INDICATIONS/CONTRAINDICATIONS
Until recently, the use of cardiopulmonary bypass (CPB) during the resection of advanced thoracic malignancies was highly controversial. Although technical advances have considerably improved the safety of CPB, the poor prognosis of advanced thoracic malignancies may suggest an unfavorable risk/benefit ratio. CPB adversely affects hemostasis and lung function and has been hypothesized to induce hematogenous tumor dissemination. Finally, some surgeons may lack the knowledge needed to manage CPB during extensive thoracic resections.
Complete en bloc resection remains the best means of improving survival in patients with thoracic malignancies. However, complete en bloc resection is difficult to achieve in tumors, invading the great vessels or heart, which are, therefore, often considered inoperable. This view has been challenged in recent years by reports of excellent outcomes after the surgical resection of primary cardiac tumors under CPB. As a result, some thoracic surgeons are reconsidering the use of CPB in oncologic thoracic surgery. A few recently published small case series studies support the technical feasibility of this approach and suggest that it can provide excellent long-term outcomes.
Indications
The use of CPB during surgical resection of thoracic malignancies should be considered only in carefully selected patients after a multidisciplinary evaluation and discussion of all treatment options. The multidisciplinary team should include skilled thoracic surgeons (trained in the use of CPB and in vascular surgery), an oncologist, an anesthesiologist, an intensivist, and a radiologist.
The complexity of the surgical procedure, high risk of morbidity and mortality, and poor prognosis of incompletely resected thoracic tumors require rigorous patient selection. Patients can benefit from these radical procedures only if complete microscopic resection is achieved.
Elective procedures should be performed with curative intent according to the well-established principles of oncologic surgery (en bloc surgery with microscopically tumor-free margins). Under no circumstances should they be performed with palliative intent.
The need for CPB may be related either to the sites of tumor involvement or to intraoperative events. CPB is helpful when the tumor involves the aorta, left atrium/pulmonary veins, pulmonary arteries, and/or right atrium/inferior and superior vena cava (SVC) complex. In this situation, the decision to use CPB is taken preoperatively based on the results of the staging workup then confirmed intraoperatively when the tumor is seen to invade the thoracic aorta (ascending, arch, and descending), left subclavian or innominate artery down to the aortic arch, common pulmonary artery up to its bifurcation, and/or cardiac chambers (left or right atrium). In these situations, the use of the CPB is mandatory to avoid hemodynamic instability or tumor embolization and to allow complete resection with safe margins. Furthermore, in a small subset of patients, intraoperative events require the use of CPB on an emergency basis. These events may consist in injury to the great mediastinal vessels or heart during tumor resection or in difficulties with ventilation or hemodynamic control during the resection of central tumors. CPB may facilitate, or provide the necessary safety net to achieve, complete surgical resection. CPB is an established alternative to ventilation during extended resections; it provides both oxygenation and hemodynamic stability. The main situations requiring emergent CPB use are the resection of thoracic malignancies involving the trachea or carina, during which adequate oxygenation may be difficult to achieve with conventional ventilation; and the resection of large thoracic tumors invading the SVC or responsible for heart and lung compression, which may result in hemodynamic instability, particularly in case of injury to the SVC, inferior vena cava (IVC), or pulmonary artery. CPB, by allowing rapid filling, may restore hemodynamic stability. With CPB, cardiorespiratory function remains stable throughout the surgical procedure and the heart can be retracted to the side as much as needed.
Contraindications
There are two absolute contraindications to the elective surgical resection of extended thoracic malignancies under CPB: A predicted inability to achieve complete resection, and poor general health or severe comorbidities jeopardizing survival even in the event of complete resection. In all other situations, the decision to perform tumor resection with CPB is taken on a case-by-case basis during a multidisciplinary conference. The factors taken into account include the biologic tumor features (aggressiveness, responsiveness to chemotherapy, and resectability), symptoms, and performance status of the patient. For example, aggressive surgery may be warranted in young patients with residual nonseminomatous germ cell tumor (NSGCT) after chemotherapy even those with removable distant metastases but is not appropriate in patients with nonsmall-cell lung cancer (NSCLC) and distant metastases.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
A careful preoperative workup should be performed to predict the likelihood of achieving complete tumor resection with an acceptable level of risk. Both the features of the tumor and the functional status of the patient should be assessed.
Evaluation of the Tumor
Histologic confirmation must be obtained before establishing the treatment plan, except for NSGCTs with increased serum tumor markers. The biopsy can be collected by direct sampling under local or general anesthesia, flexible bronchoscopy, or needle aspiration under computed tomography (CT) or ultrasound guidance. Subsequent investigations depend in large measure on the histologic findings. Investigations obtained routinely to assess local tumor spread include chest roentgenograms; CT angiography of the neck, chest, and abdomen; flexible bronchoscopy; transthoracic echocardiography; and Duplex scanning of the carotid, vertebral, and subclavian arteries on both sides to check patency. In patients with NSCLC, endobronchial ultrasound is now routinely performed to exclude mediastinal lymph node involvement; when this investigation is not available, mediastinoscopy should be performed prior to extended surgery if CT shows one or more mediastinal lymph nodes. In patients with aortic involvement, the workup may benefit from angiography of the aortic arch and supra-aortic trunks and from transesophageal ultrasound to determine whether left subclavian artery involvement extends to the esophageal wall. When the SVC or an innominate vein is involved by the tumor, phlebocavography by simultaneous injection into a forearm vein on both sides can provide invaluable information to the surgeon. Occlusion of both innominate veins contraindicates CPB, as the poor venous drainage carries a high risk of brain edema (Fig. 45.1). Magnetic resonance imaging (MRI) is very helpful to assess invasion of the intervertebral foramen or spine, heart (cardio-MRI), and IVC. Distant tumor spread is evaluated routinely by positron emission tomography-CT, cerebral CT, or MRI. Depending on the symptoms, subsequent investigations may consist of bone scintigraphy, bone MRI, and/or liver ultrasound to look for distant metastases.
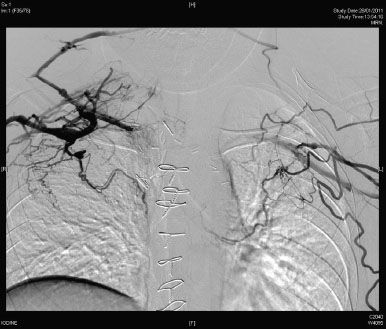
Figure 45.1 Phlebocavography by simultaneous injection into a forearm vein on both sides showing occlusion of both innominate veins.
Evaluation of the Patient’s Functional Status
The functional status of the patient should be assessed before treatment decisions are made. Cardiopulmonary function must be sufficient to allow a long surgical procedure. In addition to the standard preoperative laboratory and respiratory function tests, standard echocardiography should be performed routinely to rule out pulmonary hypertension, left ventricle dysfunction, severe valvular disease, and pericardial effusion. Depending on patient- and tumor-related factors, various other tests may be in order. Coronary angiography should be performed in patients at risk for coronary artery disease. Patients scheduled for pneumonectomy should undergo ventilation/perfusion scanning and right heart catheterization to measure mean pulmonary artery pressure, cardiac output, and pulmonary vascular resistance before and after balloon occlusion of the involved pulmonary artery. This last investigation may show pulmonary hypertension, which precludes surgery. In selected patients, the maximal oxygen uptake can be assessed.
The results of this comprehensive workup allow an assessment of tumor-related factors (local and distant extension, histology, aggressiveness, and availability of active chemotherapy) and patient-related factors (symptom severity and functional status) that serves to establish the surgical indications during a multidisciplinary conference. When designing multimodality treatment regimens, adjuvant treatments (i.e., chemotherapy, radiation therapy, or both) should be preferred over neoadjuvant therapy, which may induce a decline in general health associated with poorer outcomes of the complex surgical procedure. However, neoadjuvant therapy is mandatory in some histologic tumor types such as germ cell tumors and sarcomas.
Planning of the Cardiopulmonary Bypass Technique
Conventional CPB allows cardiac surgery in a motionless and bloodless field. The extracorporeal circuit and membrane oxygenator used to provide physiologic support require full anticoagulation, which may increase the risk of excessive bleeding requiring blood transfusion and, subsequently, of pneumonia following thoracic tumor resection. Conventional CPB must be used when cardiac arrest is required, for instance when the tumor involves the heart, requiring opening of the cardiac chambers, or infiltrates the aortic arch or common pulmonary artery. Conventional CPB may be helpful in highly selected complex cases, by allowing circulatory arrest under deep hypothermia. However, to avoid bleeding-related complications, the use of extracorporeal membrane oxygenation (ECMO) has been suggested. ECMO does not require cardiac arrest. This technique is particularly useful when stabilization of hemodynamics and/or oxygenation is required due to large tumor size, heart-chamber compression, or ventilatory difficulties. ECMO does not require full anticoagulation, as the circuit is heparin coated, and therefore constitutes an attractive alternative to conventional CPB. Intraoperative administration of a single heparin dose of 70 International Unit/kg body weight is usually adequate. The target activated clotting time is 180 to 200 seconds whereas a minimum of 300 seconds is required during conventional CPB. In addition, ECMO is less likely to induce tumor-cell dissemination, as it involves a closed loop with no suction from the operative field and therefore no reintroduction into the general circulation of tumor debris and cytokines. With ECMO, the systemic inflammatory reaction induced by contact of blood with air and artificial surfaces is less marked and the tubing system less cumbersome than with conventional CPB. A venoarterial circuit can be used when hemodynamic stabilization is required or a venovenous circuit when the only concern is the occurrence of ventilatory difficulties, for instance during carinal resection.
Another alternative to conventional CPB for thoracic tumor resection is pumpless interventional lung assist (iLA). The successful use of this technique in two patients was reported recently. The iLA device is a membrane oxygenator allowing CO2 elimination and may, therefore, constitute an alternative to venovenous ECMO.
 SURGERY
SURGERY
Given the small number of patients who undergo extended thoracic tumor resection with CPB, together with the considerable variability in the clinical and anatomical presentations of these tumors, the surgical techniques are not standardized. To achieve en bloc complete microscopic R0 resection, the surgeon must adapt the procedure to the characteristics of the tumor as assessed during the preoperative workup for scheduled surgery or during the operative exploration in emergent surgery. Furthermore, the surgical plan may need to be modified at any time depending on the operative findings. Close cooperation among team members including the surgeon, anesthesiologist, and perfusionist is mandatory.
Patient Positioning and Surgical Approach
The surgical approach is chosen based on the need to achieve complete en bloc resection followed by reconstruction of vital anatomic structures. With the wide possibilities of vascular access as cannulation sites and the different type of arterial and venous cannulas currently available, the use of the CPB is rarely critical for the choice of the surgical approach. For extended thoracic tumor resections, we recommend the routine preparation and inclusion within the operative field of a peripheral cannulation site (femoral or axillary). The most widely used approaches are median sternotomy, posterolateral thoracotomy, and the clamshell incision. Some patients may require median sternolaparotomy, anterior transclavicular thoracotomy, or combined approaches. The most commonly used arterial cannulation sites are the ascending aorta, descending aorta, and femoral artery. Venous access is usually bicaval, atrial, femoral (cannula placed in the right atrium via the femoral vein), pulmonary arterial, and/or intra-abdominal caval.
General Considerations
To decrease the risk of bleeding, the tumor is dissected free from the involved structures as far as possible before the initiation of systemic anticoagulation. In patients with a mobile malignant thrombus, for instance in lung cancer involving the left atrium (Fig. 45.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


