Extended Transsternal Thymectomy
Akira Masaoka
At Osaka University, transsternal thymectomy through an upper sternal splitting approach had been performed from 1962 to 1970. Thereafter, stimulated by the reports from the Mt. Sinai group,28 transcervical thymectomies were performed in 19 patients with myasthenia gravis (MG) from 1971 to March 1973. However, I and my associates found that these patients obtained less benefit postoperatively than those who were treated by transsternal thymectomies performed before 1970. We, therefore, thought that these results might be caused by incomplete removal of the thymus. We had noticed that the boundaries of the upper part of the thymus were clear but those of the lower part were obscure, buried in anterior mediastinal fatty tissue. Therefore, we began an investigation to establish the definitive boundaries of the thymus. Thus, en bloc resections of the thymus including the surrounding fatty tissue in the anterior mediastinum were performed via the sternal splitting approach extending to the fifth intercostal level in 18 patients. The resected specimens were separated into samples of intracapsular thymus gland and extracapsular adipose tissue, and the latter were examined microscopically to determine whether histologic thymic tissue was present. Surprisingly, Masaoka and colleagues18 found that in 13 of 18 cases (72.2%), microscopic thymic tissue was present in the gross adipose tissue. These findings led to the assertion that not only the thymus gland but also the adipose tissue of the anterior mediastinum contains microscopic thymic tissue and that, therefore, the adipose tissue should be resected together with the thymus in order to extirpate all of the thymic tissue. Thus, I and Monden20 concluded that a procedure to remove the thymus and the surrounding adipose tissue would be more adequate in the treatment of MG, and the procedure was called an extended thymectomy.
Rationale for Extended Thymectomy
Investigation by Masaoka and colleagues18 has shown that thymic tissue is scattered in the surrounding adipose tissue around the thymus in excess of 72% of cases. However, the origin of this tissue is obscure. The descent of the thymus gland from the neck to the thorax in its embryonal developmental course might be responsible for such ectopic thymic tissue, and the highly frequent presence of thymic tissue in the gross adipose tissue of the anterior mediastinum is the rationale for extended thymectomy. It is important to stress that to remove the thymus and the surrounding adipose tissue totally, extended thymectomy should be performed transsternally, not by a cervical approach. The transsternal approach permits good exposure, safe manipulation, and complete resection of the entire thymus and parathymic fat. This procedure is now among the most common forms of thymectomy. Aggressive transsternal thymectomy, as suggested by Fischer and coworkers,5 and the radical transsternal thymectomy advocated by Hatton8 and Roth33 and their associates are synonymous with extended thymectomy.
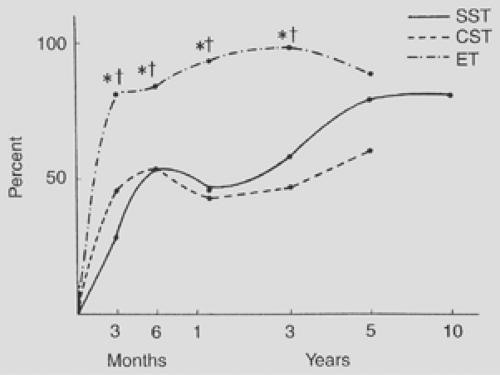
In order to determine whether this procedure could be meaningful in the treatment of MG, the superiority of its results to those of other procedures would have to be proved. At Osaka University, three different procedures for MG had been performed until 1980: (a) transsternal simple thymectomy (removal of the intracapsular thymus only through a transsternal approach), from 1962 to 1970; (b) transcervical simple thymectomy (removal of the intracapsular thymus through a transcervical approach), from 1971 to March 1973, as described by the Mt. Sinai group 28; and (c) extended thymectomy, from April 1973 to 1980. In 1982, the results of these three procedures in the nonthymomatous MG patients were investigated and compared. The effects of thymectomy were evaluated at 3 months, 6 months, 1 year, 3 years, 5 years, and 10 years postoperatively, according to specific criteria: (a) remission—no symptom without medication; (b) improvement—increased activity with less medication; (c) no clinical change; (d) more medication and/or worse symptoms; and (e) death caused by MG. Remission rate (RR) and palliation rate (PR) were calculated according to the following formulas: RR = number of remissions (criteria a)/total number patients, PR = number of remissions and improvements (criteria a+b)/total number patients. Total number is defined as the total number of patients for whom information about clinical status at each follow-up visit was obtained. A is the number of patients defined by criterion (a) and B is the number of patients defined by criterion (b), as defined previously.
Remission rate curves and PR curves of transsternal simple thymectomy (23 cases), transcervical simple thymectomy (19 cases), and extended transsternal thymectomy (95 cases) in the nonthymomatous patients with MG are shown in Figures 185-1 and 185-2. The RRs of transsternal simple thymectomy and extended thymectomy at 3- and 5-year follow-up exceeded those of transcervical simple thymectomy. On the other hand, the PRs of extended thymectomy at 3-month, 6-month, 1-year, and
3-year follow-up exceeded those of transsternal simple thymectomy and transcervical simple thymectomy.
3-year follow-up exceeded those of transsternal simple thymectomy and transcervical simple thymectomy.
Thus, the author and Monden20 concluded that the results of extended thymectomy are superior to those of transsternal simple thymectomy and transcervical simple thymectomy. This conclusion includes three separate statements: (a) extended thymectomy is superior to transcervical simple thymectomy, (b) extended thymectomy is superior to transsternal simple thymectomy, and (c) transsternal simple thymectomy is superior to transcervical simple thymectomy.
Matell and colleagues22 reported that in their institute the procedure of thymectomy changed from simple transsternal (46 cases) to simple transcervical thymectomy (95 cases). The follow-up results in both groups revealed that 77% of the patients in the transsternal group showed improvement, but only 39% in the transcervical group did so.
Disappointed with the results of the transcervical simple thymectomies, Maggi and coworkers17 changed to a combined transcervical and transsternal approach and reported the results in 622 cases. The transcervical/transsternal approach consisted of a transverse cervical incision with upper sternal splitting of 8 to 10 cm in length aimed at removal of all of the anterior mediastinal adipose tissue. Venuta and coworkers37 from Rome (232 cases) and Levasseur15 from Paris (720 cases) adopted a similar procedure instead of the transcervical simple thymectomy. Mulder and associates23 from Los Angeles (333 cases) changed their procedure of choice from the transsternal simple thymectomy to the extended thymectomy. Likewise, Evoli and coworkers4 from Rome (247 cases) adopted the extended thymectomy with an upper sternal split method instead of a transcervical thymectomy. However, these researchers did not compare the results of the former and the latter procedures. Chen and colleagues2 adopted an anterosuperior cervicomediastinal resection technique, but no hard data were presented.
Recently, Zielinski and colleagues38 reported a comparison of results of the basic thymectomies (transsternal simple thymectomies) and the extended thymectomies. The former (n = 58) were performed in 1996 through 1997, and the latter (n = 60) in 1998 through 1999. The RRs of the former were 8.3% (1 year), 11.7% (2 years), 15.0% (3 years), 16.7% (4 years) and 20.0% (5 years); those of the latter were 29.3% (1 year), 37.9% (2 years), 41.4% (3 years) and 46.6% (4 years).
Additional evidence suggesting the superiority of the extended thymectomy is the effect of this procedure in patients who were not benefited by a transcervical or transsternal simple thymectomy. In 1982, the author and colleagues reported on six patients who underwent reoperation by extended thymectomy after previous transcervical thymectomy. We20 found residual thymic tissue situated below the left brachiocephalic vein (average weight 19 g) in all six patients. This suggests technical shortcomings in transcervical thymectomy (i.e., limited exposure, difficulty of manipulation, and incompleteness of removal). Postoperatively, four of the six patients had good results. Henze and colleagues9 reported the largest series of failed transcervical thymectomies. Twenty of 95 patients (27%) who had undergone a thymectomy by the transcervical approach underwent reoperation by an extended transsternal procedure. In 18 of these, thymic tissue was found, and overall 19 patients improved. Rosenberg and associates32 reoperated on 13 transcervically thymectomized patients and found residual thymic tissue in 11. Six of the nine patients who were later followed up had improved. These findings further justify the use of the extended thymectomy. Thus, many surgeons have adopted the extended thymectomy, the rationale of the procedure being accepted by many general thoracic surgeons and neurologists.
Various other procedures were developed following the introduction of the extended thymectomy. One of these new procedures was developed by Jaretzki and Wolff11 and was aimed at enlarging the extent of removed adipose tissue both in the
thorax and in the cervical area adjacent to the thyroid gland. These researchers found thymic tissue to be present in the adipose tissue in the neck and in the deep mediastinum beyond the extent of excision of the adipose tissue by the extended thymectomy, and advocated a “maximal thymectomy” to remove all of the adipose tissue in those regions. Other procedures were developed to perform the extended thymectomy under a minimally invasive method, that is: (a) a transcervical approach with specific sternal retractor, (b) a transcervical approach with upper sternal split, and (c) video-assisted thoracoscopic surgery (VATS) thymectomy. Advantages and disadvantages of these procedures, as well as the extended transsternal thymectomy, have been discussed by Jaretzki and coworkers.13
thorax and in the cervical area adjacent to the thyroid gland. These researchers found thymic tissue to be present in the adipose tissue in the neck and in the deep mediastinum beyond the extent of excision of the adipose tissue by the extended thymectomy, and advocated a “maximal thymectomy” to remove all of the adipose tissue in those regions. Other procedures were developed to perform the extended thymectomy under a minimally invasive method, that is: (a) a transcervical approach with specific sternal retractor, (b) a transcervical approach with upper sternal split, and (c) video-assisted thoracoscopic surgery (VATS) thymectomy. Advantages and disadvantages of these procedures, as well as the extended transsternal thymectomy, have been discussed by Jaretzki and coworkers.13
Recently, Shiono and colleagues35 reported a national survey on thymectomy procedures for MG in Japan. In 2004, a total of 241 thymectomies were performed in 100 institutes; these consisted of 164 transsternal extended and 75 endoscopic thymectomies. In two cases, endoscopic procedures were performed initially but were altered to the transsternal method owing to technical difficulties. Of 100 institutes, 50 adopted transsternal extended thymectomy and 18 endoscopic surgery as a principle; 32 institutes adopted transsternal extended thymectomy as a principle but sometimes performed the endoscopic surgery by patient’s demand.
Technique of Extended Transsternal Thymectomy
The extended transsternal thymectomy is defined as a procedure to remove the thymus and its surrounding adipose tissue in the anterior mediastinum by sternal splitting. However, the operation has many variations or modifications in its technical detail. I will describe my usual procedure in detail and add some modifications performed by other surgeons.
The patient, in a supine position under induction with thiopental sodium, is intubated with an endotracheal single-lumen tube. Muscle relaxants are avoided because some patients with MG are hypersensitive to these drugs. After intubation, a small pillow is inserted behind the shoulders to extend the neck somewhat posteriorly. A longitudinal skin incision is made from the level of the upper edge of the manubrium sterni to the level of the lower end of the corpus sterni (Fig. 185-3). It is possible to shorten the length of the skin incision somewhat by a wide subcutaneous dissection. Mulder24 recommends a submammary wavy transverse skin incision in most women for cosmetic reasons. Budde and colleagues1 recommended a T-shaped skin incision to eliminate the upper part of the longitudinal incision.
After the chosen skin incision, the sternum is split with a sternal saw. I prefer to split the sternum from the manubrium to the fifth intercostal level; the remaining 1-cm-long portion of the sternal body is left intact (Fig. 185-4). This split can allow a successful extended thymectomy and serves to keep the postoperative form of the sternum. Some surgeons, such as Mulder24 and Mussi and associates,25 use a complete sternal split, but I do not use it except in when a thymoma is located at the lower pole. I think the sternal split to the fifth intercostal level is enough in nonthymomatous patients with MG. On the other hand, some surgeons decrease the length of the sternal split. Cohn3 and Pego-Fernandes31 and their coworkers adopt a short sternal split to the fourth intercostal level. Grandjean and associates7 contend that a reversed-T upper ministernotomy is a less invasive method.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree