Risk-adjusted survival for adenocarcinoma according to the 7th edition of the American Joint Committee on Cancer (AJCC)/UICC staging system.
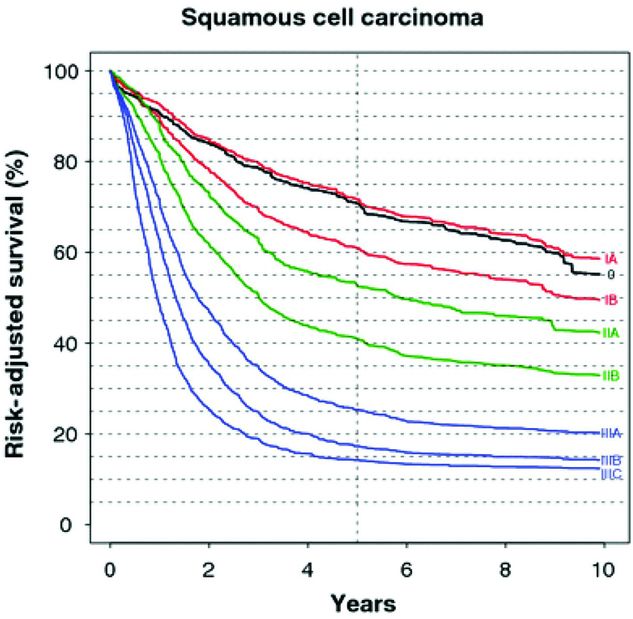
Risk-adjusted survival for squamous cell carcinoma according to the 7th edition of the AJCC/UICC staging system.
It is increasingly recognized that the quality of surgery is important in achieving good outcomes. Surgeons reporting single-center experience with en bloc or modified en bloc esophagectomy report 5-year survivals similar to those achieved in the Cross trial. Although some have argued that good surgery obviates the need for preoperative chemoradiation, the evidence doesn’t support this. Nonetheless, it is incumbent on the surgeon to provide the highest-quality resection possible. This mandates an adequate lymphadenectomy, adequate margins, R0 resection, and reliable and functional reconstruction performed with the least morbidity and mortality.
Surgery has been the mainstay of treatment for those with locoregional disease who are fit enough from a cardiorespiratory perspective. There are a number of surgical approaches. The principles of cancer surgery should be considered when deciding on the operative approach as well as the patient’s comorbidities. The standard approaches by open surgery include Ivor Lewis (laparotomy and right thoracotomy), McKeown (right thoracotomy, laparotomy and left cervicotomy), transhiatal (laparotomy and left cervicotomy), left thoracoabdominal with or without left cervicotomy, and left transdiaphragmatic with or without left cervicotomy. More recently, minimally invasive approaches have developed including either hybrid or fully minimally invasive equivalents of the Ivor Lewis or McKeown approaches.
The choice of operative approach depends on the location of the tumor, patient comorbidities, and surgeon experience. The best surgery is the one that provides the best cancer operation with the lowest morbidity and mortality.
An adequate cancer operation requires an R0 resection: microscopically negative margins. Distally, a margin of 5 cm is appropriate, while the proximal margin should be 7–10 cm in situ. Although a microscopically negative radial margin is desirable, it may be difficult to achieve because of the anatomic relations of the esophagus. Preoperative radiation has been shown to improve the likelihood of a negative radial margin.
An adequate lymph node dissection is essential for both staging and prognosis. It appears that the number of lymph nodes required depends on the T stage. For T1 tumors, 10–16 nodes are required, while for T3 or T4 tumors, 20 or more nodes must be resected. These data are based on patients who were not treated with neoadjuvant therapy. There is no data regarding the number of nodes required for an adequate resection after neoadjuvant therapy.
Tumors of the middle or upper esophagus are best approached using the McKeown approach either open or minimally invasive equivalent. Tumors of the distal third of the esophagus are best approached using Ivor Lewis, thoracoabdominal, McKeown, or minimally invasive equivalent. Tumors of the gastroesophageal junction may be approached by any of the aforementioned approaches as well as the transhiatal approach.
Minimally invasive esophagectomy or transhiatal esophagectomy has both been shown to be associated with reduced pulmonary morbidity. For patients with limited pulmonary reserve, these operative approaches should be considered. For patients with cardiac comorbidity, a transhiatal approach is less desirable.
Although there is some suggestion that transthoracic approaches may offer a survival benefit over transhiatal esophagectomy, both approaches are considered acceptable. Minimally invasive esophagectomy appears to be equivalent to open approaches at least in terms of short-term outcomes and lymph node harvest and is associated with reduced pulmonary morbidity.
Finally, surgeon experience is important. Esophagectomy is one of the complex operative procedures wherein surgeon experience has been shown to have an impact on outcome. The exact operative approach is probably less important.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


