INDICATIONS/CONTRAINDICATIONS
Endoscopic resection is a minimally invasive, organ-preserving technique to endoscopically remove premalignancy or early-stage cancer arising from the gastrointestinal epithelium as a mucosal–submucosal complex. Patients with no risk of lymph node involvement or lower risk for developing lymph node metastasis compared with the risk of mortality from surgery are ideal candidates for endoscopic treatments such as endoscopic resection and ablation therapy. Unlike endoscopic ablation therapy, such as radiofrequency ablation and cryoablation, endoscopic resection can provide specimens for complete histologic assessment including depth of cancer invasion, degree of cellular differentiation, and lymphovascular invasion. Accurate staging based on the histologic assessment is crucial to assess the risk of lymph node involvement and determine whether endoscopic treatment is appropriate for the individual patient. For the purposes of staging, the mucosal and submucosal layers have been subdivided into thirds with each third going deeper into the gastrointestinal wall. As such, T1 tumors have six different layers of invasion: T1m1—m3 (m1 = limited to the epithelial layer, m2 = invades into the lamina propria, m3 = invades into but not through the muscularis mucosa) and T1sm1—sm3 (different thirds of the submucosa) (Fig. 33.1).
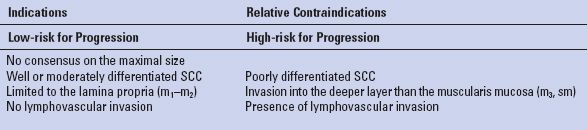
Indications for endoscopic resection for each type of esophageal cancer are summarized in Tables 33.1 and 33.2. For esophageal high-grade dysplasia (HGD) and intramucosal adenocarcinoma, esophagectomy has been recommended as a standard of care based on the fact that HGD is likely to progress to cancer and unexpected cancer is found in approximately 40% of surgically resected specimens obtained from patients with the preoperative diagnosis of only HGD. However, the rate of lymph node involvement is low (<10% for intramucosal cancer) and endoscopic resection can be a good option in some patients to avoid unnecessary, invasive surgery, particularly, in patients with medical comorbidities. It is crucial to differentiate patients at higher risk for progression or for having concomitant invasive cancer with possible lymph node involvement based on the criteria of low- and high-risk factors (Table 33.1). Patients with high-risk for progression will likely be better treated with esophagectomy. Low-risk factors include unifocal (limited or focal) or flat HGD, type I, IIa <2 cm, IIb, IIc <1 cm, well or moderately differentiated adenocarcinoma, mucosal cancer (m) and no lymphovascular invasion. Esophageal squamous cell cancer appears to be biologically more aggressive compared with adenocarcinoma and the risk of lymph node involvement appears higher in patients with squamous cell cancer. Intraepithelial cancers (m1) and cancers invading the lamina propria (m2) are associated with almost no risk of lymph node metastasis. However, the risk of lymph node involvement in cancers invading the muscularis mucosa (m3) and the submucosa ranges from 0% to 10% and 50% to 55%, respectively. Therefore, endoscopic resection can be indicated for superficial well or moderately differentiated squamous cell carcinoma (SCC) limited to the lamina propria (m1–m2). Patients with cancers invading the muscularis mucosa (m3) may be treated endoscopically if there are no further risk factors for lymph node involvement. However, patients with submucosal invasion should be considered for surgery (Table 33.2).

Figure 33.1 Subdivision of early cancers of the gastrointestinal tract based on the depth of invasion. Left panel: Scheme of the gastrointestinal wall. m1, intramucosal cancers; m2, cancer invasion to the lamina propria; m3, cancer invasion into the muscularis mucosa. The submucosa is divided into thirds; sm1, to the upper third; sm2, to the middle third; and sm3, to the lower third. Right panel: The corresponding histologic appearance. (Reproduced from Witteman BP, Foxwell TJ, Monsheimer S, et al. Transoral endoscopic inner layer esophagectomy: management of high-grade dysplasia and superficial cancer with organ preservation. J Gastrointest Surg. 2009;13:2104–2112, with permission.)
Endoscopic resection includes two techniques: Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD). Overall, EMR is commonly used as both a diagnostic as well as a therapeutic tool for the tumor <2 cm in diameter, and ESD is considered for en bloc resection when the diameter of tumors is >2 cm. In any situation, en bloc resection is ideal. Piecemeal resection is acceptable, but is associated with the high rate of metachronous lesions due to incomplete resection and compromised histologic assessment.
TABLE 33.1 Factors to Consider for Endoscopic Resection of High-grade Dysplasia (HGD) and Intramucosal Adenocarcinoma
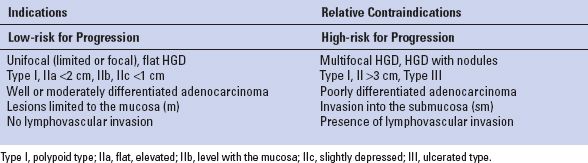
TABLE 33.2 Indications for Endoscopic Resection of Esophageal Squamous Cell Carcinoma (SCC)
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
Accurate endoscopic examination and clinical staging are essential to select patients who are appropriate candidates for endoscopic resection. It is crucial to exclude patients with high risk of lymph node involvement or metastatic disease. Therefore, preoperative work-up should include endoscopic ultrasound (EUS), and positron emission tomography/ computed tomography (PET/CT) to assess lymph node involvement and metastatic disease, in addition to the careful evaluation of extension of the tumor using advanced imaging techniques such as high-resolution endoscopy, chromoendoscopy, or narrow-band imaging. A diagnostic endoscopic resection can be included for staging. The depth of tumor invasion is highly associated with the likelihood of lymph node metastasis.
The role of EUS is to exclude lymph node metastasis and to determine the depth of tumor invasion. It has been shown that EUS can accurately differentiate T1 and T2 tumors but not T1a (m cancer) and T1b (sm cancer) with the current technology. Even the high-frequency miniprobe (20 or 30 MHz) still has a limited accuracy to discriminate between T1a and T1b tumors. Because EUS may not be sufficiently reliable to exclude submucosal invasion in early cancers, the EMR must be diagnostic for this staging purpose. EMR provides specimens for histologic analysis including both mucosa and submucosa, and can reliably determine the T stage of suspicious lesions (i.e., differentiating T1a from T1b). A positive lateral margin can be addressed with further endoscopic intervention, but a positive deep margin should be addressed with surgery. Because PET/CT has been shown to be less accurate than EUS in determining nodal staging but EUS is ineffective in detection of distant metastasis, these modalities should be used in combination during the preoperative work-up. The major role of PET/CT is to confirm the absence of metastatic disease.
Endoscopic resection often requires several sessions. In addition, an intensive follow-up endoscopy is required. Strict acid suppression with high-dose proton pump inhibitors (PPIs) and/or H2 blockade is critical to allow the resected area to heal to normal “neosquamous” epithelium, especially in patients with esophageal HGD or intramucosal adenocarcinoma. These points should be discussed with patients prior to the initiation of treatment.
 SURGERY
SURGERY
Endoscopic resection can be performed under deep sedation using the combination of narcotics and short-acting benzodiazepines in either the GI laboratory or the operating room. ESD often requires a longer time to complete and the general anesthesia in the operating room should be considered. As is typical for endoscopy, the patient is placed in the left lateral decubitus position with the proper monitoring such as cardiogram, blood pressure, and percutaneous oxygen saturation. At the beginning of the procedure, it is important to re-evaluate the extension of the lesions. Placement of an overtube may be useful to keep an easy access to the lesions and facilitate the following procedure.
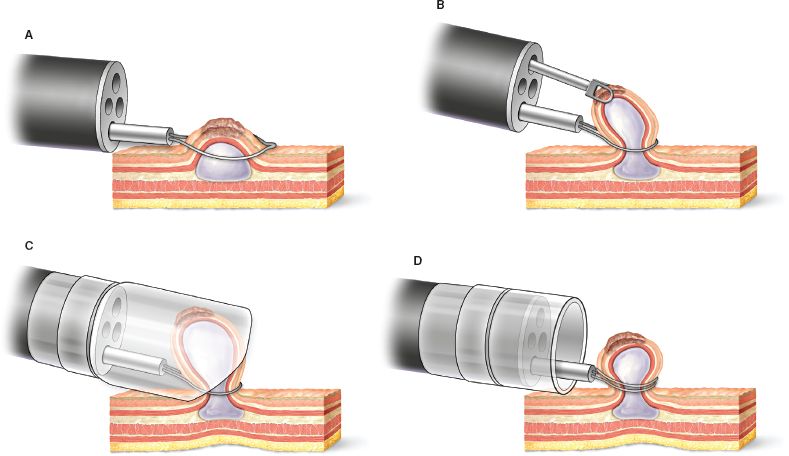
Figure 33.2 Four types of endoscopic mucosal resection (EMR) techniques. A: Snare polypectomy. B: Strip biopsy technique. C: The cap resection technique. D: The ligate-and-cut technique.



