valve pressure gradient mean (mm Hg) | 48 ± 17 | 44 ± 15 | 51 ± 17 | 0.02 |
| Pulmonary artery pressure (mm Hg) | 48 ± 15 | 50 ± 16 | 46 ± 14 | 0.15 |
| Pulmonary artery pressure >60 mm Hg | 21 | 27 | 16 | 0.07 |
| Aortic annulus diameter (mm) | 20 ± 7 | 21 ± 8 | 20 ± 6 | 0.001 |
The statistical software used for the analyses was SAS, version 9.2 (SAS Institute, Cary, North Carolina). A 2-sided p value <0.05 was used for declaring statistical significance.
Results
Of the 224 enrolled patients, 127 were women (57%) and 97 were men (43%). Their mean age was 82 years (median 83, interquartile range 79 to 86).
The baseline clinical characteristics of study patients by gender are presented in Table 1 . Men and women displayed a similar age and rate of associated co-morbidities, including diabetes mellitus, renal failure, chronic obstructive pulmonary disease, and heart failure functional class. Accordingly, the EuroSCORE before the procedure was not significantly different between the 2 groups. However, women had a significantly lower frequency of CAD, and previous coronary artery bypass graft surgery compared with men. When echocardiographic parameters were compared, women were shown to have a significantly higher baseline left ventricular ejection fraction (LVEF), increased mean gradients across the aortic valve, and a smaller aortic root annulus diameter.
The procedural characteristics are presented in Table 2 . The CoreValve device was used in the majority of the whole cohort but was used less frequently in women than in men, whereas the transfemoral access was used more often in women than in men.
| Variable | All (n = 224) | Men (n = 97) | Women (n = 127) | p Value |
|---|---|---|---|---|
| CoreValve | 70 | 82 | 61 | <0.001 |
| Edwards | 30 | 18 | 39 | <0.001 |
| TF access | 93 | 90 | 95 | 0.01 |
There were no significant differences in the 30-day procedural outcome between men and women, except for acute kidney injury, which was more prevalent in men ( Table 3 ).
| 30-Day Procedural Outcome | Men | Women | p Value |
|---|---|---|---|
| All-cause mortality | 5 | 4 | 0.45 |
| Clinically relevant bleeding | 11 | 8 | 0.32 |
| Acute kidney Injury † | 26 | 14 | 0.04 |
| New pacemaker | 20 | 14 | 0.15 |
∗ Data regarding 30-day procedural outcomes were available for 176 study patients (79%).
† Acute Kidney Injury was defined based on the Acute Kidney Injury Network classification as any increase in serum creatinine to 150% to 199% (1.5 to 1.99 × increase compared with baseline) or increase of >0.3 mg/dl.
The mean follow-up period in this cohort was 17 months, interquartile range 7 to 27.
Kaplan-Meier survival analysis showed that at 2 years of follow-up the cumulative probability of all-cause mortality was significantly lower among women (8.6%) compared with men (26.8%; log-rank p value for the overall difference during follow-up <0.001; Figure 1 ). Consistent with these findings, multivariate Cox proportional hazards regression modeling ( Table 4 ) demonstrated that men had a 2.5-fold increased risk for death during 2 years of follow-up after the TAVI procedure compared with women. In addition, lower baseline ejection fraction (<45%) was shown to be associated with a fourfold increased mortality risk. Additional clinical and echocardiographic factors (listed in Table 1 ) were not shown to be independently associated with a statistically significant increase in mortality risk during follow-up after adjustment for gender and baseline LVEF. Notably, similar results regarding increased risk among men were observed in a secondary analysis that included further adjustment for procedural data (data not shown).