Extracranial Carotid and Vertebral Artery Disease
Pranav M. Patel MD, FSCAI
Extracranial carotid and vertebral artery disease (ECVD) can encompass several disorders that affect the arteries that supply the brain. These include atherosclerosis, fibromuscular dysplasia (FMD), cystic medial necrosis, arteritis, and artery dissection. ECVD is an important cause of stroke and transient cerebral ischemic attack (TIA), and accounts for up to 15% to 20% of all ischemic strokes depending on the population studied (1). The most frequent cause is atherosclerosis.
Atherosclerosis is a systemic disease, and patients with ECVD frequently have atherosclerosis within the aorta, coronary arteries, and peripheral arteries. Patients with ECVD are at increased risk of myocardial infarction (MI) and death, secondary to cardiac disease. Patients with carotid artery stenosis have an increased risk of death caused by MI than of stroke. To improve survival, neurological status, and quality of life, these patients should receive preventive and therapeutic treatments to address both cerebral and systemic risks of atherosclerosis. Coronary atherosclerosis is common in patients with fatal stroke and occurs more frequently in individuals with carotid or vertebral artery atherosclerosis.
EPIDEMIOLOGY
Stroke is the third leading cause of death and the leading cause of long-term disability in industrialized countries (2). Population studies of stroke, including data from the Greater Cincinnati/Northern Kentucky Stroke Study suggest an annual incidence of ˜700,000 stroke events, of which ˜500,000 are new and 200,000 are recurrent strokes. Approximately 30% of patients die within the first year of having a stroke and another 50% are left disabled (3). Current data suggest that ˜88% of all strokes are ischemic, 9% are intracerebral hemorrhages, and 3% are subarachnoid hemorrhages (4, 5, 6).
Extracranial carotid disease (carotid stenosis) accounts for at least 50% of ischemic strokes, and should be managed efficiently to minimize the incidence of stroke. Unfortunately, only about 15% of strokes are preceded by transient ischemic attacks (7). Stroke and TIA may arise as a consequence of several mechanisms that originate in the extracranial cerebral arteries, including:
Artery-to-artery thromboembolism
Embolism of cholesterol material or other atheromatous debris (e.g., Hollenhorst plaque)
Acute thrombotic occlusion of an extracranial artery from plaque rupture
Arterial wall damage from dissection or subintimal hematoma
Reduced cerebral blood perfusion from significant stenosis or occlusion caused by plaque enlargement
ANATOMY
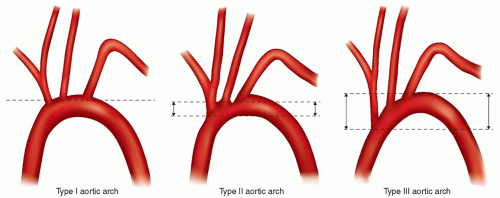
The aortic arch and cervical arteries are subject to many variations. The morphology of the aortic arc can be determined by using the relationship of the brachiocephalic (innominate) artery to the aortic arch. The aortic arch can be classified into three types based on the distance of the origin of the great vessels from the top of the arch. The widest diameter of the left common carotid is used as a reference vessel. In a type I arch, all great vessels originate within one diameter length (diameter length of the widest portion of the left common carotid) from the top of the arch; in a type II arch, all great vessels originate within two diameter lengths from the top of the arch; and in a type III arch, the great vessels originate more than two diameter lengths from the top of the arch (Fig. 36-1). In addition, a segment of the population has the left carotid artery
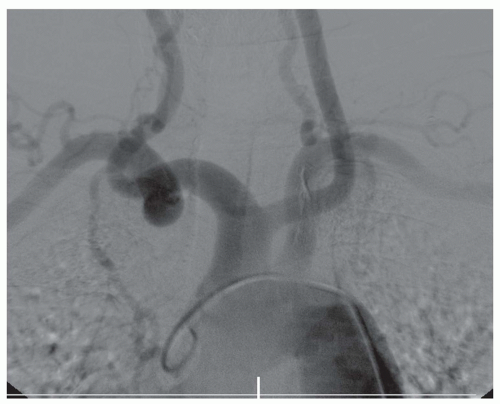
originating from the innominate artery (Fig. 36-2). This is known as a “bovine arch.” Most commonly, the brachiocephalic artery, left common carotid artery, and left subclavian artery originate separately from the aortic arch.
originating from the innominate artery (Fig. 36-2). This is known as a “bovine arch.” Most commonly, the brachiocephalic artery, left common carotid artery, and left subclavian artery originate separately from the aortic arch.
EVALUATION OF ASYMPTOMATIC PATIENTS WITH CAROTID ARTERY DISEASE
Extracranial atherosclerotic disease accounts for up to 15% to 20% of all ischemic strokes (1). There is correlation between the degree of stenosis and the risk of stroke according to the North American Symptomatic Carotid Endarterectomy Trial (NASCET). However, the relationship between stroke risk and severity of stenosis in asymptomatic patients was less clear in other studies (8, 9). In Asymptomatic Carotid Atherosclerosis Study (ACAS) and Asymptomatic Carotid Surgery Trial (ACST), asymptomatic patients with 60% to 80% stenosis had higher stroke rates than those with more severe stenosis (10, 11, 12).
The American College of Cardiology Foundation (ACCF), American Stoke Association (ASA), American Heart Association (AHA), and other organizations recommend that asymptomatic patients with known or suspected carotid stenosis should be evaluated by a duplex ultrasonography (13). This study should be performed by a qualified technologist in a certified facility (Class I, Level of Evidence: C).
Currently no screening program aimed at identifying people with asymptomatic carotid stenosis has been shown to reduce their risk of stroke. The ACCF/AHA, therefore, also recommends that certain individuals will NOT benefit from further evaluations. This includes the following:
Carotid duplex ultrasonography is not recommended for routine screening of asymptomatic patients who have no clinical manifestations of or risk factors for atherosclerosis. (Class III, Level of Evidence: C)
Carotid duplex ultrasonography is not recommended for routine evaluation of patients with neurological or psychiatric disorders unrelated to focal cerebral ischemia, such as brain tumors, familial or degenerative cerebral or motor neuron disorders, infectious and inflammatory conditions affecting the brain, psychiatric disorders, or epilepsy. (Class III, Level of Evidence: C)
Routine serial imaging of the extracranial carotid arteries is not recommended for patients who have no risk factors for development of atherosclerotic carotid disease and no disease evident on initial vascular testing. (Class III, Level of Evidence: C)
DIAGNOSIS
Carotid ultrasonography, computerized tomography angiography (CTA), and magnetic resonance angiography (MRA) can provide the imaging modalities to help diagnose and treat extracranial carotid artery stenosis. The severity of stenosis is defined according to angiographic criteria by the method used in NASCET (Fig. 36-3). This method corresponds as well to assessment by ultrasound (US), CTA and MRA. Catheter-based angiography may be necessary in cases for definitive diagnosis when noninvasive imaging findings are inconclusive. This type of angiography, however, also carries risks of vessel dissection and plaque embolization, although these risks tend to be very low.
Carotid ultrasound also has a high accuracy for carotid restenosis after endarterectomy. Numerous criteria (14, 15) have been proposed to diagnose severe carotid stenosis. In most cases, >80% stenosis correlates with systolic velocity >300 to 400 cm/s, diastolic velocity >100 to 135 cm/s and ratio of internal carotid artery/common carotid artery (ICA/CCA) systolic velocity of >3.5. Other factors such as contralateral occlusion diminished cardiac output from severe left ventricular dysfunction, aortic stenosis, and common carotid artery stenosis may make these measurements less reliable.
Digital cineangiography remains the gold standard with which other methods of vascular imaging are compared in patients with ECVD. The NASCET method for measuring stenosis in the internal carotid arteries has been used in most modern clinical trials.
Aortic Arch Angiography
Aortic arch angiography becomes very important when considering carotid and vertebral artery intervention. The origin of the great vessel is best visualized in the left anterior oblique (LAO) position. In most cases, selective angiography of the great vessels should not be completed without first performing nonselective angiogram of the aortic arch. Arch angiography is usually performed with a pigtail catheter. The image intensifier is positioned in an LAO position until no foreshortening of the catheter is visible. This occurs when the intensifier is perpendicular to the arch. The arch angiogram can then be followed by selective vertebral and carotid artery angiograms.
Carotid and Vertebral Artery Angiography
Catheters of various shapes are available for carotid artery and vertebral angiography. The catheters can be divided into three groups: passive, intermediate, and active catheters. Use of a particular category of catheter will depend on the shape of the aortic arch and takeoff of the great vessels. Elongation of aorta with aging and atherosclerosis along with different anatomy of the chest cavity gives rise to tortuosity of the arch vessels. This may also alters relationship of their origins to descending aorta. It is very important to recognize these changes as they determine accessibility of these vessels for percutaneous interventions. The aortic
arch can be classified into three types based on the distance of the origin of the great vessels from the top of the arch, and may require different types of catheters for selective cannulation of the great vessels.
arch can be classified into three types based on the distance of the origin of the great vessels from the top of the arch, and may require different types of catheters for selective cannulation of the great vessels.
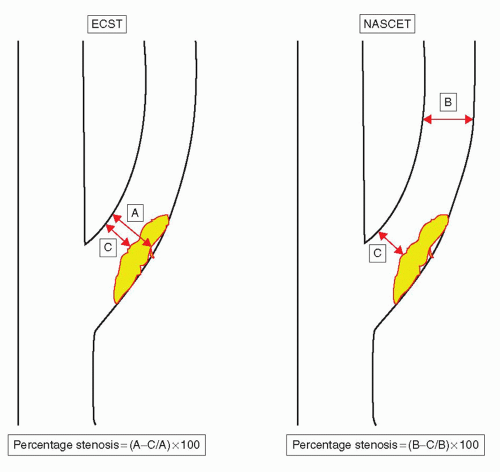 FIGURE 36-3 Angiographic methods for determining carotid stenosis severity. ECST, European Carotid Surgery Trial; NASCET, North American Symptomatic Carotid Endarterectomy Trial. |
Passive catheters such as headhunter, multipurpose, and vertebral are used to access the great vessels in patients with type I aortic arch. Intermediate catheters include the Vitek (Cook Incorporated, Bloomington, IN), Bentson (JB 1-3; Cordis, Miami Lakes, FL). These catheters will require more manipulation than the passive catheters, and are ideal for type II aortic arches. Active catheters such as the Simmons sidewinder (Cook, Inc., Bloomington, IN) and Newton (Cordis Corp, Miami, FL) may require more maneuvers to get into the preformed shape in order to facilitate access into type II or type III arches.
Active catheters must be shaped in the ascending aorta and, therefore, can be a source of artheroemboli. The best way of shaping these catheters requires advancing them into the aortic arch over a wire (angled Gildewire is recommended). With removal of the wire, the catheter is then flushed. The catheter can then be retracted and the tip positioned in the left subclavian artery. The wire is once again advanced into the catheter and, subsequently, into the left subclavian artery. Further advancing of the catheter (over the wire) will allow the secondary curve of the catheter to climb to the origin of the subclavian. If the wire is removed and the catheter rotated (so that the secondary curve points to the right side of the arch), this allows the catheter to prolapse into the ascending aorta. The catheter can then be manipulated into each specific great vessel. The great vessels can usually be viewed in a lateral or ipsilateral oblique view. The right anterior oblique (RAO) view allows visualization of the origins of the right common carotid, right subclavian, and right and left vertebral arteries. The LAO view allows visualization of the left common carotid and left subclavian and innominate arteries.
MEDICAL THERAPY FOR PATIENTS WITH ATHEROSCLEROSIS ECVD
Hypertension increases the risk of stroke. For each 10-mm Hg increase in blood pressure, the risk of stroke increases by 30% to 45%. Additionally, antihypertensive therapy reduces the risk of stroke. Studies have demonstrated a 33% decreased risk of stroke for each 10-mm Hg reduction in systolic blood pressure to 115/75 mm Hg. Antihypertensive therapy reduces the risk of recurrent stroke by 24% (16, 17, 18). Even patients without hypertension benefit, as demonstrated in the Heart Outcomes Protection Evaluation (HOPE) trial, in which patients with systemic atherosclerosis randomized to treatment with ramipril, displayed a significantly lower risk of stroke than those given a placebo (19).
Tobacco smoking has been associated with extracranial carotid artery intimal disease and the severity of carotid artery stenosis. Smoking increases the relative risk of ischemic stroke by 25% to 50%. Stroke risk decreases substantially within 5 years in those who quit smoking compared with continuing smokers (20, 21, 22).
The relationship between cholesterol and ischemic stroke is not as evident as that between cholesterol and MI. In the MR FIT (Multiple Risk Factor Intervention Trial), the relative risk of death increased progressively with increase of serum cholesterol. In the Framingham Heart Study (24), the relative risk of carotid artery stenosis >25% was ˜1.1 for every 10-mg/dL increase in total cholesterol (25). The Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) prospectively compared the effect of atorvastatin (80 mg daily) with placebo on the risk of stroke among patients with recent stroke or TIA. Statin therapy reduced the absolute risk of stroke at 5 years by 2.2%, the relative risk of all stroke by 16%, and the relative risk of ischemic stroke by 22% (26).
Diet, exercise, and glucose-lowering drugs can be useful for patients with diabetes mellitus and atherosclerotic ECVD. However, the stroke prevention benefit of intensive glucose-lowering therapy to a glycosylated hemoglobin A1C level less than 7.0% has not been proven or established (27, 28).
Antiplatelet medications are a critical component of primary stroke prevention. These drugs reduce the risk of stroke compared with placebo in patients with TIA or previous stroke. However, this has not been demonstrated in asymptomatic patients with ECVD. In secondary prevention, aspirin reduces the risk of future strokes by 15% to 25% (29, 30). High-dose aspirin provided no more benefit than lower doses (160-325 mg daily), but was associated with more side effects. Clopidogrel for Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance (CHARISMA) trial included over 4,300 patients with a prior TIA or stroke, and found that aspirin, 75-162 mg daily, was as effective as aspirin plus clopidogrel in preventing future MI, stroke, or cardiovascular death (31). Current ACCF/ASA/AHA guidelines recommend that all patients with carotid atherosclerosis be placed on antiplatelet medications. Aspirin, 50-325 mg daily, aspirin-dipyridamole, or clopidogrel should be initiated for secondary prevention of stroke. The combination of aspirin and dipyridamole is recommended over aspirin alone, and preferred over the combination of aspirin and clopidogrel (13).
The use of clopidogrel in combination with aspirin is NOT recommended within 3 months after stroke or TIA. In addition, anticoagulation with unfractionated heparin or low-molecular-weight heparin is NOT recommended for patients with ECVD atherosclerosis who develop transient cerebral ischemia or acute ischemic stroke (13).
CAROTID REVASCULARIZATION
Current ACCF/ASA/AHA guidelines suggest that patients with average or low surgical risk who experience nondisabling ischemic stroke or transient cerebral ischemic symptoms within 6 months (symptomatic patients) should undergo carotid endarterectomy (CEA) if the diameter of the ipsilateral ICA is reduced more than 70% (via noninvasive testing) or more than 50% via catheter angiography; and if the anticipated rate of perioperative stroke or mortality is less than 6%.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree