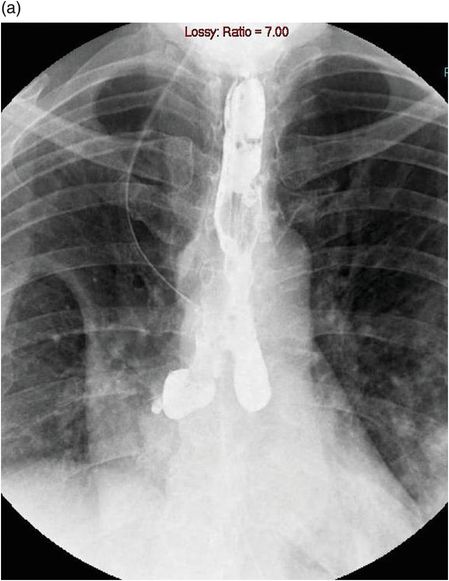
Chest x-ray of a man following a spontaneous perforation of the oesophagus. The left hydropneumothorax has been drained. Surgical emphysema is present and a slight pneumomediastinum can be made out on the right heart border.
Contrast swallow
This remains the most accepted method for the diagnosis of a perforated oesophagus. A positive result clearly indicates the level of perforation as well as the site, side and extent of contamination of the pleural space, enabling planning of any treatment. A normal contrast study does not completely exclude a small perforation. There is a false-negative rate of between 10 and 20%[47]. Non-ionic contrast medium such as gastrografin or gastromyelin is the agent of choice as it is less harmful to the mediastinum. If aspirated, gastrografin can cause a severe necrotizing pneumonitis due to its hypertonicity[47]. It should therefore be avoided in patients at risk of aspiration or with a suspected trache-oesophageal fistula. A contrast swallow has its limitations and is not possible in a ventilated patient.
Computed tomography
This is the method of choice for assessing a perforated oesophagus in the ventilated patient. Computed tomography (CT) is good at assessing the degree of contamination and localizing pleural and mediastinal collections. It also identifies any underlying pathology and eliminates any other serious conditions that may have been in the differential diagnosis (Figures 25.2A, 25.2B, and 25.3).
CT scan following a perorated oesophagus.

surgical emphysema.

hydropneumothorax.
CT scan with oral contrast showing a large perforation of the oesophagus into the left chest.
Endoscopy
In experienced hands, flexible endoscopy provides direct visualization of the perforation and provides details to determine the aetiology of the perforation. Figure 25.4 shows the endoscopic finding in a gentleman suspected of having a spontaneous perforation of the oesophagus. In the emergency setting of assessing a perforated oesophagus secondary to penetrating trauma, it is associated with 100% sensitivity and a specificity of 83%[48]. The role of endoscopy remains controversial due to the worry of further damaging the oesophagus and causing an increase in pneumomediastinum or pneumothorax. Endoscopy does, however, allow for the assessment of any associated pathology in the oesophagus or stomach. It also allows for the assessment as to whether any endoscopic treatment options would be possible.

Endoscopy view showing a tear in the left lateral wall of the oesophagus just above the gastro-oesophageal junction following a spontaneous perforation.
Treatment
Oesophageal perforations represent a heterogeneous group, ranging from an iatrogenic perforation on a normal oesophagus to spontaneous perforations. The location, aetiology of the perforation, degree of mediastinal contamination and time to diagnosis are the most important factors on which to base treatment[4,7,8,49,50].
Cervical oesophageal perforations, because of the containment of the contents within the fascial planes of the neck, tend to incite less of a systemic inflammatory response than thoracic and abdominal perforations. Perforations occurring in these lower areas are not as well contained and thus elicit more of both a local and systemic inflammatory response leading to a compromise in many organ systems, particularly respiratory function, and lead to a higher mortality and morbidity[51].
Perforation of the oesophagus into the thoracic cavity is a potential life-threatening condition and still remains a true surgical emergency.
Initial management
Patients presenting with a perforated oesophagus are often in septic shock, and therefore, initial treatment involves keeping the patient nil by mouth, intravenous antibiotics, anti-fungal agents, reduction of gastric acid production with proton pump inhibitors and fluid resuscitation. If there is a large pleural collection or pneumothorax, then a large-bore chest drain should be inserted. Organ support may be necessary in intensive care.
Non-operative
Most instrumental perforations are small and, if identified early, respond to conservative measures as described earlier. If a decision is made to treat a patient non-operatively, then one has to monitor the patient’s clinical condition closely and be prepared to change the management strategy.
Strict criteria for the non-operative management of oesophageal perforations have been proposed[4,52,53]. Even with these strict criteria for non-operative treatment, 20–54% of patients will develop multiple complications and require operative intervention[4,52].
Operative
Cervical perforations
Due to the reasons described earlier, these perforations are often small and well contained and can be managed by drainage alone.
Intrathoracic and abdominal
The treatment of choice is primary closure. To achieve this, the tissues of the oesophageal wall need to be fairly healthy. The longer the time interval before diagnosis, the less likely this is to be the case. Where possible, the patient should undergo single lung ventilation. A posterolateral thoracotomy is performed. The side and level of the posterolateral thoracotomy will be determined by the information gained from the contrast study. The lung is fully mobilized, and any pleural debris and fluid are removed. The mediastinal pleura is opened. The tear in the oesophagus may not always be obvious. The careful placement of a Maloney bougie pre-operatively may help the identification of it. The upper and lower limits of the tear are identified. The mucosal tear is often longer than the tear in the muscular layer; therefore, one has to open the muscle layer to fully demarcate the upper and lower margins. The mucosa is then approximated using interrupted sutures such as 3-0 Monocryl. The muscle layer is then closed in a similar fashion. Sometimes if the edges of the tear are necrotic, excision is necessary. Also, a single-layer closure may sometimes be possible.
After primary closure, the repair should be buttressed using vascularized tissue. The author’s first choice is a pedicled intercostal muscle flap, which can be harvested at the beginning of the procedure. Other options include diaphragm or pericardium.
An NG tube is passed into the stomach with careful guidance past the repair. Two large-bore 32F drains are inserted, one basal and one adjacent to the repair.
One then has to consider how the patient will be fed; options include total parental nutrition (TPN) or performing a mini-laparotomy and insertion of a feeding jejunostomy.
Post-operative care includes intravenous antibiotics, free drainage and 4-hourly aspirations of NG tube and proton pump inhibitors. Consideration should be given to putting the patient on anti-fungal agents such as fluconazole. The patient is kept nil by mouth (NBM) for 5–7 days when a contrast swallow is performed.
Oesophagectomy
Performing an oesophagectomy for an oesophageal perforation is controversial[51]. If the perforation is an instrumental perforation due to a benign or malignant stricture, then resection may be the treatment of choice. The approach and extent of resection will depend on the site of the pathology.
Saarnio et al. have recently advocated a two-staged repair of oesophageal perforations, with initial oesophageal resection and cervical oesophagostomy and gastrostomy in cases of severe mediastinal sepsis[54]. At a later date, continuity of the upper gastro-intestinal tract is restored with a second operation. Altorjay et al. have presented a series of 27 cases of oesophageal resection with a mortality rate of 3.7%[5]. Proponents of performing an oesophagectomy argue that it provides the best option for controlling the sepsis as there will be no chance of a residual leak. The disadvantages are the need for a second major operation to restore continuity of the gastrointestinal tract and the long-term complications of a stomach tube or colonic interposition.
Endoscopic therapies
Over the last decade, developments in the minimally invasive endoluminal approach in the management of oesophageal perforations include closure of the perforation with clips or sutures, covering the leaks with a covered stent and/or endoluminal drainage of the mediastinal infection.
Endoscopic clips are either deployed through the endoscope or over the scope (Over The Scope Clip [OTSC], Ovesco, Tubingen, Germany). In a systematic review of endoclip closure for oesophageal perforations in 17 patients, through the scope clip was used to close perforations from 3–25 mm. The OTSC is a 12-mm Nitonol clip that fits on the tip of the endoscope. It can be used to close perforations up to 30 mm in diameter. In a multicentre study, all five oesophageal perforations were closed successfully[59].
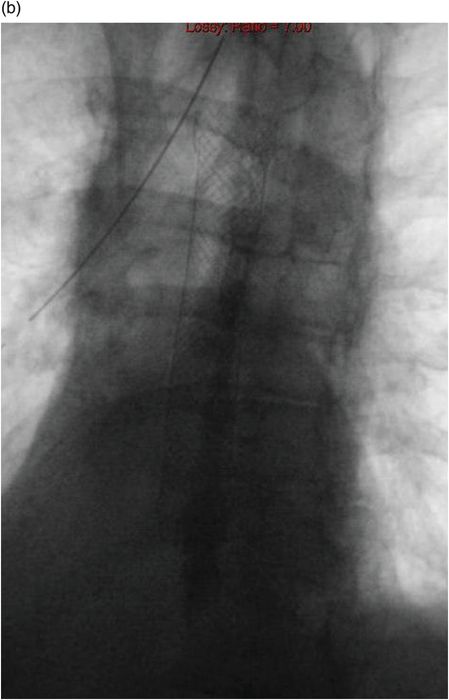
Stents can be used to close oesophageal perforations. Stents may be plastic, covered metal or covered biodegradable material[60]. Dai et al.[61] reported a retrospective series of 41 oesophageal leaks (6 of which were for perforations) treated with covered stents. Complete healing was observed in six leaks with one death. Figures 25.5a and 25.5b show a large oesophageal perforation that was treated with a covered stent.
Contrast swallow showing a large oesophageal perforation into the right chest.

Contrast swallow following placement of a covered stent showed no leak.

Contrast swallow showing a residual leak into the right chest following primary repair of a spontaneous oesophageal perforation into the right chest with intercostal muscle flap.
The residual leak was treated with a covered stent. Contrast swallow following placement of the stent showed no residual leak.
Possible complications of covered stents include stent migration or leakage around the stent. Patients treated with oesophageal stents therefore require close monitoring clinically for signs of sepsis and radiologically for signs of stent migration.
Vacuum-assisted closure is now routinely used to treat many different wounds. The principles behind it are the utilization of suction to remove bacterial contamination, secretions and oedema, thereby promotingthe development of granulation tissue and healing by secondary intention. Endoscopically placed vacuum-assisted therapy has been used to treat oesophageal perforations[62–64]. The device consists of a nasogastric tube with a sponge attached, which is placed endoscopically through the oesophageal defect into the mediastinal cavity. Once the sponge is in the desired position, suction of 75–125 mmHg is applied to the NG tube. The sponge is changed at regular intervals.
Results
In a review of the literature between 1990 and 2003, Brinster et al. found the overall mortality from oesophageal perforation to be 18%[9]. Various factors have been found to affect the mortality rate. These include reason for perforation, underlying pathology, time to diagnosis and method of treatment[4,50,65].
Brinster et al. reported a mortality rate of 36% for spontaneous perforations (range 0–70%), 19% for iatrogenic perforations (range 7–33%) and 7% for traumatic perforations (range 0–33%)[9]. Spontaneous perforations probably have the highest mortality rate due to the high degree of mediastinal contamination and frequent delay in diagnosis. Iatrogenic perforations usually occur following endoscopy and are therefore more easily recognized. The patient usually is starved prior to the procedure, leading to less contamination. Traumatic perforations are often confined to the cervical oesophagus with limited contamination of the mediastinum.
In the same study, cervical oesophageal perforations were associated with a 6% mortality (range 0–16%), thoracic perforations a 27% mortality (range 0 to 44%) and intra-abdominal perforations with a 21% mortality (range 0–43%)[9]. As mentioned previously, cervical leaks are often contained in the neck with limited contamination.
The time interval between perforation and treatment affects mortality and morbidity[7,49,50,66–68]. In their review, Brinster et al. found that a delay in treatment of more than 24 hours was associated with a doubling of mortality[9]. In the past, the first 24 hours have been described as the ‘golden 24 hours’. It was suggested that primary repair should only be performed if less than 24 hours after presentation; after 24 hours, treatment should be more conservative with drainage of pleural collections. However, there are many case series of primary repairs performed after 24 hours with excellent results[7,66–73].
Factors shown to be associated with a poor prognosis include pre-operative respiratory failure requiring mechanical ventilation, malignant perforation, a Charlson co-morbidity index of 7.1 or greater, the presence of a pulmonary co-morbidity and sepsis[51].
The type of treatment of the oesophageal perforation seems to be an important determinant of survival. In their review of the literature containing 726 patients, Brinster et al. found that primary repair had a mortality rate of 12% (range 0–31%), compared with 36% (range 0–40%) for drainage and 17% (range 0–33%) for non-operative management[9]. Careful interpretation of these results is vital, as they are based on case series where significant selection bias would have occurred and the management strategy was individualized for every patient.
After primary repair of intrathoracic perforations, 25–50% of patients have been reported to have a residual leak[51,68,71,73,74]. The majority of these can be managed conservatively, although the author tends to consider placement of a covered stent at 2 weeks post-operatively if there is still a residual leak. Patients treated late are at increased risk of having residual leaks[68].
Although limited data are available on the long-term follow-up of patients who have successfully survived an oesophageal perforation, the outlook is generally good. Three case series provide data on medium- to long-term survival with an average of 3[67], 3.7[75] and 12.5[6] years with survival rates of 90, 88 and 64%, respectively.
Summary
Oesophageal perforation is a surgical emergency that carries a significant mortality and morbidity. Prompt and accurate diagnosis is essential. The management has to be tailored to the individual patient.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


