Endovascular Management of Innominate Artery Disease
MARTYN KNOWLES and CARLOS H. TIMARAN
Presentation
A 69-year-old male presents with right arm weakness and difficulty performing routine tasks. He also endorses a transient episode of left arm and leg numbness and weakness several weeks ago, and episodes of near-syncope and vertigo. His past medical history includes hypertension, peripheral vascular disease, chronic obstructive pulmonary disease (COPD), diabetes mellitus, and coronary artery disease requiring coronary artery bypass grafting (CABG) 9 years before presentation. He has been a heavy smoker for most of his life. On physical examination, he is neurologically intact and has a right carotid bruit. His blood pressure is 80/54 mm Hg in the right arm and 167/76 mm Hg in the left arm. He has a palpable pulse in the left arm but not in the right. A carotid duplex ultrasound is ordered.
Differential Diagnosis
The differential diagnosis includes stroke or transient ischemic attack (TIA), degenerative joint disease, musculoskeletal disease, thoracic outlet syndrome, occlusive brachiocephalic vessel disease, and vertebrobasilar insufficiency (VBI).
Workup
A complete duplex ultrasound is obtained; no prior study is available for comparison. The ultrasound shows a peak systolic velocity (PSV) of 284 cm/s in the right internal carotid artery (ICA), a PSV of 100 cm/s in the right common carotid artery (CCA), and an end-diastolic velocity (EDV) of 186 cm/s in the ICA, yielding an ICA/CCA ratio of 2.8. The vertebral artery on the right is occluded. On the left, there is a PSV of 103 cm/s in the ICA, a PSV of 54 cm/s in the CCA, and an EDV of 53 cm/s, yielding an ICA/CCA ratio of 0.8. Interpretation: right carotid artery severe stenosis, 80% to 99%; his right vertebral is occluded, left carotid artery mild stenosis, 1% to 49%; the left vertebral is blunted.
A magnetic resonance (MR) angiogram is obtained and reveals severe innominate artery stenosis greater than 90%, left proximal subclavian artery occlusion, left proximal CCA stenosis greater than 90%, and severe right internal carotid stenosis (greater than 70%) just distal to the bulb.
Discussion
The brachiocephalic branches of the aorta include the innominate artery, the left CCA, and the left subclavian artery. Congenital variations are not infrequent and include a bovine arch with a common orifice for the innominate artery and left CCA and an aberrant takeoff of the right subclavian artery. The brachiocephalic arteries, also known as the great vessels, supply the upper extremities and the brain. The great vessels are frequently affected by atherosclerotic disease, which accounts for 70% of cases, which can cause flow-limiting stenoses or embolism. Atherosclerotic disease can cause single or multivessel disease in 60% and 40% of patients, respectively.
Symptoms of severe atherosclerotic disease of the great vessels include stroke, TIA, upper extremity ischemia, and VBI. Single-vessel carotid disease is more likely to cause symptoms of a stroke or TIA. Innominate artery disease can cause stroke, TIA, upper extremity ischemia, or a combination of these symptoms. Occlusion of the proximal subclavian artery can cause a steal syndrome involving the vertebral arteries. VBI is more likely in, but not exclusive of, multivessel disease. Symptoms of VBI include vertigo, diplopia, dizziness, drop attacks, and ataxia. Lesions involving the subclavian or innominate arteries can cause upper extremity claudication, embolism, or distal ischemia. There are other diseases that can cause brachiocephalic disease including giant cell arteritis, Takayasu’s disease, aneurysm, dissection, infections (syphilis and tuberculosis), radiation-induced injury, and trauma.
The diagnostic evaluation of patients with presumed brachiocephalic disease should start with a complete physical examination. Assessment of the upper extremity pulses and blood pressures should be performed and documented. The carotid arteries should be evaluated for bruits. Complete duplex ultrasonography is usually recommended as the initial imaging modality. Careful examination of the carotid, vertebral, and subclavian arteries should be sought. Demonstration of poststenotic flow or reversal of flow should raise suspicion for occlusive disease. Computerized tomography (CT) and MR angiography can provide excellent imaging of the aorta and brachiocephalic vessels and have mostly replaced the need for angiography. Detailed images with 1-mm or finer cuts can accurately be used for careful case planning. Angiography should, however, be used if there is any question of severity or location of disease and for the assessment of flow dynamics or collateral flow (Figs. 1 and 2).
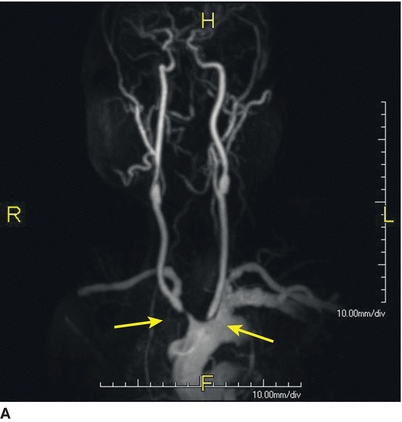
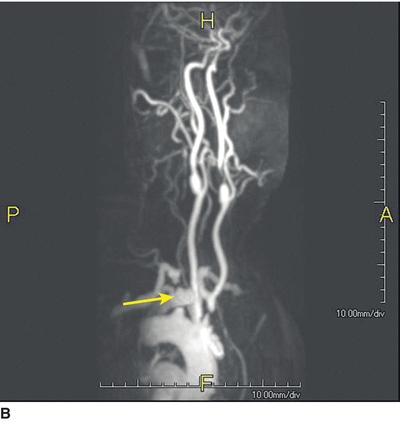
FIGURE 1 MR angiogram showing severe innominate artery stenosis, left subclavian occlusion, and proximal left CCA stenosis. (arrows, lesions in sequential order from left to right).
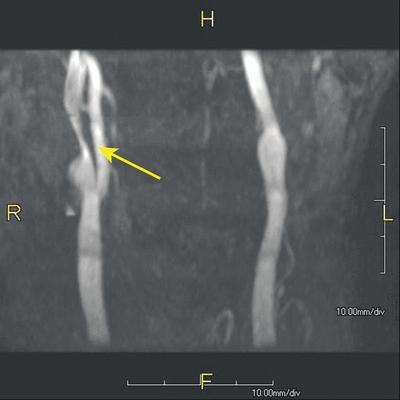
FIGURE 2 MR angiogram showing severe right ICA stenosis just distal to the bifurcation (arrow).
Indications for repair include symptomatic lesions (VBI, stroke, TIA, and upper extremity symptoms). Asymptomatic subclavian-vertebral or subclavian-carotid steal from innominate artery stenosis is not an indication for repair. Severe stenosis of the proximal left subclavian artery, even if asymptomatic, should be pursued if the patient has current or future plans for use of the left internal mammary artery for bypass in CABG (Fig. 3).


FIGURE 3 Intraoperative angiography showing: (A) Severe stenosis of the proximal left CCA and innominate artery, and left subclavian artery occlusion. (B) Severe stenosis of the right ICA distal to the bifurcation.
Diagnosis and Treatment
Diagnosis of severe symptomatic brachiocephalic occlusive disease with severe stenosis of the innominate artery, proximal left CCA, and right ICA requires prompt surgical intervention. Options for brachiocephalic atherosclerotic arterial occlusive disease include both open and endovascular revascularization. In the current case, an endovascular option is sought due to the high morbidity and mortality associated with open surgical revascularization. The patient has severe COPD, history of CABG, and multivessel disease that would require a redo sternotomy (Fig. 4).
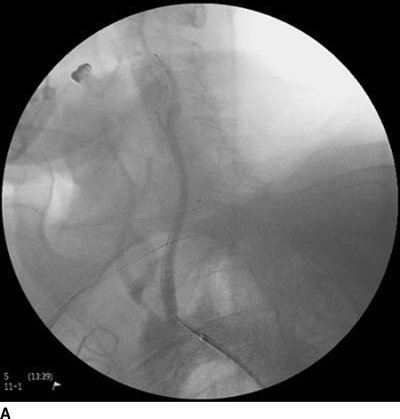

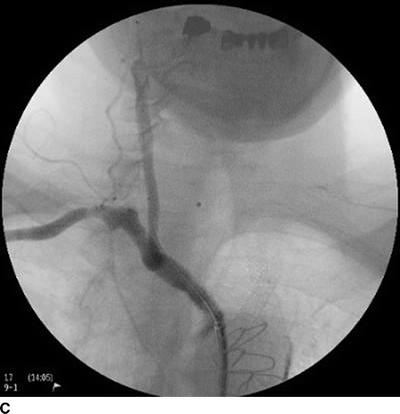
FIGURE 4 Completion angiography following stenting of (A) the left common carotid, (B) right internal carotid and (C) innominate arteries with excellent result and minimal residual stenosis.



