Endovascular Repair of a Popliteal Artery Aneurysm
ELIZABETH ANDRASKA, JOHN RECTENWALD, and PETER K. HENKE
Presentation
A 70-year-old man was referred to the clinic to evaluate a pulsatile mass felt in the left popliteal fossa by his primary care physician. His medical history is significant for hypertension, hyperlipidemia, and coronary artery disease with history of myocardial infarction. He has no family history of aneurysmal disease or coronary artery disease. A duplex ultrasound scan was performed on his femoral and popliteal arteries bilaterally. He was found to have bilateral popliteal artery aneurysms (PAAs) measuring 3 cm on the right and 3.4 cm on the left (Figs. 1 and 2). He was on a beta-blocker, aspirin, and a statin. In clinic, an ankle-brachial index (ABI) was measured to be 1.10 bilaterally, with triphasic pedal waveforms.
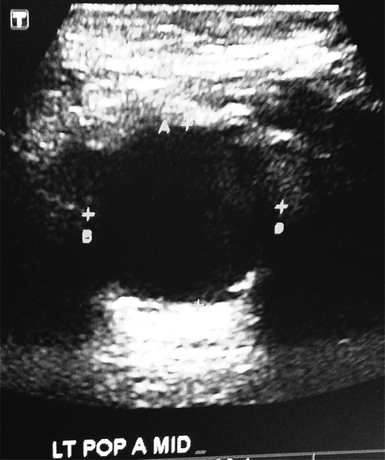
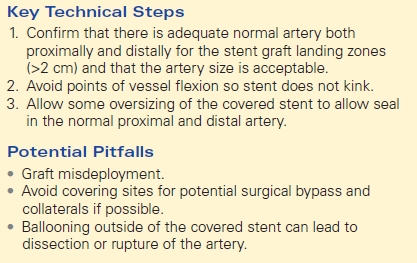
FIGURE 1 Duplex ultrasound image showing left popliteal arterial dilation, consistent with an aneurysm.

FIGURE 2 Duplex ultrasound image with color flow showing blood flow and thrombus in popliteal aneurysm.
Differential Diagnosis
Any mass in the popliteal fossa should prompt a PAA workup. In this patient, the mass was pulsatile, and the ultrasound confirmed PAAs greater than 2 cm bilaterally. The differential diagnosis for a mass in this patient’s popliteal fossa includes a Baker’s cyst, venous thrombosis, hematoma, or neoplasm in addition to a PAA. An ultrasound should be performed to determine the presence of an aneurysm, size of the aneurysm, and presence or absence of intraluminal thrombus. While one third to one half of PAAs are asymptomatic, 20% to 40% present with some form of limb ischemia. Ischemic symptoms include claudication (25%), rest pain, foot ulceration, or acute limb ischemia. Patients may also present with “blue toe syndrome” (4% to 12%), which is caused by repeated thromboemboli from the PAA.
Workup
PAA disease is relatively uncommon in the general population, with an incidence of less than 0.1% in the general population. In patients with a diagnosed abdominal aortic aneurysm (AAA), the incidence of PAA is much higher (approximately 13% to 15%). Patients with PAAs are also at increased risk for other peripheral arterial aneurysms such as an iliac aneurysm (15%) or a femoral aneurysm. As with our patient, it is common for PAAs to occur bilaterally (35% to 48%). If a patient is found to have a PAA, abdominal and peripheral duplex ultrasound should be performed to rule out any synchronous aneurysms. Due to the morbidity of a ruptured AAA, prioritizing interventions in patients with both PAA and AAA is crucial. A large or rapidly growing AAA should be repaired prior to the PAA.
A computed tomography angiography (CTA) should be performed to better define the anatomy of the PAA and to establish inflow and outflow targets in case of surgical intervention. An ABI can be helpful in determining baseline limb perfusion, although it should not be considered a definitive test. If a patient has acute limb ischemia, urgent intervention is necessary due to high long-term amputation rates (9% to 36%). These patients should receive heparin anticoagulation and may be candidates for thrombolytic therapy before any other intervention is considered.
Diagnosis and Treatment
A PAA is defined as a popliteal artery that dilates to 1.5 to 2 times greater in diameter than the normal artery. The incidence of PAA in males as compared to females is extremely high (96%), and risk factors include coronary artery disease, hypertension, cerebrovascular disease, and a history of tobacco use.
Duplex ultrasonography should be used to screen and diagnose the PAA, as well as to evaluate for aneurysm size and presence of thrombus (Fig. Figs. 1 and 2). Duplex ultrasonography with power Doppler technique can be used to evaluate flow through the artery. These studies can also be done postoperatively to evaluate size and flow postrepair. Magnetic resonance angiography (MRA) or CTA can be used to further evaluate the inflow and outflow of a patient’s aneurysm and the surrounding anatomy (Fig. 3). Lower extremity angiography should be performed prior to a PAA repair to evaluate distal arterial runoff in cases where concomitant atherosclerosis exists (e.g., decreased ABI). Vein mapping should be done to determine presence of usable autologous conduit and, if none, may be a reason to repair the PAA via an endovascular technique.
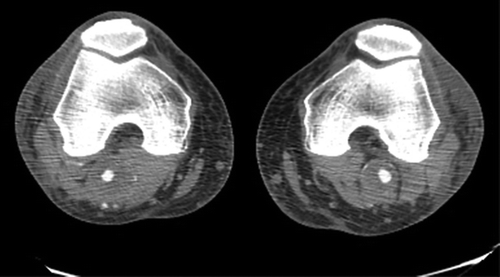
FIGURE 3 Contrast CT scan showing bilateral popliteal aneurysms.
Surgical or endovascular repair of the PAA is indicated in symptomatic patients and in asymptomatic patients with an aneurysm diameter of greater than 2 cm. However, some believe any PAA regardless of size should be repaired. Elective PAA repair for asymptomatic patients has been shown to provide better limb salvage than emergency revascularization due to a thrombosed PAA. While open surgical repair for a PAA remains the gold standard of treatment, endovascular repair has some advantages.
Endovascular repair avoids the morbidity associated with wound and possibly other major operative complications. If the patient is extremely high risk, anticoagulation therapy alone can be considered as an alternative to surgical intervention.
The patient underwent CTA of the abdomen, pelvis, and lower extremities. PAAs were confirmed bilaterally and were both focally confined to the popliteal fossa and with modest thrombus. Neither AAA nor other aneurysms were present. The anatomy of the aneurysm was not tortuous or extensive. Due to the relatively normal anatomy and the patient’s preference, an endovascular repair of the left PAA was elected.
Surgical Approach
Anatomical parameters defined by the preoperative CTA or MRA should confirm that the PAA should not be extensive (e.g., long segment into below-knee popliteal artery) and that adequate landing zones (≥2 cm), both proximal and distal to the aneurysm, are present. The artery diameter between the two landing zones should be relatively similar and range usually 8 to 14 mm. Additionally, the patient must be able to tolerate antiplatelet therapy such as clopidogrel. Endovascular treatment is also a good alternative for patients that do not have adequate autologous conduit for bypass repair. Success rate with endovascular treatment has not been extensively quantified, but a large review estimated the 5-year success rate to be 47% to 75%.
The procedure can be done under general, regional, or local anesthesia. The femoral artery is accessed by ultrasound-guided percutaneous or cutdown technique, per the surgeon’s preference. A floppy followed by stiff guidewire is then threaded in an anterograde fashion, toward the popliteal artery. A nitinol stent lined with polytetrafluoroethylene such as the Viabahn (Gore, AZ) stent graft is slowly deployed along the guidewire, careful not to bend the graft into the aneurysm. Angiography of the aneurysm should be done prior to graft placement to aid in procedural planning and to confirm the proximal and distal landing zones and length of the graft. The diameter of stent graft should be chosen based on measurements taken by CTA and angiogram and should oversize the luminal diameter by 10% to 15%. The deployed graft should exclude the entire aneurysm and extend past the aneurysm endpoint to allow for shortening of the graft. The stent is then sealed both proximally and distally by ballooning within the stent. In this patient, no additional stents were needed. However, for more extensive PAAs, multiple stents may be indicated. In this case, stents should overlap to prevent endoleaks by 2 to 3 cm. The stent placement is then visualized with contrast angiography to check for presence of endoleak. The patient’s knee is then flexed and observed under ultrasound guidance to ensure there is no occlusion due to stent bending. Intravenous heparin is given periprocedurally, based on the patient’s weight, and any operative wounds are closed in the standard fashion (Table 1).
TABLE 1. Key Technical Steps and Potential Pitfalls