Chapter 29 Epidemiology of Cerebrovascular Disease
Overview
Stroke is the second leading cause of death worldwide, accounting for 4 million deaths in 2004.1 Until recently, stroke ranked as the third leading cause of death in the United States.2 Owing to a reclassification of respiratory diseases using the 10th version of the International Classification of Diseases (ICD-10), preliminary data from the Centers for Disease Control and Prevention (CDC) released on December 9, 2010, ranks cerebrovascular disease as the fourth most common cause of death in the country behind diseases of the heart, cancer, and chronic lower respiratory diseases. On average, every 40 seconds someone in the United States has a stroke, and every 4 minutes someone dies.2 Stroke is also a leading cause of long-term disability in adults. There are a variety of nontreatable and treatable stroke risk factors (Box 29-1).
Stroke Burden
In the United States, an estimated 795,000 persons have a stroke each year, and 7 million individuals 20 years of age or older have had a stroke.2 Ischemic strokes account for 87% of all strokes, with the remaining 13% due to intracranial hemorrhages. About three quarters of these strokes are first cerebrovascular events, and the remainder are recurrent.2 The risk of first ischemic stroke varies by race-ethnicity, increasing from 88 per 100,000 in whites, to 149 per 100,000 in Hispanics/Latinos, to 191 per 100,000 in blacks.2 There were over three quarters of a million hospital discharges for stroke in 2007, and approximately 3.7 million ambulatory care visits attributable to stroke in 2008.3 Up to 70% of cerebrovascular events evaluated in hospitals are ischemic strokes, with 30% due to transient ischemic attacks (TIAs) and hemorrhagic strokes.4 Two thirds of patients hospitalized for stroke are older than age 65; half are older than 70. Importantly, stroke is the second leading cause of death in persons aged 85 and over, who by 2050 will number approximately 20.9 million.5 As measured by disability-adjusted life-years, the burden of stroke relative to other diseases is anticipated to continue to increase worldwide from sixth in 1990 to fourth in 2020.6
A TIA precedes approximately 15% to 23% of ischemic strokes and carries a 90-day stroke risk of 9% to 17%7 and a 25% risk of death over the ensuing year.8 About half of all patients who have a TIA fail to report their symptoms to a healthcare provider.9 With an estimated 240,000 TIAs diagnosed annually in the United States, TIA represents an important target for secondary stroke prevention.
Mortality from stroke accounted for 1 of every 18 deaths in 2007, for a total of 135,952 deaths.2 Mortality in the 5 years after stroke ranges from 27% to 61% across sex-age subgroups.2 Current data on long-term survivorship following ischemic stroke reflects wide ranges of estimated mortality; 13% to 45% at 1 year, 36% to 69% at 5 years, and 31% to 87% at 10 years.10–29 These estimates were primarily obtained from international studies or single regions within the United States and included a relatively small number of cases. Women and minority populations may have higher long-term mortality following stroke, although the evidence is limited, and more research is needed to investigate differences by patient characteristics.13,23,25
In addition to the relatively high mortality from stroke, its aftermath can be devastating. Twenty percent of stroke survivors require institutional care after 3 months, and 15% to 30% are permanently disabled.30 Given the large number of stroke survivors in this country, effective rehabilitation and secondary prevention are important targets for public health intervention.
Cost
Stroke is among the 10 highest contributors to Medicare costs.31 In 2007, the annual cost of stroke in the United States was estimated at $40.9 billion, with $25.2 billion in direct costs.2 Total stroke-related costs were estimated at $68.9 billion in 2009.4 These costs are projected to exceed $2.2 trillion through 2050.32 The mean lifetime cost of ischemic stroke is now estimated at $140,048 in 1999 dollars.33
Regional Patterns of Stroke
Over the last 50 years, stroke mortality has varied regionally in the United States, with the highest mortality rates in the Southeast, a region of the country termed the “Stroke Belt.”34–38 The Stroke Belt is usually defined as including the eight southern states of North Carolina, South Carolina, Georgia, Tennessee, Mississippi, Alabama, Louisiana, and Arkansas. These geographic differences have been documented since at least 1940,34 and despite some minor shifts35 still persist.36–38 The reason for the existence of the Stroke Belt remains uncertain. Within it, a “buckle” region along the coastal plain of North Carolina, South Carolina, and Georgia has been identified with even higher stroke mortality rates than other portions.39 Overall average stroke mortality is about 20% higher in the Stroke Belt than in the rest of the nation and about 40% higher in the stroke buckle. Individuals living in the southeastern United States have a 50% greater risk of dying from a stroke than residents of other regions.39
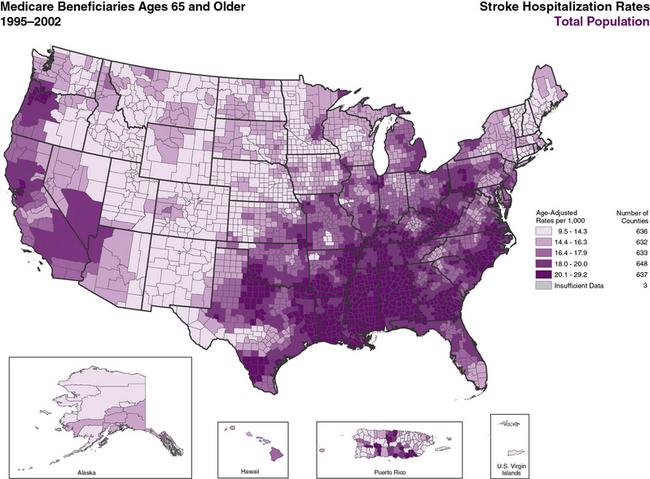
Higher stroke mortality rates are now also noted in the Pacific Northwest.40,41 Overall mortality reflects a combination of incidence and case-fatality rates. Stroke incidence is higher in the Southeast,37,42,43 whereas case-fatality rates vary little across the country.37 The CDC published an atlas showing geographic patterns in age-adjusted stroke hospitalization rates by county that are consistent with stroke mortality patterns (Figure 29-1).44 There are also regional differences in recurrent stroke events within the year after stroke hospitalization, even after adjusting for common risk factors.45,46 Causes for these shifts remain unclear, and contemporary national data are needed to monitor incident and prevalent stroke patterns over time, particularly by age, race-ethnicity, and sex subgroups.
Stroke Risk Factors
Demographic Factors
Age
Stroke is rare in young children, occurring at a rate of 4.6 to 6.4 per 100,000 children in the United States.2 The incidence of stroke in adults is strongly age dependent,25 and the rate of adverse outcomes and complications associated with stroke increases with advanced age.47 The mean age of stroke patients in this country is 70 years. The U.S. population is aging, and by the year 2050, the total number of people aged 65 and older will nearly triple, increasing from 34 million in 2000 to 90 million.5,48,49 This means that by 2050, 20% of the population will be 65 years of age or older and at increased risk for stroke. A report released by the CDC in collaboration with the Center for Medicare & Medicaid Services (CMS), the Atlas of Stroke Hospitalizations Among Medicare Beneficiaries, found that 30-day stroke mortality rates varied by age: 9% in patients aged 65 to 74, 13.1% in those aged 74 to 84, and 23% in those aged 85 or older.44 Because stroke is so strongly age dependent, understanding the epidemiology of stroke in the elderly is critical for both clinicians and policy makers.
Sex
Women are older at stroke onset compared with men (75 years vs. 71 years).2 Overall, women have a lower age-adjusted stroke incidence than men, but sex-related differences in stroke risk are modified by age. Data from the Framingham Heart Study demonstrate that compared with white men, white women 45 to 84 years of age have lower stroke risk than men, but this association is reversed in women older than 85, whose risk is higher than men.2 The absolute number of strokes in the population is, however, greater for women because of the increasing risk of stroke with advancing age, combined with women’s longer life expectancy.
A focus on age-adjusted and age-specific stroke mortality rates conceal the greater total number of stroke deaths in women. The excess deaths in women result from the higher mortality in women and their disproportionate representation in the population. About 55% of all strokes occur in women, who have approximately 60% of stroke-related deaths. Not only do more strokes occur in women, the bulk occur in women over the age of 70, who are more likely to be socially isolated, live alone, have fiscal constraints, and higher rates of comorbid disease. The greater burden of stroke deaths in women is predicted to be even greater in the future, based on population projections; an excess of 32,000 stroke deaths in women in 2000 is anticipated to increase to nearly 68,000 excess deaths by 2050.50
The rate of stroke increases during pregnancy, with the majority occurring during the postpartum period. Pregnancy-related intracerebral hemorrhage (ICH) has the highest mortality and morbidity of all stroke types. Risk factors for stroke in pregnancy include advanced maternal age, African American race-ethnicity, migraines, preeclampsia, and gestational hypertension.51 Meta-analyses summarizing over 30 years of studies show that oral contraceptive users have about a twofold increased risk of stroke compared with non-users; hypertension, cigarette smoking, and migraine headaches further increase stroke risk in women taking oral contraceptives.51 Women younger than 50 are generally considered to be at lower risk for stroke than men, although recent studies show that women aged 35 to 64 were almost three times more likely than men to report prior stroke, largely because of higher rates in 45- to 54-year-olds.52 Prevalence of stroke increases as women reach the menopausal transition. Studies suggest that women are protected by endogenous estrogens, but clinical trials have not found a lower risk of either stroke or cardiac events in postmenopausal women treated with exogenous estrogen and progesterone.50
Race-ethnicity
There are prominent stroke race-ethnic disparities. Blacks and Hispanic/Latinos have two to four times the rate of stroke, stroke recurrence, and stroke-related deaths as whites.53–56 Although differences may be more prominent in younger age groups,57 race-ethnic differences remain among older age groups.56,58 Stroke incidence has been decreasing in U.S. whites, but not in U.S. blacks over the past decade, suggesting a worsening of racial disparity in stroke incidence.59
Lifestyle Factors
Diet/nutrition
Numerous studies implicate dietary factors in the risk for stroke. Aspects of diet that have received attention include individual dietary factors such as omega-3 fatty acids, vitamins C and E, potassium, calcium, fatty acids, homocysteine, and sodium, as well as food groups and dietary patterns such as consumption of fruits and vegetables, the Dietary Approaches to Stop Hypertension (DASH) diet, and the Mediterranean diet.60 Intake of antioxidant vitamin supplements such as vitamin C and E do not lower stroke risk. Although some evidence suggests higher total fat intake increases stroke risk,61 higher fish consumption, a marker for omega-3 fatty acid intake, was associated with reduced stroke risk in the Nurses’ Health Study and the Health Professionals’ Follow-up Study.62,63 Higher fruit and vegetable consumption has been associated with lower stroke risk in many studies64–68 and was found to reduce the risk of stroke in a clinical trial.69 A meta-analysis of cohort studies reported a 26% reduction in stroke risk associated with consumption of five or more servings a day of fruits and vegetables compared with consumption of less than three servings a day.70
Reduced sodium and increased potassium intake have also been associated with decreased stroke risk.71–74 The proposed effects of sodium and potassium on stroke risk are likely in part due to their role in lowering blood pressure. The DASH diet, characterized by high intake of fruits and vegetables, consumption of low-fat dairy products, and low intake of saturated and total fat, effectively lowers blood pressure in clinical trials75 and was associated with an 18% lower risk of stroke in the Nurses’ Health Study (highest quintile vs. lowest quintile).76 The Mediterranean style diet has also received considerable attention with regard to its favorable impact on cardiovascular health. Women in the Nurses’ Health Study at the highest vs. lowest quintiles of the Alternate Mediterranean Diet Score had a lower risk of stroke (relative risk [RR] = 0.87; 95% CI, 0.73-1.02) after 20 years of follow-up.77 Analyses in the same group of women evaluating consumption of a so-called prudent diet (high in vegetable, fruit, legume, fish, and whole grain intake) and a so-called Western diet (one high in red and processed meats, refined grains, sweets, and desserts) found a 58% increased risk of stroke in the highest vs. lowest quintile of a Western diet and a 22% lower risk of stroke in the highest vs. lowest quintile of a prudent diet.78
Current dietary guidelines for stroke prevention recommend reduced sodium intake and increased intake of potassium and fruits and vegetables. Unfortunately, according to national surveys conducted in 2005-2006, average adult consumption ranges from 1.1 to 1.8 servings a day of fruit and 1.2 to 2.1 servings a day of vegetables across race-ethnic groups,4 whereas sodium intake exceeds recommendations for 90% of the adult U.S. population.79 Low fruit and vegetable intake is estimated to account for 9% and 11% of stroke deaths in high-income and mid- to low-income countries, respectively.80
Physical inactivity
Lack of regular physical activity is a well-established predictor of early mortality and cardiovascular disease, and regular exercise is associated with a lower risk of stroke in prospective and case-control studies.81–88 The effects of physical activity are thought to be mediated through reductions in blood pressure, control of other cardiovascular risk factors, improvements in glucose tolerance and body weight, reductions in plasma fibrinogen and platelet activity, and elevations in high-density lipoprotein (HDL) cholesterol concentration.88–94 Current guidelines recommend a minimum of 30 minutes per day of moderate-intensity physical activity most days of the week.95,96 In the 2008 National Health and Nutrition Examination Survey (NHANES), only 32.5% of adults aged 18 and older reported they engaged in regular leisure time physical activity.4 Physical inactivity accounts for 8% and 6% of stroke deaths worldwide in high-income and middle- to low-income countries, respectively.80 Participants in the Physicians’ Health Study engaging in vigorous exercise five or more times per week had a 14% lower risk of stroke compared with those engaging in vigorous activity less than 1 time per week.94 The Framingham Heart Study and the Honolulu Heart Program have found similar effects in men.81,82 Studies in women, including the Nurses’ Health Study and the Copenhagen City Heart Study, also report reductions in stroke incidence with increased physical activity.87,88 Among women aged 45 and older in the Women’s Health Study, higher levels of physical activity (measured in kcal/wk) were associated with a 20% to 40% reduction in stroke risk.97 Finally, in the Northern Manhattan Stroke Study, there was an overal 63% reduction in stroke risk associated with physical activity; this protective effect was found in all subgroups of age, sex, and race-ethnicity (white, black, Hispanic). There is some uncertainty as to the dose and intensity of physical activity required for adequate reduction in stroke risk, and comparison studies are limited. An analysis of the Northern Manhattan Study suggested that heavy physical activity was more beneficial than low to moderate activity.86 Other evidence supports the beneficial effect of light exercise. The intensity of physical activity was not related to stroke risk among participants in the Women’s Health Study, although walking time and pace were inversely related to stroke risk.97
Overweight/obesity
Obesity likely increases stroke risk through multiple mechanisms including increased blood pressure, impaired glucose tolerance, and more frequent atherogenic serum lipid levels. Traditionally, weight categorization has been defined according to the body mass index (BMI; weight [kg] divided by the square of height [m]), with 25 and 30 kg/m2 used as cut-points defining overweight and obesity, respectively. In the Framingham cohort, BMI was related to first cerebrovascular events after adjustment for traditional stroke risk factors.98 Relative risks for stroke in an analysis of women aged 30 to 55 in the Nurses’ Health Study ranged from 1.75 for a BMI of 27 to 28.9 kg/m2 to 2.37 for a BMI above 32 kg/m2, and were independent of other risk factors including age, smoking, hormone use, and menopausal status.99
Obesity was also identified as an independent stroke risk factor in the Honolulu Heart Study.100 Abdominal obesity has emerged as an even stronger risk factor for stroke than BMI. In a study of 28,643 male health professionals, the relative risk of stroke was 2.3 times higher in the upper compared with the lower quintiles of waist-to-hip ratio.101 Obesity is a major public health problem in the United States and worldwide. According to a national survey, 67% of U.S. adults are overweight, and 30% are obese.102 As a population attributable risk factor, obesity accounts for an estimated 20% of stroke deaths in high-income countries and 15% in middle- to low-income countries, a risk that is likely to increase in the United States owing to the epidemic of obesity in the young.
Environmental Factors
Air pollution reflects a heterogenous amalgamation of gases, liquids, and particulate matter that has gained attention as a risk factor for stroke. A 2004 American Heart Association (AHA) Scientific Statement on the relationship between particulate matter (PM) air pollution and cardiovascular disease concluded that both short- and long-term exposure to ambient PM increases the risk of acute cardiovascular events.103 With the proliferation of studies on this topic following this Scientific Statement, an update was published in 2010.104 Indeed, most epidemiological studies have corroborated the initial conclusions, generally reporting an elevated risk of cardiovascular events associated with exposure to fine PM less than 2.5 μm in aerodynamic diameter (PM2.5) for susceptible individuals (e.g., the elderly, those with existing cardiovascular conditions). Recent research also suggests a role for ultrafine particulates less than 0.1 μm, co-pollutants such as ozone and nitrogen oxides, and specific sources of pollution such as motor vehicle traffic.
Among the subcategories of cardiovascular disease, the strength of evidence for an association between air pollution and cerebrovascular disease is less than that for heart disease, but the literature is still growing.104 Among more than 60,000 postmenopausal women initially free of cardiovascular disease in the Women’s Health Initiative, each 10 μm/m3 increase in annual PM2.5 exposure was associated with a 28% increased risk of stroke, a 35% increased risk of stroke or fatal cerebrovascular disease, and an 83% increased risk of fatal cerebrovascular disease.105 There was no association between fatal cerebrovascular and long-term PM2.5 exposure in a cohort of over 300,000 adults derived from the American Cancer Society’s Cancer Prevention Study-II.106 Several studies have reported small but statistically significant associations for short-term pollutant exposure. Daily time-series studies from Korea (Seoul),107,108 China (Shanghai),109 and Finland (Helsinki)110 reported associations between elevated levels of air pollution and stroke mortality; however, the associations were found for ischemic but not hemorrhagic stroke mortality in one study,109 and in the warm but not cold seasons in another.110 A U.S. study of Medicare hospitalizations for stroke or cerebrovascular disease in nine cities found that several measures of air pollution within the 0 to 2 days before hospitalization were associated with ischemic but not hemorrhagic stroke. Additional studies using surveillance data from Dijon, France,111 and Corpus Christi, Texas,112 have also linked certain types of air pollutants with the risk of ischemic stroke and TIA.
In addition to acute cardiovascular events, air pollutants potentially contribute to numerous subclinical physiological changes including systemic inflammation and oxidative stress, coagulation/thrombosis, systemic and pulmonary arterial blood pressure, vascular function, atherosclerosis, heart rate variability, cardiac ischemia and repolarization abnormalities, epigenetic changes, and traditional cardiovascular risk factors.104 Such associations provide further support for a relationship between cardiovascular disease and air pollution and provide insight into plausible mechanistic pathways. As a potentially avoidable risk factor, it may be prudent for those at high risk of cardiovascular disease and stroke to limit outdoor air exposure on high pollution days.
Cigarette smoking
Cigarette smoking is consistently identified as a major independent risk factor for ischemic stroke in epidemiological studies including the Framingham Heart Study,113 Cardiovascular Health Study,114 Honolulu Heart Study,115 and INTERSTROKE,116 among many others. In general, cigarette smoking leads to an approximate twofold increase in stroke risk.117 Smoking is also associated with a two- to fourfold increase in risk of subarachnoid hemorrhage (SAH).118–121 Data are inconclusive regarding a relationship between smoking and the risk of parenchymal ICH. Analyses of data from the Hemorrhagic Stroke Project,122 Physicians’ Health Study,120 and the Women’s Health Study119 find an association between smoking and increased ICH risk, whereas analyses from other studies, including a pooled analysis of data from the Atherosclerosis Risk in Communities (ARIC) Study and the Cardiovascular Health Study, find no relationship.123 One meta-analysis even reported a paradoxical protective effect of smoking for ICH risk,124 although a more contemporary review found an approximate 30% increase in ICH risk associated with smoking.125 Using data from the National Health Interview Survey and death certificates for 2000 to 2004, the CDC estimates that nearly 16,000 cerebrovascular deaths annually can be attributed to smoking, equating to approximately 13% of cerebrovascular deaths for men and 8% for women.126
Environmental tobacco smoke (also known as passive or secondhand smoke) is also thought to increase the risk of stroke for lifelong nonsmokers. A meta-analysis of 24 sex-specific estimates from 15 studies found an overall 25% (95% CI, 16%-36%) increased risk of stroke with current spousal exposure (or its nearest equivalent).127 There was no heterogeneity by sex, publication year, or outcome, but risk estimates tended to be lower for prospective studies and those studies with U.S. or European cohorts. There was not an increased risk for SAH, and overall risk estimates were similar when using ever spousal exposure or total exposure rather than current spousal exposure. A 56% (95% CI, 34%-82%) increased risk of stroke was found for the highest level of spousal exposure.
Although data strongly support a relationship between smoking and stroke, the linearity of a dose effect remains uncertain. A number of studies suggest a nonlinear effect, with the stroke risk attributable to smoking increasing sharply at lower cigarette consumption levels and then leveling off as the number of cigarettes per day increases.128 Similarities between stroke risk estimates and changes in biomarkers of cardiovascular risk for active and passive smokers further support a nonlinear effect of cigarette smoking, suggesting a low overall threshold of tobacco smoke exposure.117,129,130
Clinical and experimental studies indicate both acute and chronic effects of cigarette smoking that likely contribute to increased stroke risk.128 Cigarette smoking causes endothelial injury and dysfunction in both the coronary and peripheral arteries. It increases the risk of thrombus generation in atherosclerotic arteries and creates a chronic state of inflammation associated with development of atherosclerosis. Smoking also leads to an atherogenic lipid profile (increased triglycerides and decreased HDL cholesterol), and it is thought to produce insulin resistance that, along with chronic inflammation, can accelerate macrovascular and microvascular complications such as nephropathy. Smoking even just one cigarette increases heart rate, mean blood pressure, and cardiac index and decreases arterial distensibility.131,132 A number of studies also demonstrate a synergistic action of smoking with other cardiovascular risk factors in increasing stroke risk. Such factors include systolic blood pressure,133 vital exhaustion,134 and oral contraceptives135,136 among others.
Smoking cessation is generally accepted as an essential component of primary and secondary stroke prevention.117 Rapid reduction in stroke risk with smoking cessation is often observed, with considerable reductions apparent within 5 years.124,137–141 Although stroke risk is greatly lower for former compared to current smokers, it remains unclear whether risk ever reverts to that of never smokers. The Framingham Study139 and the Nurses’ Health Study137 show a near-complete loss of excess risk, whereas the Honolulu Heart Program,140 British Regional Heart Study,138 and others124,141 report a slight excess risk for former compared to never smokers. Several studies suggest that this excess risk may be retained for up to 2 decades after quitting.138,141 Heavy smokers may have more sustained excess risk compared with light smokers, whose risk falls more rapidly to the level of nonsmokers.138,141 It is possible that past level of smoking rather than years since cessation or duration of smoking might be the determining factor in achieving risk equivalence.
Alcohol Consumption
The effects of alcohol intake on stroke risk appear to be dependent on both level of consumption and stroke type. In the Honolulu Heart Study, there was a very strong dose-response relationship between alcohol intake and intracranial and subarachnoid hemorrhage.142 Alcohol intake also appears to confer risk for ischemic stroke, although effects at low to moderate levels are less clear, with most evidence suggesting a beneficial effect. A study following male health professionals reported increased risk of stroke with an intake of more than two drinks per day, but no clear association with lower levels of consumption.143 Other studies support a J-shaped relationship between alcohol intake and the risk of ischemic stroke, such that low to moderate levels of intake are associated with reduced stroke risk, and heavy consumption is associated with increasingly higher risk.144–150 A meta-analysis of the effects of alcohol (1 drink defined as 12 g of alcohol) and stroke risk reported a 20% to 28% reduced risk of stroke among those consuming fewer than 1 or 1 to 2 drinks a day relative to abstainers.151 In contrast, heavy drinking (> 5 drinks/day) was associated with a 69% increased risk. The population attributable risk associated with alcohol use for stroke mortality in high-income and middle- and low-income countries is estimated at 11% and 5%, respectively.80 Heavy alcohol use may impact risk through increases in blood pressure, higher rates of atrial fibrillation and coagulation disorders, and reductions in cerebral blood flow. At moderate levels of intake, however, alcohol may have beneficial effects through reductions in platelet aggregation and plasma fibrinogen concentration, and improvements in HDL cholesterol levels and endothelial function. Current guidelines recommend moderate drinking of two or less drinks per day for men and one drink or less per day for nonpregnant women who consume alcohol.152
Medically Treatable Risk Factors
Hypertension
Hypertension, or high blood pressure—defined as systolic blood pressure 140 mmHg or greater, diastolic blood pressure 90 mmHg or greater, or requiring antihypertensive medication—occurs in one in three adults in the United States. Hypertension currently affects more than 76 million people in the country. Prevalence is particularly high in individuals older than 65, in whom it exceeds 67%.153,154 Lifetime risk of hypertension in individuals aged 55 years is 90%. African Americans have one of the highest rates of hypertension in the world; prevalence in this group is 32.3%, compared with 23.0% for whites and 21.5% for Hispanics/Latinos. Despite the relative ease of diagnosis and effectiveness of treatment, approximately 20.4% of adults with hypertension are unaware of their condition, 29.1% are not being treated, and 52.2% do not have adequately controlled blood pressure. Control is lower in Mexican Americans (35.2%) compared with non-Hispanic whites (46.1%) and non- Hispanic blacks (46.5%).2
High blood pressure is one of the most important modifiable risk factors for both ischemic and hemorrhagic stroke. Individuals with blood pressures below 120/80 mmHg have approximately half the lifetime risk of stroke of those with hypertension.4 There is a 38% increased relative risk of stroke for every 10 to 20 mmHg increase in systolic blood pressure, and a 34% increased relative risk for every 5 mmHg increase in diastolic blood pressure.155 This increased risk is a graded response with no apparent threshold, even within the normal range. Lowering blood pressure reduces the incidence of stroke.155
Lifestyle changes can effectively lower blood pressure levels. Adherence to the DASH diet (low in sodium, high in potassium and low-fat dairy) lowers blood pressure.69,75 Weight loss is strongly related with improved blood pressure; a meta-analysis found that a 5.1 kg loss of body weight was associated with an average lowering of systolic blood pressure by 4.4 mmHg and diastolic by 3.6 mmHg.156 Treatment with β-blockers lowers the risk for stroke by 29% (RR = 0.71; 95% CI, 0.59-0.86), and diuretics are estimated to reduce the risk by 51% (RR = 0.49; 95% CI, 0.39-0.62).157 Overall reduction in incident stroke with antihypertensive therapy is estimated at 35% to 44%.158 Recent data suggest that reductions in stroke risk may be related to type of antihypertensive used, based on the agent’s relative effects on blood pressure variability.159
Lipids
A clear linear relationship exists between serum cholesterol levels and coronary heart disease; the relationship between serum cholesterol and stroke is less certain. The totality of evidence from large epidemiological studies suggests, at best, a minimal association between increased total cholesterol levels and stroke risk.117,160 A meta-analysis of 45 prospective cohorts involving 450,000 people and 13,000 incident strokes found no relationship between total cholesterol and stroke.161 The cohorts upon which the analyses were based included many middle-aged participants, and stroke subtypes were not specified. Subsequent studies found a small association between higher total or low-density lipoprotein (LDL) cholesterol levels and increasing ischemic stroke risk; paradoxically, lower total or LDL cholesterol has generally been associated with an increased risk of hemorrhagic stroke.117,160 These differing risks may in part explain the lack of a relationship between cholesterol levels and overall stroke rates.
An individual-data meta-analysis of nearly 900,000 patients from 61 studies worldwide found only a weak positive association between total cholesterol and total stroke mortality at ages 40 to 59, with no association at older ages.162 A weak positive association was also found between total cholesterol and ischemic stroke, with a negative association with hemorrhagic stroke. For both total and ischemic stroke mortality, associations were larger at baseline systolic blood pressure below 145 mmHg.
High-density lipoprotein cholesterol protects against atherosclerosis through reverse cholesterol transport, improvement of endothelial function, and antioxidant, antiinflammatory, and antithrombotic effects.163,164 Numerous large cohort studies have evaluated the relationship between serum HDL cholesterol and stroke risk.164 Despite using different HDL cholesterol cut-points and including cohorts of different ages and geography, most of these studies find either a strong and statistically significant inverse relationship165–169 or a trend towards such a relationship.170,171 The risk of atherosclerotic stroke, in particular, may be most strongly related to low HDL cholesterol levels.172–174 A recent large meta-analysis, however, found no evidence for a significant association between HDL cholesterol and stroke mortality, and only a weak positive association between the ratio of total to HDL cholesterol and stroke mortality for those aged 40 to 69.162 There have been no studies showing that pharmacologically raising HDL cholesterol levels decreases stroke risk.
Findings about the relationship between triglycerides and ischemic stroke are conflicting. Fasting levels were not associated with ischemic stroke in the ARIC and other studies,171 but a meta-analysis of prospective studies in the Asia-Pacific region showed a 50% increase in ischemic stroke risk for those with the highest vs. lowest fasting levels.175 In the Copenhagen City Heart Study176 and the Women’s Health Study,177 higher nonfasting triglycerides were associated with increased risk of ischemic stroke. The Women’s Health Study also evaluated fasting triglycerides and found no association with ischemic stroke.177
Although no large consistent association between cholesterol and total stroke has been observed in epidemiological cohorts, data from randomized trials show that statin therapy reduces risk of stroke among patients with established coronary heart disease and in those at increased vascular risk.178,179 One meta-analysis of data from 14 trials including more than 90,000 patients found an approximate 17% to 21% reduction in the relative risk of incident stroke per mmol/L decrease in LDL cholesterol.178 A significant trend with greater proportional reductions in stroke was associated with greater mean absolute LDL cholesterol reductions. Another meta-analysis including nearly 166,000 participants in trials of statins in combination with other preventive efforts also found an approximate 21% decrease in stroke for each mmol/L decrease in LDL cholesterol.179 Incidence of all strokes was reduced by 18%, and a reduction in the risk of recurrent stroke and major cardiovascular events among persons with noncardioembolic stroke was found, with a trend toward a lower incidence of fatal stroke.
Use of statin therapy to reduce cholesterol did not lead to increased risk of hemorrhagic stroke in primary stroke prevention populations. Among those with prior stroke or TIA, statins may be associated with an increased risk of hemorrhagic stroke that partially attenuates their overall benefit. Other lipid-modification therapies including niacin, fibric acid derivatives, bile acid sequestrants, and ezetimibe also have favorable effects on lipid parameters, but evidence in support of such strategies for stroke prevention is not well established.117
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree